Latest News
-

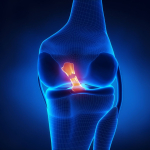
JOINT REPLACEMENT : HOW PHYSIO CAN HELP
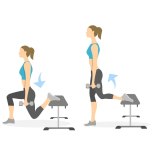
JOINT REPLACEMENT : HOW PHYSIO CAN HELP Joint replacement is a surgery to replace damaged joints with manufactured parts, most commonly performed on the knee or hip when other treatments have failed. Physiotherapy has an important role to play when it comes to preparation and recovery from joint replacement surgery. Read on to find out more. Why are joints replaced? Joints are replaced when they are worn and damaged and it is causing chronic pain and mobility issues. If the issues have not been resolved from other treatments, a partial or complete joint replacement may be recommended by your doctor. Common reasons that knee or hip joints are replaced include: Arthritis (i.e. osteoarthritis, or rheumatoid arthritis) Hip disease since birth (for hip replacements) A serious knee or hip injury Chronic pain that is present even while at rest and that restricts your mobility If you are suffering from chronic pain and mobility issues, joint replacement may be recommended by your doctor to help increase mobility, reduce pain, and improve your quality of life. How physiotherapy can help you to prepare for joint replacement surgery There are many benefits to pre-surgery physiotherapy, whether you are having a knee replaced or a hip (or both!). The right preparation can make a big difference to your recovery. As physiotherapists, we help you to stabilise and strengthen the muscles surrounding the joint. Leading up to your surgery we will set you up with a program of exercises and stretches and show you how to do them with the proper technique. We can also provide guidance on how to modify activities at home to stay mobile before and after surgery. Staying physically active leading up to your surgery is really important and can help to speed up your recovery. In the lead-up to your operation, try to continue with gentle exercise including walking or swimming. It is also a good idea to strengthen your upper body to help with using crutches or walking aids post-surgery. How physiotherapy can help you to recover from joint replacement surgery Physiotherapy is a vital part of recovery and rehabilitation from joint replacement surgery. It’s important to keep moving, but you also need to moderate your activity to make sure you don’t do too much too soon. It will take time for the pain and swelling to subside following your surgery. In the early stages, it’s important to get moving and do exercises to increase circulation and prevent blood clots. The hospital physiotherapist & medical team will have you moving on day 1 and will show you the exercises to do. By the time you leave the hospital, the staff will have shown you how to move, sit, sleep, and use walking aides to get around. They will also show you how to get up and down stairs safely. When you head home, the rehabilitation and hard work continue. Post-surgery physiotherapy aims to reduce pain and inflammation, restore the range of motion in the joint, improve flexibility, strengthen the surrounding muscles and improve the functionality of the joint. It can take 3 to 6 months to recover and return to normal activities (hopefully improved with your new joint!). References: OrthoInfo (2020). Total knee replacement. [Online] Available from: https://orthoinfo.aaos.org/en/treatment/total-knee-replacement/ (Accessed 25 September 2022). NHS (2019). Recovery: knee replacement. [Online] Available from: https://www.nhs.uk/conditions/knee-replacement/recovery/ (Accessed 25 September 2022). Patient Info (2020). Do you need physiotherapy after joint replacement? [Online] Available from: https://patient.info/news-and-features/do-you-need-physiotherapy-after-joint-replacement (Accessed 25 September 2022). Health Direct (2021). Hip replacement. [Online] Available from: https://www.healthdirect.gov.au/hip-replacement (Accessed 25 September 2022). Uploaded : 28 October 2022 Read More -

Work Station Ergonomics
OUR TIPS TO IMPROVE YOUR DESK ERGONOMICS Whether you work in the office, from home, or a combination of the two, the setup of your desk is important for your health and well-being. Keep reading for our important desk tips to help you feel your best while you work. Adjust your monitor Having an incorrect screen setup causes you to strain your neck, which may lead to neck pain. Follow our screen setup tips to reduce the risk of neck strain:● If you are using a laptop, invest in an external monitor that you can adjust to the right height.● Adjust the monitor so that it is an arm's length away, directly in front of you. ● When using two monitors, set them up so that they are centered to avoid overturning your head. ● As a guide, the top of the monitor should be at eye level. Adjust your desk chair Having an adjustable chair is VERY important to your desk setup. When set up properly, it will minimize the risk of experiencing back pain and strain. Follow our chair setup tips: Move the height of your chair so that your elbows are resting at approximately 90 degrees. Your hips should be slightly open. Use a foot support if your feet don’t touch the floor (a step or ream of paper may do the trick if you don’t have a suitable footrest). Use an external keyboard, vertical mouse, and headset Keep key objects that you use often close to your body to avoid reaching or straining for them. Your keyboard should be positioned directly in front of you, about 10cm away from the edge of your desk. Your arms and shoulders should be relaxed to avoid any strain. Make sure your mouse is close to your keyboard to limit shoulder movement. Use a headset or earphones if you are often on the phone to avoid holding it in between your neck and shoulders. Take regular movement and stretch breaks! To reduce the risk of injury and strain, remember to get up and move your body often. Aim to get up at least once every hour. Here are some helpful ways to get moving at work: Set a reminder for a quick stretch every hour Go for a walk Refill your water bottle or glass Take a phone call outside Organise a walking meeting Stretch! References: Safe Work Australia (2020). How do I set up a workstation from home? [Online]. Available at: https://www.safeworkaustralia.gov.au/sites/default/files/2020-05/Working_from_home_Workstation_Setup_%20Guide-COVID-19.pdf Office of Industrial Relations (2012). Ergonomic guide to computer based workstations. [Online]. Available at: https://www.worksafe.qld.gov.au/__data/assets/pdf_file/0013/19102/guide-ergo-comp-workstations.pdf MayoClinic (2021). Office ergonomics: Your how-to guide. [Online]. Available at: https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/office-ergonomics/art-20046169 Uploaded : 28 October 2022 Read More -

Eating Healthy
WHY A HEALTHY DIET IS KEY TO SUCCESS A healthy, balanced diet is key to your well-being. Read on to dive into the many benefits of eating healthy. What does a healthy, balanced diet look like? First things first: what does a healthy diet look like? There is a plethora of information online about healthy eating and it can be overwhelming. We’ve pulled together the important points for you! In summary, a healthy, balanced diet looks like this: Eating a wide variety of healthy foods from each food group daily: fruit, vegetables, grains, protein (including lean meat, poultry, eggs, tofu, nuts, seeds, legumes, beans), and dairy (or alternatives). Limiting your intake of foods that are high in saturated fats, sugar, and salt by only eating them occasionally and in small amounts. Drinking enough water every day. Understanding how much food you need to fuel your body based on your activity levels and eating according to your body’s needs. Get ready for improved sleep There is growing evidence that sufficient intake of key nutrients promotes sleep. A diet lacking key nutrients including calcium and magnesium is associated with sleep problems. A diet that is high in carbohydrates can affect the quality of your sleep. Just as nutrition affects sleep, sleep also changes nutrition, with studies finding that people are more likely to overeat when they don’t get enough sleep. Protection against chronic diseases A balanced diet reduces your risk of developing chronic diseases including heart disease, high blood pressure, type 2 diabetes, and can reduce your risk of developing certain cancers. Key to reaching and maintaining a healthy weight Rates of obesity are growing in adults and children worldwide, with an estimated 1.9 billion adults worldwide being overweight or obese. Maintaining a healthy weight can reduce your risk of chronic disease and also puts less pressure on your joints, muscles, and bones. A balanced diet is essential for reaching and staying at a healthy weight. A good place to start is to learn how much food you need to fuel your body based on your activity levels and make healthy choices by reducing your intake of foods high in saturated fats, sugar and salt. Nutrition plays a key role in mental health There is evidence to suggest a link between your diet and your mood. Studies have found that a diet high in refined sugar is correlated to impaired brain function and a worsening of mood disorders. A healthy diet has been associated with a reduced risk of depression. References: 1. Better Health Channel (2022). Healthy eating and diet. [Onlinehttps://www.betterhealth.vic.gov.au/health/healthyliving/healthy-eating 2. Sleep Foundation (2022). Nutrition and Sleep. [Onlinehttps://www.sleepfoundation.org/nutrition 3. Health Direct (2021). Food, drink and mental health. [Onlinehttps://www.healthdirect.gov.au/food-drink-and-mental-health 4. World Health Organisation (2021). Obesity and Overweight. [Onlinehttps://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight Uploaded : 26 September 2022 Read More -

Lumber Disc Prolapse
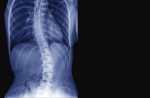
INJURY BLOG: LUMBAR DISC PROLAPSE Did you know that 4 out of 5 people will suffer from lower back pain during their lives? It is a common reason that our patients come to the clinic for physiotherapy treatment. As physios, we want to help to manage your symptoms and improve your quality of life. Read on to find out what causes this condition and how physiotherapy could help. What is a lumbar disc prolapse? Between each vertebra of your spine are spongy, cushion-like discs known as intervertebral discs. These discs provide shock absorption when you run, walk, and jump. They also keep the spine stable, allowing the vertebrae to move. Intervertebral discs have a tough outer shell with a jelly-like centre. The outer shell keeps the jelly in place. Spinal discs withstand lots of pressure and load but sometimes they become damaged and irritated, and the contents push out. This is known as a disc bulge. In the case of a prolapsed disc, the soft centre pushes all the way through. The lumbar spine or lower spine is the area where a prolapsed disc is most likely to occur, making it a common cause of back pain. What are the symptoms of lumbar disc prolapse? The common symptoms of a lumbar disc prolapse include: Inflammation and swelling caused by pressure on the spinal cord Pain that may be persistent, dull and aching, or sharp Numbness, pins and needles, or weakness in one or both legs Tightness that radiates down your glutes and thigh Discomfort that worsens during activity or movement, or when sitting in the same position for extended periods Decreased range of motion and/or stiffness Muscle spasms What causes a lumbar disc prolapse? This condition is commonly caused by natural wear and tear: the amount of water in the discs decreases as we age, and they become less flexible. It is sometimes caused by a traumatic event such as a fall or accident. There are also factors that increase your risk of a lower back injury: Repetitive manual labour and improper lifting techniques increase your risk. It’s important to lift with your legs instead of your back to protect your spine. Being overweight or obese puts more pressure on your spine and increases your risk of injury. A sedentary lifestyle and staying seated for long periods also increase your risk of developing a lower back injury. Can back pain be managed at home? If you’re experiencing mild to moderate muscle strain, you may be able to take some steps at home to manage your symptoms which include relative rest in the early stages, regular gentle movement to promote healing, drinking lots of water and staying off or at least reducing your alcohol intake and smoking habits. How can physiotherapy help? As physios, we are expertly trained to deal with lower back injuries and know when it is necessary to be referred on for further investigations. Most of the time, a disc prolapse can be handled in the clinic. We use a range of passive and active treatment techniques to restore your normal range of motion and function. Initially, we may use techniques such as deep tissue massage, hot and cold therapy, and hydrotherapy to help relieve pain and relax the muscles.As your body heals, we may progress to more active techniques including building core stability, teaching proper stretching techniques to increase flexibility, and muscle strengthening to help prevent future flare-ups. We will work with you at every stage of your recovery and provide advice on how to manage your injury at home. References: 1. OrthoInfo (2018). Herniated Disk in the Lower Back. [Onlinehttps://orthoinfo.aaos.org/en/diseases--conditions/herniated-disk-in-the-lower-back/ (Accessed 19 August 2022). 2. Patient (2020). Prolapsed Disc. [Onlinehttps://patient.info/bones-joints-muscles/back-and-spine-pain/slipped-disc-prolapsed-disc. (Accessed 19 August 2022). 3. Spine Universe (2019). Physical therapy for herniated discs. [Onlinehttps://www.spineuniverse.com/conditions/herniated-disc/physical-therapy-herniated-discs (Accessed 19 August 2022). Uploaded : 26 September 2022 Read More -

Yoga
Have you tried yoga? Are you curious about trying yoga but not sure what it involves? Read on to learn about how it could benefit your life along with physiotherapy. What is yoga? Yoga is a mind and body practice that involves moving into physical poses while combining concentration and deep breathing. It began as a spiritual practice in India over 5000 years ago and has grown in popularity in modern society over the last 50 years. What does a yoga class involve? A typical class includes: Relaxing breathing/introduction to help you focus Warm-up Main flow of postures, movements, stretches Relaxation/meditation to finish Are there different types? There are many different types of yoga to choose from so there is sure to be a style that matches your goals. If you want the benefit of deeper stretches and slow movement then yin or restorative yoga may be for you. If you’re keen to work up a sweat and challenge yourself, you could try a hot yoga class or power yoga. Hatha and Ashtanga are popular all-round styles. Many studios run introductory classes or courses for beginners. Yoga is versatile: you could give it a try at home with an exercise mat and an online class. Be sure to avoid some of the more extreme poses without proper instruction so that you don’t injure yourself. Do I have to be flexible to do yoga? Not flexible? Good news: you’re in the perfect position to benefit from yoga. You don’t need to be flexible to begin. It is a type of mindful movement that allows you to enhance your flexibility. Try not to be put off by comparing yourself to other people. Start at your current ability with the intent of improving your flexibility through regular practice. What are the benefits of a regular yoga practice? Much like physiotherapy, it has many mental and physical health benefits. Research suggests that it may help: Improve flexibility Increase muscle strength Reduce stress, anxiety, and depression Improve sleep Enhance wellbeing and quality of life Yoga is a great low-impact workout that can be adapted to different levels of fitness and ability. Whether you’re returning to exercise from injury, looking to incorporate more strength work, or wanting to enhance your existing fitness routine, it has something for everyone! References: Medical News Today (2021). How does yoga work? [Onlinehttps://www.medicalnewstoday.com/articles/286745 (Accessed 21 July 2022).National Center for Complementary and Integrative Health (2021). Yoga: What you need to know. [Onlinehttps://www.nccih.nih.gov/health/yoga-what-you-need-to-know (Accessed 21 July 2022). Uploaded : 26 September 2022 Read More -

Rib pain
PHYSIOTHERAPY FOR RIB PAIN If you’ve injured your ribs while playing a sport like rugby or football before, you’ll know that it can be both uncomfortable and unpleasant! It’s important to seek proper care to reduce your risk of complications. Read on to find out how physiotherapy could help with your recovery. Anatomy of the rib cage The rib cage, or thoracic cage, is made up of 12 thoracic vertebrae, 12 pairs of ribs (lightweight, curved bones), intercostal muscles, cartilage, and the sternum. The thoracic cage provides stability and support for the upper body, protects vital organs including the lungs and heart, and aids breathing. It also acts as an attachment point for muscles in the upper body. What are the common symptoms of rib pain? Symptoms of rib injuries range from mild discomfort that resolves in several days to severe pain that takes weeks or months to heal. Common symptoms include: a sharp or dull pain in the chest that worsens when breathing in, sore and tender ribs that may be accompanied by bruising, and a popping or cracking sound if a fracture occurs. It’s important to seek emergency medical treatment if you experience severe pain or pressure in the chest and breathing difficulties, as this could indicate a medical emergency, such as a heart attack. What are the common causes? The most common causes of rib pain include: Bruised or strained intercostal muscles Broken or fractured ribs Sports injuries Trauma from motor vehicle accidents or falls Severe coughing during illness Stiffness in spine overloading the thoracic cage Rib subluxation or slipped rib syndrome Osteoporosis (increasing chances of fracture) Inflamed rib cartilage, known as costochondritis (inflammation of the cartilage connecting the rib to the sternum). Can rib pain be managed at home? If you’re experiencing a mild to moderate muscle strain, you may be able to take some steps at home to manage your symptoms. Breathe normally and deeply to clear your lungs and avoid chest infections Use over-the-counter medication to manage the pain, as advised by your Doctor Avoid sports or exercises that aggravate the pain Use ice therapy to reduce any swelling Holding a pillow to your chest for support if you need to cough or sneeze Try to remain upright as much as possible, and prop yourself up to sleep Avoid straining or lifting heavy objects How can physiotherapy help? Physiotherapy aims to restore your normal range of motion and function. It could be an important part of your recovery from a rib injury. Treatment may involve breathing exercises and chest stretches performed slowly and gradually. If you’ve suffered a fracture or cracked rib, make sure you get medical clearance from your GP before commencing exercise. As physios, we work with you to understand the cause of your symptoms and come up with an appropriate plan for treatment. We can show you the proper technique for stretches and exercises to ease your discomfort and promote recovery. We can also provide advice on how to manage your injury at home. see : Thoracic Rings section elsewhere on this site Deep breathing for broken ribs Deep breathing is essential to prevent chest infections or pneumonia. A gentle breathing exercise you can start with is to sit upright in a chair or a bed. Hold a pillow over your chest for support then breathe slowly and deeply until your lungs are full. Try to hold your breath for up to ten seconds, then slowly exhale. Repeat five times, several times a day. References: Physio-pedia (2020). Ribs. [Onlinehttps://www.physio-pedia.com/Ribs (Accessed 20 July 2022).Healthline. (2019). What causes rib pain and how to treat it. [Onlinehttps://www.healthline.com/health/rib-cage-pain (Accessed 20 July 2022).NHS (2021). Broken or bruised ribs. [Onlinehttps://www.nhs.uk/conditions/broken-or-bruised-ribs/ (Accessed 20 July 2022).WebMD (2020). Best exercises for broken ribs recovery. [Onlinehttps://www.webmd.com/a-to-z-guides/best-exercises-broken-ribs-recovery (Accessed 20 July 2022). Uploaded : 26 September 2022 Read More -

The skeletal muscle clock
Skeletal muscle clock disruption by Martin Krause (B Appl Sc Physio; Master Appl Sci Manip Physio, Grad Dip Hlth Sc (Ex and Sp), Grad Cert hlth Sc Edu, Cert IV Workplace Assessment and Training Skeletal muscle contribute to approximately 40% of body mass, Apart from performing work, maintaining posture and providing locomotion, they contribute to systemic physiological and metabolic function, including considerable cross talk with the liver, pancreas, adipose tissue and bone. Disruption of musculoskeletal circadian metabolic function leads to peripheral insulin resistance, glucose intolerance, increased energy expenditure and fasting hypoglycaemia. A review by Erickson ML et al (2021 Ex Sp Sc Reviews 49, 1, 35-41) discussed the diurnal variation of metabolism and substrate preference. Substrate preference has an evolutionary advantage where high carbohydrate utilisation occurs in the morning. with muscles increasing insulin sensitivity, whilst a high fat storage for later oxidation is preferred in the evening. Skeletal muscle oxidative capacity peaks around 2300 and is lowest at 0400 suggesting mitochondrial dynamics rather than biogenesis being the driving factor. Hence, muscles fine tune the expectations of energy expenditure required to perform work. Skeletal muscle clock regulates the myotubule secretion of basal myokines, including Interleukin-6 (IL-6), IL-8 and macrophage stimulating factor - 1 (Perrin L et al 2015, Molecular Metabolism, 4, 11, 834-845). Investigations with Clock mutant mice, have demonstrated reduced GLUT-4 mRNA and protein levels, meaning less ability for muscles to absorb glucose. Circadian rhythms from human donors with various phenotypes appear to demonstrate dampened in metabolic disease. Moreover, metabolic genes under control of Clock show robust rhythmic expression when cultured from lean exercised trained donors, which wasn't observed in donors with type II diabetes (Hansen J et aL 2016, Sci Rep, 6, 35047). Since muscle is responsible for 80% of post insulin release glucose absorption, it is conceivable that skeletal muscle Clock disruption, affects glucose excursions which are the hallmark of type II diabetes. Sleep One night of restless sleep, sleep loss or wakefulness has a significant impact on increases of BMAL1 protein expression, a core component of molecular Clock leading to downstream upregulation of fatty acid uptake and reduced activation of glycolytic pathways (Cedernaes J et al 2018 Sci Adv 4, 8, eaar8590). Circadian mal-alignment studies, reveal metabolic phenotypes of a pre-diabetic state, including increased glucose despite increased insulin, increased mean arterial blood pressure, reduced sleep efficacy and reduced leptin (Scheer FA et al 2009, Proc Nat Acad Sci, USA, 106, 11, 4453-8). Suggestions are, that the skeletal muscle clock orchestrates "sleeping metabolism" even during states of wakefulness. Exercise to reset the skeletal muscle clock In humans, an acute exercise session (both endurance and resistance training), increases skeletal muscle Clock gene expression (Popov DV et al 2018 Biol Sport, 35, 3, 277-89; Zambon AC et al 2003, Genome Biol, 4, 10, R61).Thanks to the paucity of human investigations, it remains to be elucidated whether there is an optimal time to exercise, since carbohydrate metabolic preference seems to be greater in the mornings, this may mean that greater glucose utilization may occur in the morning, resulting in more effective insulin use and/or Glut-4 mediated glucose uptake by skeletal muscle? Yet lipid based metabolism may be more preferred training objective in over weight individuals and hence exercise in the afternoon may be more beneficial? Unfortunately, limited knowledge, on timing of exercise, can be gained from animal studies, as feeding and foraging frequently occur at night. Additionally, the effect of 16:8 fasting diets and morning exercise might also need to be considered. Anecdotally, my clinical observations are that significant weight loss can occur using a morning exercise regime along with 16 hours of fasting. Exercise and weight loss A minimum of 300KCal of energy expenditure every 72 hours is required for weight loss. The greater the calorific expenditure, the greater the weight loss. Conclusion It is plausible and conceivable that skeletal muscles are an organ of circadian rhythm, which have an impact on multiple organs associated with energy expenditure. From an evolutionary perspective, gaining of food was associated with work, which generally occurred during the day. Shifts in metabolic preferences and immune preference suggest an important role of the skeletal muscle Clock. Further investigations are required to fully understand the impact of exercise on people who have poor sleep hygiene, work shifts or fly regularly across multiple time zones. Additionally, the impact of 'timing of exercise' still needs to be elucidated, especially when adding calorific restriction variables such as the 16:8 diet. Uploaded : 10 August 2022 Read More -

Shoulder dislocations
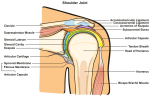
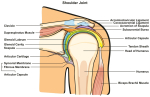
INJURY BLOG: SHOULDER DISLOCATION There is no doubt that dislocating a joint is a painful experience. Whether from a nasty fall, a car accident, or during a game of rugby, the shoulder is easy to dislocate, as it is a very mobile joint. Recovery can take months and after you have done it once, you are more susceptible to it happening again. In this blog, we look at common causes of a dislocated shoulder, and how physiotherapy may help with your recovery. Anatomy of the joint The shoulder is a complex joint that allows for a wide range of motion. It is a ball and socket joint formed where the humerus fits into the shoulder blade/scapula. Think about all the ways that you can move your arms: up, down, side to side, making circles every which way. The complex shoulder joint makes all of this possible. What is a dislocated shoulder? A dislocated shoulder is when the head of the humerus bone pops out of the shoulder socket (ouch!). It can either be partially or completely dislocated depending on whether the bone is all the way out of the socket (double ouch!). What causes a dislocated shoulder? Dislocation is generally caused by a sudden blow to your shoulder. It’s a common sports injury, particular in contact sports such as rugby. Car accidents and falls are also common causes. Hypermobility People suffering with joint hypermobility syndrome (JHS) or Ehlers Danlos Syndrome (EDS) can often spontaneously dislocate their shoulders https://youtu.be/4rj-4TWogFU Symptoms It will usually be fairly obvious if you have dislocated your shoulder because you will not be able to move your arm without being in a lot of pain, and your shoulder will look square instead of round. You may also experience swelling, numbness, weakness and bruising. If you suspect a dislocation, you should seek immediate medical treatment from your doctor or a hospital where you will likely be examined and sent for an X-ray to confirm the dislocation. It is important to have a doctor treat you and put your shoulder back in place to ensure that you don’t damage tissues, nerves and blood vessels. Can physiotherapy help recovery? So, you’ve sought medical treatment and had your shoulder examined and put back into place by a doctor, now what? Once the pain and swelling subsides and the doctor has given the all-clear, rehabilitation can commence. Physical therapy is an important part of recovering from your injury. It will help to restore the normal range of motion in your joint, stabilise and strengthen the surrounding muscles, and prevent the injury from reoccurring. We work with you to come up with an appropriate treatment plan to help you regain strength and restore movement as quickly and safely as possible. In the initial stages, you may feel aches and discomfort as you recover. We can recommend stretches and exercises to ease your discomfort and promote recovery. We can also provide advice on how to manage your injury at home. Preventing the injury from reoccurring As your condition improves, we will change up the program to focus on strengthening and stabilising the joint and surrounding muscles. This is an important part of rehabilitation and recovery and will help to reduce your risk of dislocation in the future. Some additional steps you can take to prevent the injury from reoccurring include:● Wearing padding and protective gear during sports● Taking care to avoid falls● Keeping up exercise to maintain strength and flexibility● Avoiding awkward arm positions References1. NHS. (2020). Dislocated shoulder. [Onlinehttps://www.nhs.uk/conditions/dislocated-shoulder/ (Accessed 24 June 2022). 2. Mayo Clinic (2020). Dislocated shoulder. [Onlinehttps://www.mayoclinic.org/diseases-conditions/dislocated-shoulder/symptoms-causes/syc-20371715 (Accessed 24 June 2022). 3. OrthoInfo (2017). Dislocated shoulder. [Onlinehttps://orthoinfo.aaos.org/en/diseases--conditions/dislocated-shoulder/ (Accessed 24 June 2022). Uploaded : 23 July 2022 Read More -

Physio Myths
Physio myths busted! There are many myths and misconceptions about physiotherapy that can prevent people from seeking treatment to enhance their lives. So, let’s bust some of the common physio myths! Myth: Physiotherapy only helps your muscles People think that physiotherapy only helps with your muscles. It’s true that physio treatment can help if you have pulled a muscle or have an area of muscle weakness that needs strengthening. However, it has many other benefits for your health and wellbeing. Physical therapy can reduce pain and increase mobility if you have stiff joints or are suffering from arthritis, it can also help to strengthen your bones and prevent them from weakening. There are many ways that physiotherapy can help to enhance your well-being and your life. Myth: You only need physiotherapy when you have an injury The belief that you only need physiotherapy when you are injured is a common misconception. As physios, we can help you to recover from injury and promote rehabilitation by developing a program of specific exercises and stretches designed to restore function and strength. However, you don’t have to wait until an injury pops up to come and see us. Prevention is better than cure! If you are putting up with any niggling pain or discomfort in your day-to-day life, come and see us before injury occurs and it becomes a bigger problem. Myth: Only athletes need regular physiotherapy On TV or at sports games, we often see professional athletes or sports teams with a dedicated physiotherapist (or several) on the side-lines ready to assist with injuries. This probably adds to the misconception that regular physiotherapy is only for professional athletes or people into sports and fitness. It’s true that we help sportspeople whether professional or amateur, to improve their strength and fitness or recover from injury. However, everyone can benefit from physiotherapy! We treat a range of patients from all ages and levels of fitness and mobility. Regular physiotherapy can be beneficial if you are suffering from chronic conditions like osteoarthritis or osteoporosis or are experiencing chronic back pain or headaches. Myth: Physiotherapy treatment is just stretches and exercises! Most people think that physiotherapy treatment consists of a list of stretches or exercises to do. Depending on your condition, your treatment will possibly involve a range of exercises and stretches to improve your strength, flexibility and mobility. There is so much more to physio treatment though! We may use techniques such as massage and soft tissue therapy, lifestyle advice, education, training plans, acupuncture and dry needling, joint mobilisation and more! We will take the time to listen to your symptoms and medical history, assess your condition, and develop a treatment plan that is specific to you and your needs. Uploaded : 23 July 2022 Read More -

INJURY BLOG: THORACIC OUTLET SYNDROME
INJURY BLOG: THORACIC OUTLET SYNDROME Have you experienced numbness or weakness in the arm and hands that seem to run from your upper chest all the way down your arm? If you also have trouble lifting objects over your head, thoracic outlet syndrome could be to blame! Today’s blog explains thoracic outlet syndrome, the signs and symptoms, and how it is treated. Before we dive in, let’s talk about what the thoracic outlet is. The thoracic outlet The thoracic outlet is the space between the collarbone and ribs in the lower neck and upper chest area. It’s a narrow space that houses nerves, muscles and blood vessels that pass through from your back to your arms. What is thoracic outlet syndrome and what are the symptoms? Thoracic outlet syndrome is the term used when the thoracic outlet is compressed, irritated or injured. Sometimes the thoracic outlet becomes too narrow and can compress the muscles, nerves, and blood vessels (ouch!). It most commonly affects the nerves but can also affect the veins and arteries. What are the symptoms of thoracic outlet syndrome? The symptoms of thoracic outlet syndrome can include: Pain in the shoulders, neck, arm, or hand. Numbness, pins and needles, or weakness in the hand and arm. Swelling, redness of the hand, arm, or fingers. Arm becomes easily fatigued. Limited range of motion in your arm and shoulder. What causes thoracic outlet syndrome? Common causes of thoracic outlet syndrome include: Physical trauma such as a car accident causing whiplash. Repetitive movements from sports such as baseball, swimming, golfing or volleyball. Manual labour - carrying heavy shoulder loads. Weightlifting. Pregnancy Structural abnormalities (e.g. an extra rib, called a cervical rib). The condition can be aggravated by poor posture, obesity, stress, depression, and sleep disorders. Can physiotherapy help to treat thoracic outlet syndrome? Yes. Physical therapy is a common treatment for thoracic outlet syndrome. As physiotherapists, we will conduct an assessment, talk to you about your symptoms and medical history, and come up with an appropriate treatment plan to help to reduce your symptoms and pain. Initial treatment will focus on: Reducing pain. Increasing the range of motion in the neck and shoulders. Strengthening the muscles around the shoulder to better support the whole area. Exercises to improve your posture to lessen the pressure on the area. Physical therapy can assist with recovery, restoring function and strengthening to get you back to your best. Preventing thoracic outlet syndrome It’s not always possible to avoid thoracic outlet syndrome, however there are steps you can take to reduce the risk of recurrence: Practice good posture when sitting or standing to create space in the thoracic outlet. Try to maintain a healthy weight. Avoid heavy backpacks and shoulder bags. Avoid heavy lifting or activities that make symptoms worse. Stretch and strengthen! We can help you with exercises and to master the correct technique. If you are experiencing the symptoms of thoracic outlet syndrome and need help to manage them, come and see us. We will investigate and come up with an appropriate treatment plan to help improve your quality of life. Give us a call or email us or book online to make an appointment. References: 1. Burke, D. (2021). Thoracic Outlet Syndromes. [Onlinehttps://www.healthline.com/health/thoracic-outlet-syndrome (Accessed 23 April 2022). 2. Cleveland Clinic. (2022). Thoracic Outlet Syndrome. [Onlinehttps://my.clevelandclinic.org/health/diseases/17553-thoracic-outlet-syndrome-tos (Accessed 23 April 2022). 3. Mayo Clinic (2022). Thoracic Outlet Syndrome. [Onlinehttps://www.mayoclinic.org/diseases-conditions/thoracic-outlet-syndrome/symptoms-causes/syc-20353988 (Accessed 23 April 2022). 4. OrthoInfo (2022). Thoracic Outlet Syndrome. [Onlinehttps://orthoinfo.aaos.org/en/diseases--conditions/thoracic-outlet-syndrome (Accessed 23 April 2022). Uploaded : 26 May 2022 Read More -

Frequently Asked Questions
PHYSIOTHERAPY FAQs In this blog, we’re bringing you the answers to questions we’re frequently asked as physiotherapists. Read on to find what we do and how we can help you and your family. What is physiotherapy? Physiotherapy is the use of physical techniques to improve movement, restore function, reduce pain and promote recovery from an injury, illness or disability. Other important facts about physiotherapy: ● It is a government-registered healthcare profession, requiring a university qualification.● As physiotherapists, we work to prevent as well as manage injury, disease, and disability.● We assess and diagnose your condition and develop a treatment plan that is specific to you. What conditions does a physio treat? Physiotherapists assess, diagnose and treat a wide range of conditions including: ● Back and neck pain and stiffness.● Aches, sprains, and strains: from your hands to your hamstrings!● Sports injuries including preventative strengthening and conditioning.● Recovery from fractures - we’ll come up with a treatment plan to help to restore function and promote healing.● Managing diseases including diabetes, osteoarthritis and osteoporosis.● Promoting safe movement.● Rehabilitation after surgery. And so much more… Is physiotherapy suitable for children and adolescents? A physiotherapist can treat people of any age. Some physio’s may choose to specialise in treating newborns or young children (i.e. paediatrics) or women’s health and pregnancy-related conditions. Others may solely work in a sports setting, working closely with a team or club. You will also see physios working within the aged care setting. We are very versatile! What techniques are used in physiotherapy? Depending on your symptoms, some of the treatment methods we may use include:● Exercise programs to build strength and improve mobility.● Massage/soft tissue mobilisation.● Acupuncture and dry needling.● Therapeutic taping.● Joint manipulation and mobilisation.● Hydrotherapy.● Muscle re-education. We develop a treatment plan that is specific to you and your needs. How does physiotherapy help? We can help you to have pain-free movement, restore function and prevent chronic diseases. We aim to help you to get the most out of life! Uploaded : 26 May 2022 Read More -

Hamstring Injuries
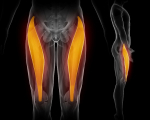
Exercises for hamstrings injuries in sport Hamstrings injuries can take many forms. Acute sporting injuries, in younger individuals, are frequently to the bulk of the muscle belly, whereas more chronic injuries, in older individuals, tend to involve the tendon insertions on the sitting bone. Depending on the type of sport, dynamic sports such as running and kicking tend to involved the contractile apparatus of the muscle, whereas less dynamic sports such as cycling or rock climbing, tend to involving the sitting bones and tendon insertion. Severe traumatic injuries, such as those from water skiing may also involve insertional fractures. Additionally, some sciatic nerve dysfunction from the low back or piriformis can mask as a hamstring injury. Finally, haematomas from a hamstring injury can form around the peripheral sciatic nerve, resulting in sciatic nerve like symptoms. The Hamstrings are made up of four muscles. The Biceps Femoris (outside two muscles), Semitendinosus and Semimembranosus. The biceps can be considered the power mobilisers for bending and extending the knee, whereas the inside two muscles have a greater role in stabilisation, especially of the knee's medial joint complex. The role of musculoskeletal physiotherapy is to make a differential diagnosis. Hereby, ascertaining the appropriate course of treatment and rehabilitation. More can be read elsewhere on the site : Differential Diagnosis of Hamstring Injuries. Exercise regimes should be functional and appropriate to the stage of injury and will often include back-hip and knee exercises as well as the eccentric hamstring programmes promoted by therapists dealing with the latter stages of an injury. Chronic Tendon - sitting bone insertion injuries, should be encouraged to do a lot of gluteal work, to take some of the load off the hamstring as well as enhance the nutrition to the tendon. PRP - involving injections of platelet rich plasma might also be considered and was found to be effective in combination with haematoma aspiration in athletes (Trunz LM et al 2022, Med Sc Sp Ex, 54,1, 12-17). These authors found a significantly shorter return to play and shorter recurrence rate compared with athletes receiving conservative treatment. However, an active recovery program should be an essential part of rehabilitation, as it prepares a framework for the process of recovery, as well as establishes baselines and goals, specific to the stage of injury, which provide a benchmark, as to the rate and extent of recovery, which ultimately determines their return to sport competency. Invasive procedures should be undertaken with care and sometimes it's better 'not to poke the bear'. Uploaded : 28 April 2022 Read More -

Lisfranc Fracture
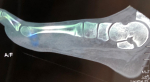
Lisfranc fracture of the foot Lisfranc was a surgeon in the Napoleonic army who first described a unique fracture which occurred when cannons recoiled over a soldiers foot A Lisfranc fracture is one of the most common foot fractures. Dropping something on your foot is a common way to fracture your Lisfranc joint. Two-thirds of Lisfranc injuries happen when something hits your foot directly, with force. This could be in a motor-vehicle accident, a crush injury, or a fall from height. One-third of Lisfranc injuries occur indirectly and are more commonly missed, e.g. during sports or activities like horse riding; from household accidents or twisting your foot when you fall. The latter is often confused with a lateral ankle sprain. What are the symptoms of a Lisfranc injury? Lisfranc injuries range in severity from a mild sprain to a severe fracture. Typically, an injury to the Lisfranc joint or ligament will have the following symptoms:● Swelling in the midfoot.● Pain when trying to bear weight, and pain when walking down stairs.● Bruising to the top and bottom of the foot - bruising on the bottom of your foot indicates you have more likely fractured the bone. How is a Lisfranc injury treated? Treatment will depend on the severity of the Lisfranc injury. For a mild Lisfranc sprain, follow the normal first aid protocols of relative rest, ice, compression and elevation until you are able to see your physio for a thorough assessment. Your physio should then have you back on your feet within weeks. For severe injuries/fractures, you may need a cast or brace or moon boot for up to six weeks. Occasionally surgery is required to pin bones in place or fuse them together. Can physiotherapy help to treat a Lisfranc injury? Yes. We can help you to manage your injury from diagnosis, to treatment and recovery. If a Lisfranc fracture is suspected at the initial assessment, we will send you for an x-ray. If a fracture is confirmed, we can apply an appropriate cast, splint or brace once you’ve been to your doctor, or before you go to see them for review. We will provide you with crutches, if needed. As your fracture heals, we will monitor your progress and make adjustments to your cast or splint. Chronic pain, arthritis or decreased function can occur if the injury is not detected and treated promptly. Physical therapy can assist with recovery, restoring function and strengthening. We will give you a tailored exercise program to help you progress to a full recovery. References: 1. Adcox, M. (2017). Recognizing a Lisfranc Fracture. [Onlinehttps://www.healthline.com/health/lisfranc-fracture (Accessed 23 March 2022). 2. Australian Physiotherapy Association. (2022). Choose physio for Fractures. [Onlinehttps://choose.physio/your-lifestage/ageing-well/fractures (Accessed 23 March 2022). 3. Beahrs, T. and Weatherford, B. M. (2022). Lisfranc (Midfoot) Injury. [Onlinehttps://orthoinfo.aaos.org/en/diseases--conditions/lisfranc-midfoot-injury/ (Accessed 23 March 2022). 4. Whelan, C. (2019). What causes ticklish feet and why some people are more sensitive than others. [Onlinehttps://www.healthline.com/health/ticklish-feet#sensitivity (Accessed 23 March 2022). Uploaded : 27 April 2022 Read More -

Kinesiotape
The low-down on kinesiology tape Have you ever wondered why your physiotherapist is making you all colourful with stretchy tape during your appointment? Read on for some answers! What is kinesiology tape? As physiotherapists, we use a range of treatment methods to help increase your mobility as you recover from an injury, including therapeutic taping. Kinesiology tape (or kinesio tape) is an elastic, therapeutic tape that we use to provide your joint with support, without limiting movement. Originally developed in Japan as long ago as the 1980's, it only became popular in the West in the late 1990's. Why is kinesio tape used? We generally use kinesio tape to help reduce pressure on damaged muscles and joints, increase mobility, lessen pain, and reduce swelling. We also use it to reduce the chances of further damage to an area that is weak from injury. If you are prone to injury in a certain area, taping may also give you some protection. How does it work? During an appointment, we will assess your condition and determine if kinesio tape is necessary, and then work out the best way to apply it. We apply it in a pattern that will help to support your specific injury. Kinesio tape is stretchy and flexible. It’s designed to be elastic like your skin, so that you can move freely when it is applied. When applied, it lifts the layers of skin and tissue, encouraging blood flow. It has roughly 35% elasticity, whereas semi-rigid sports strapping tape is only around 6%. There is also some research to suggest that using kinesio tape changes the signals between your brain and the skin over an injured area. The tape helps to strengthen the signals, increasing connectivity between the area and the brain. Skin sensitivity Kinesiotape seems to be better tolerated, by most skin, than the traditional sport stape. However, people have been known to have allergic reactions, to even this mild adhesive. What about the colour of tape, does that matter? No! We think the different colours look cool though, the brighter the better! However, some people suggest the darker colours absorb more heat and maybe better for areas which are feeling cold Other forms of taping Other forms of taping can be read elsewhere on this site : What we do : Taping and under Patellofemoral Taping or Tape Tape Tape Uploaded : 27 April 2022 Read More -

Muscular System
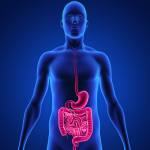
THE MUSCULAR SYSTEM When we think about muscles, we tend to think of fitness, strength training, and toning. While muscles are responsible for moving our bodies, the muscular system also has other important functions in the body. The muscular system The muscular system is made up of three types of muscles: skeletal, cardiac and smooth. Here’s a breakdown of the three muscle types and what they do. Skeletal muscles are attached to bones and create movement. They require conscious or voluntary movement. Skeletal muscles are generally grouped into opposing pairs (e.g. biceps and triceps). The body contains more than 600 skeletal muscles. They are also called striated muscles, since they appear striped. Cardiac muscles are specific to the heart. They create pulsing that pumps blood through the heart and body. Cardiac muscles contract and relax without our conscious awareness, therefore are known as involuntary muscles. Smooth muscles are layered sheets of muscle tissue that line internal organs and vessels and contract in waves. These involuntary muscles are responsible for propelling things throughout the organs e.g. food through the digestive tract; urine through the bladder. Muscle health and nutrition Healthy muscles need exercise and proper nutrition. Muscle tissue requires protein, glucose from carbohydrates, electrolytes and minerals such as calcium, magnesium, potassium and sodium to function. A very strong interaction occurs with the immune system of the gut and the immune system of the muscle. Read more : https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-the-immune-system-during-covid-19.html . Additionally, the gut biome and the muscles are inextricably linked through their energy species. You are what you eat : https://www.back-in-business-physiotherapy.com/latest-news/257-you-are-what-you-eat-and-exercise.html Skeletal, cardiac and smooth muscles all share the same composition, even though they have different roles in the body. A muscle is made of tightly bundled elastic fibres that are wrapped in a thin membrane. Individual muscle fibres are made of protein blocks. Skeletal muscle movement is driven by the neuromuscular system. The brain sends a signal to motor nerves, which then release a chemical. Calcium is released into the cells and the muscle contracts in response. Magnesium in turn acts as a gate keeper of calcium movement into and out of the muscles membrane. Muscle disorders Muscle disorders are collectively known as myopathies. Some common disorders that affect muscles, include: Overuse resulting in sprains, tendonitis, bruising and cramping. Genetic conditions, including muscular dystrophy and Parkinson’s disease. Inflammation, such as myositis. Diseases of the nerves that affect muscles, including multiple sclerosis and motor neurone disease. Chronic conditions, such as fibromyalgia Some cancers. More common muscular disorders are associated with disuse commonly referred to as sarcopenia. Sarcopenia is the 1% loss of muscle mass from the 4th decade of life, which accelerates by the 7th decade to 2%. Since the muscle mass is important in generating muscle power, it's loss can result in fragility. Falls are common in fragile people. Furthermore, bones become weaker, commencing with osteopenia and eventually progressing to osteoporosis. Strong muscles and agility allows people to undertake high impact activity needed for maintaining bone health. Finally, muscle mass is important as an 'insulin sink' to maintain healthy blood glucose levels, as well as a 'protein reservoir' for the immune system. Read more : https://www.back-in-business-physiotherapy.com/we-treat/exercise-muscle-mass.html Can a physiotherapist help treat muscle disorders? Yes, we are here to help you! We help diagnose and treat a broad range of conditions that affect your bones, muscles, nerves and other parts of your body. We will assess your symptoms and develop an appropriate plan to manage them and improve your quality of life. We use treatment techniques, such as soft tissue massage, joint manipulation, dry needling, and exercise prescription. Nutritional considerations should also be entertained and can be read here : https://www.back-in-business-physiotherapy.com/we-do/nutritional-supplementation.html References: 1. Better Health Channel. (2012). Muscles. [Onlinehttps://www.betterhealth.vic.gov.au/health/conditionsandtreatments/muscles (Accessed 19 February 2022).2. Healthline. (2018). Human Body Maps: Muscular System. [Onlinehttps://www.healthline.com/human-body-maps/muscular-system#1 (Accessed 19 February 2022). Uploaded : 24 March 2022 Read More -

LATERAL ANKLE SPRAIN
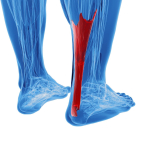
INJURY BLOG: LATERAL ANKLE SPRAIN Are you an avid netball or basketball player? There’s a good chance you have had a lateral ankle sprain (or anterior talo-fibular ligament (ATFL) sprain) at some point! The classic ‘rolled ankle’ is one of the most common sports injuries. However, this common injury doesn’t just occur on the sporting field. It can be caused by stepping awkwardly on an uneven surface, or even wearing high heels. Any action that throws off your balance and shifts your centre of gravity, could result in a painful sprain. What is a lateral ankle sprain and what causes it? The ankle joint is made up of three bones: the talus (ankle bone), the tibia (shin bone), and the fibula (the smaller leg bone). A series of ligaments running in different directions connect the bones and provide stability and support to the joint. There are three lateral (outer) ligaments that help to stabilise the ankle joint, preventing it from moving too much. The anterior talo-fibular ligament, or ATFL is one of them. It is a short ligament that attaches the fibula to the talus. The ATFL is the weakest outer ligament and the most injured. Sports and activities that involve running, jumping, and sudden changes in direction put pressure on the ankle and may cause it to abruptly roll outwards. When this results in overstretching and tearing of the outside ligaments, it is known as a lateral ankle sprain. What are the symptoms of a lateral ankle sprain? If you’ve sprained your ankle you may experience the following symptoms: swelling (immediately or over a few hours); localised tenderness or bruising around the joint; pain when trying to walk, or when you put weight on it. Lateral ankle sprains are graded depending on severity: Grade 1 is a smaller ATFL tear with minimal swelling and the ability to walk with little to no pain. Grade 2 is a larger ATFL tear with bruising, swelling over the outer ankle, inability to walk or bear weight without pain. Grade 3 tear is the most serious with a complete rupture of the ATFL, minimal or no ability to walk without severe pain; swelling and tenderness surrounding the whole ankle. What can you do about an ankle sprain? RICER protocol is suggested for treatment of a sprained ankle: Rest or reduce activity. Ice therapy (on for 20 minutes every two hours for the first 24 hours). Compress the injured ankle using tape or a bandage wrapped firmly around the joint. Elevate the ankle (above the heart if possible). Refer - if you are unable to walk on the ankle, you should seek medical attention to determine if medical imaging is required. You should also avoid HARM - Heat, Alcohol, Running/exercise and Massage, in the first 48 hours to keep any swelling to a minimum. You should also call your physiotherapist at your earliest convenience. How can a physiotherapist help with a sprained ankle? Physiotherapy can help with rehabilitation as you recover from an ankle sprain. Your physio will work with you to develop an exercise program focused on improving the mobility of the joint and regain movement. Evidence shows that commencing rehabilitation exercises within a week of a sprain speeds up recovery. Your physiotherapist can also help you to strengthen the surrounding muscles to aid your recovery. This is particularly important to prevent the injury from reoccurring. Stabilising the ankle using tape or a brace will allow the ATFL to rest and heal. Your physio can recommend a support or brace as appropriate and teach you the correct technique to ensure the best recovery. Further concepts on stability can be read here : https://www.back-in-business-physiotherapy.com/stability.html When you return to your favourite sport activity, you may need to brace or tape the ankle for extra support. Your physiotherapist will provide advice on whether this is necessary. You should also ensure that you warm up and wear supportive shoes when you get back out there! Lumbopelvic dynamics - core and hip - knee stability on ankle imbalance The entire kinetic chain needs to be addressed when dealing with lateral ankle sprains. In chronic ankle instability, weakness of the gluteal muscles has been found by researchers and clinicians. A challenging high repetition functional exercise program, not only mitigates these deficiencies, it also becomes a tool to assess recovery and eventually integrated into the functional assessment of the sport specific activity. Weber fracture Importantly, with an ankle sprain, differentiation with a Weber fracture, is required. These types of fractures and tears of the syndesmosis require some form of immobilisation, such as a moon boot, for up to 6 weeks, and sometimes longer.. LisFranc's fracture Named after a Napoleonic surgeon who noted a very specific injury when cannons rolled back over artillery soldiers feet, a small ligament on the inside of the foot can become detached, leading to a very unstable mid foot, frequently, but not exclusively, seen as a dropped arch. Imaging should be undertaken to confirm diagnosis. Achilles tendon and lateral ankle instability Achilles tendonosis can arise from altered biomechanical patterns of movement such as ankle inversion or foot over pronation as a result of lateral ankle instability. Addressing the entire lower limb chain, including hip strength and symmetrical calf pull can improve the functional stability in the ankle and thus reduce the strain in the Achilles. Read more : https://www.back-in-business-physiotherapy.com/we-treat/achilles-tendonosis.html References: 1. Better Health Channel. (2014). Ankle sprains. [Onlinehttps://www.betterhealth.vic.gov.au/health/conditionsandtreatments/ankle-sprains (Accessed 19 February 2022).2. Physiopedia. (2022). Anterior Talo-Fibular Ligament (ATFL). [Onlinehttps://www.physio-pedia.com/Anterior_Talo-Fibular_Ligament_(ATFL) (Accessed 20 February 2022). Uploaded : 24 March 2022 Updated : 7 April 2022 Read More -

Exercise and sleep on memory
Exercise and sleep on memory by Martin Krause Physical exercise and sleep seem like opposing ends of the spectrum, yet without sleep, exercise becomes difficult. We also know that exercise aids with sleep. Moreover, recent wars in the Middle East have shown that a most potent form of torture is sleep deprivation. Furthermore, investigations into sleep deprivation amongst young active healthy individuals have shown a blood profile, similar to someone with type II diabetes, after 72 hours of no sleep. So why sleep and what affect does sleep have on memory? Contrasting exercise and sleep Performing exercise such as running and cycling (orienteering and adventure racing - visual and spatial memory tasks) improve the capacity for information storage about facts and events (declarative memory) as well as motor skills (procedural memory). Moreover, in certain sports, experiential learning, memory and 'constructivism' through exercising, whilst map reading in variable unfamiliar terrain, have been shown to improve various cognitive traits, including psychological ones. Read more : https://back-in-business-physiotherapy.com/constructivism. At high levels of athletic performance, rest and recovery (R+R) is a very important component to muscles and the immune system during training. Furthermore, sleep also plays an important role in declarative and procedural memory, making it less susceptible to 'interference', thereby allowing short term memory (STM) data to be transformed into long term memory (LTM). Hence, exercise and memory can be used synergistically to improve memory. Sleep deprivation There is an alarming prevalence of sleep deprivation world wide whose costs include reduced work productivity, motor vehicle accidents, work related accidents, medical errors and risk of cognitive impairment due to reduced neuroplasticity. There are two main hypothesis to explain memory and sleep. One, called 'synaptic homeostasis' proposes that during sleep, the increased synaptic processing occurring during the day, is 'depotentiated', whilst undergoing slow wave sleep (SWS). The alternate hypothesis is one which proposes that the primary function of sleep consists of 'strengthening' the synaptic encoding which occurs whilst awake. Specifically, during SWS, a synchronized reactivation results in our brain transforming memory representations from the hippocampus to neo-cortical areas, where they are consolidated into LTM. Body Clock Sleep architecture The architecture of sleep consists of REM (rapid eye movement) and three non REM (NREM 1->3), NREM occurs predominantly in early sleep, whereas REM is later in the sleep cycle. Various brain electrical wave signals occur these phases. NREM 2 is characterised by 'sleep spindles' (SS) of short burst of sigma thalamocortical activity. Slow (delta) neocortical waves and hippocampal waves superimpose into sharp wave ripples during NREM 3. Ponto-geniculo-occipital (POC) and hippocampal theta waves are typically observed during REM sleep. NREM sleep has been implicated in declarative memory, whilst manipulating slow wave activity with acoustic or transcranial stimulation during SWS has been shown to improve this. Both memory formation and encoding are implicated in SWS. Renewal of synapsis through this process, frees up the hippocampus for new memory formation. Procedural cognitive skills through repetitive tasks leads to enhance motor skills by increased sleep spindles and slow waves during subsequent NREM 2 and 3. In contrast, investigations, involving 24 hour immobilisation of a limb, demonstrate reduced cortical activity in those regions, of the brain, represented by the limb. Perturbing slow wave activity during NREM 3 sleep reduces the capacity to increase corticospinal excitability to markers of synaptic plasticity, in response to motor skill acquisition to repetitive activity. Taken together, SWS prevents synaptic saturation through encoding. The role of REM sleep on cortical memory processing remains a source of intense scientific debate. Procedural and consolidation of emotional memory may take place during REM. REM has often been described as the deepest sleep, but paradoxically, the one in which we can arouse ourselves most easily. REM is where our most vivid dreams occur. It is also the time at which we have minimal muscle tone - so that we don't act out our dreams? The benefits of daytime naps on the consolidation of emotional memory have been correlated with the duration of REM sleep and the level of theta activity in the pre-frontal areas of the brain. Impact of exercise on the sleeping brain Meta-analysis has shown that a single bout of day-time exercise improves some objective measures of sleep quality, reducing overall sleep latency, and increasing total sleep time and efficiency. Exercise seems to also reduce total REM and increase the duration of subsequent NREM 3. Simply by investigating visual memory tasks, after exercises and after a daytime nap with or without exercise was used to demonstrate enhanced declarative memory formation when combing exercise and sleep. Other investigations have also consistently found that the retention of a motor skill (procedural memory) improved after a latency period of 1 or more days, thereby implying the benefit of sleep. Mechanisms Exercise increases core body temperature -> increases in body temperature gradient induced by exercise are associated with increases in SW activity Exercise increases Heart Rate (HR) and Heart Rate Variability (HRV) during the early stages of sleep -> increases in HR and HRV during sleep are coupled with SW and SS activity Exercise increases BDNF (brain derived neurotrophic factor) and promotes neuronal plasticity -> increased BDNF and synaptic activity prior to sleep induces SW activity Exercise increases adenosine levels in the brain -> increasing adenosine levels prior to sleep increases sleep pressure and SW activity Exercise increases the secretion of TNF-alpha, IL-1, IL-6 and Growth Hormone -> increases in these neuropeptides and GH expression promotes increases in SW activity Sleep deprivation and exercise Exercise cannot replace the many functions of sleep, but given the immense societal cost of sleep deprivation, it would be of enormous interest to know if exercise can mitigate against sleep deprivation. Given that the definition of endurance exercise is 'resistance to fatigue' at least anecdotally, people with greater endurance, should by definition be less tired, at least during normal activities of daily living. However, this would be very much dependent upon the training regime, and the time spent on recovery. Periodisation of training has been used, to mitigate cycles of intense physical activity with those of moderate and low activity. These cycles can be micro-cycles of a day to a week as well as macrocycles of weeks to months and even years between major competitions. Read more : https://back-in-business-physiotherapy.com/sports-performance/periodisation-of-training.html. However, protecting against fatigue and maintaining executive function isn't necessarily protecting against memory formation. Numerous animal studies have shown the nullifying affects of severe sleep deprivation (4 hours sleep) on the beneficial effects of endurance exercise programs (eg 11 weeks). Human results suggest that short bursts of exercise (10 minutes every 2 hours during 40 hours of sleep deprivation) may transiently reduce sleepiness and fatigue associated with sleep loss, yet they cannot preserve cognition during an extended period of sleep deprivation. Although training reduced the reduction in vigilance, and attention performance from sleep deprivation, it did not protect 'working memory'. However, it can be argued the 'working memory' is an executive function. It would be interesting to examine these responses in sports such as 24 hour Rogaining (Orienteering) or Adventure Sports, where sleep deprivation of 1 -> several days occurs simultaneously with map reading, navigation and decision making. Working memory and decision making is a function of experiential learning in these cases, of expert elite athletes, and hence potentially a true expression of memory. Read more : https://back-in-business-physiotherapy.com/sports-performance/orienteering.html Sleep deprivation and mental health Sleep has been identified as a major determinant for mental health outcomes in elite professional sports people. Investigations on elite Australian Football League (AFL) players concluded that poor sleep results in poor mental health in a population under immense pressure to perform at the highest level. They suggested that mental health issues are under reported and they concluded that sleep assessment should be used as an initial screening tool and re-used routinely during rehabilitation programs (Facer-Childs ER et al 2022 Med Sc Sp Ex, 54, 4, 665-672). These investigators also refer to reports of 62% of all adults reporting insufficient sleep and mental distress, as well as approximately half of all Olympic athletes reporting poor quality sleep. Conclusion Generally, investigations have failed to demonstrate a protective function of exercise on neuroplasticity against sleep loss. Many deficiencies exist in our understanding of a bidirectional effect between exercise and sleep. As the above diagram alludes to, populations need to be investigated which differentiates acute vs chronic exercisers, endurance vs resistance training, acute vs chronic sleep deprivation with memory acquisition in declarative and procedural function Reference Roig M et al (2022) Exercising the sleep-ing Brain: Exercise, Sleep, Sleep Loss on Memory. Exercise and Sport Science Reviews, 50, 1, 38-48 Uploaded : 3 March 2022 Updated : 26 May 2022 Read More -

Stable shoulder workout
Exercise blog: Stable shoulder workout Whether you are a swimmer, tennis player, builder or simply do the laundry - having a stable shoulder is super important in preventing injury! With repetitive overhead actions, the shoulder can fall victim to overuse, resulting in poor movement, pain and loss of range of motion. Here are some simple exercises you can incorporate into your exercise routine to keep your shoulders in tip-top shape! Scap push-ups Scap (or scapular) push-ups use a small range of motion to improve shoulder stability, by strengthening the serratus anterior muscle (located on the sides of the rib cage). They may seem like nothing fancy, but trust us they are worth your time! ● Start with your hands on the floor. Push back into a plank position (with knees lifted or lowered depending on your strength).● Whilst keeping your arms straight, retract or draw your shoulder blades together. After a pause, protract or draw your shoulder blades away from each other, your shoulders and upper back should look slightly rounded.● Continue to retract and protract for 3 sets of 10 reps. Remember to engage your core, tuck your chin and don’t let your hips drop throughout the entire set! Banded row A banded row uses a theraband (or resistance band) to work the upper back muscles, helping support good posture and lessen the strain on your shoulders. Choose a level of band and give this one a go! ● Secure the band to a tree, pole or any secure anchor point.● Hold each end and take a few steps back so the band is taut and your arms are straight.● Pull your elbows back so they graze your ribs. Squeeze your upper back and pause for 3 seconds (remember to keep your shoulders down and relaxed!).● Slowly return your arms to the starting position (parallel to the floor).● Repeat for 3 sets of 10 reps. Wall circles We love wall circles as they not only strengthen the serratus anterior but also target the deep muscles in your rotator cuff. All you need is a wall (duh!), basketball or light medicine ball and a little bit of coordination! ● Place the ball at shoulder height, with one hand firmly placed at the centre. ● Place your other hand down by your side and keep your shoulders down and relaxed.● Start to make small clockwise circles for 10 counts, then change to anticlockwise circles for 10. ● Once you have got the hang of that, try to advance to figures of eight for 10.● Repeat on the other arm.● Repeat for 2 sets. Are you looking for some extra shoulder support? Want some more guidance on your exercise regime? Give us a call on 02 9922 6806 or book your appointment online https://www.back-in-business-physiotherapy.com/book-now! Further Reading https://www.back-in-business-physiotherapy.com/shoulder.html Uploaded : 25 February 2022 Updtaed : 7 April 2022 References 1. McPhillips, K. (2021). If Your Shoulder Mobility Is the Pits, Meet the ‘Scapular Push up’. [Onlinehttps://www.wellandgood.com/shoulder-mobility/ (Accessed 29 Jan 2022)2. MasterClass staff. (2021). Scapular Push-Up Guide: How to Master Scapular Push Ups. [Onlinehttps://www.masterclass.com/articles/scapular-push-ups-guide#3-benefits-of-doing-scapular-pushups (Accessed 29 Jan 2022)3. Cronkleton, E. (2022). 6 Resistance Band Exercises for Shoulders. [Onlinehttps://www.healthline.com/health/shoulder-band-exercise (Accessed 29 Jan 2022).4. Dale, P. (n.d.). Exercises to Strengthen the Stabilizers in the Shoulder. [Onlinehttps://www.livestrong.com/article/334944-stabilizing-strengthening-shoulder-scapula-exercises/ (Accessed 29 Jan 2022) Read More -

Pregnancy, elite athletes and arduous occupations
Pregnancy and physical activity Alex Morgan, USA soccer super star, heavily pregnant and still at training, only months before she was supposed to go to the Tokyo Olympics. How do pregnant women deal with physical activity? What is a good amount of activity and when is it too much? What should be encouraged during pregnancy and post partum? What should be watched for or avoided? Where does musculoskeletal physiotherapy play a part? Since 2016 servicewomen have been fully integrated into the British Armed Forces, including combat roles. However, during pregnancy these duties are downgraded, but can return to full physical and mentally challenging duties, 2 weeks post partum. Little is known about pregnancy and post partum fitness in physically arduous activities. Despite evidence to suggest that women are at risk to pelvic floor dysfunction and musculoskeletal injury, there are no data, nor clinical guidelines on the most appropriate management. Excessive physical activity during pregnancy has been associated with adverse outcomes, including premature delivery, low birth weight, small for gestational weight and preeclampsia. Generally, women reduce their training volume each trimester, whilst no women participate in high impact intense activities in the final trimester. Moreover, the changes induced by pregnancy can last 12 months post partum. Yet, generally, women return to physical activity 6- 12 weeks post partum. Consequently, early return to arduous activities mean that they risk musculoskeletal injury due to deconditioning, potential mental health issues, such as depression, as well as those from the hormonal changes induced ligamentous laxity, altered pelvic floor function, rectus abdominis diastasis and continued changes to hip and back muscular synergies from enhanced anterior pelvic tilt during pregnancy, continuing post partum. Normal timeframes for soft tissue inflammation, proliferation and healing are 12 weeks. Optimal endurance outcome is 16 weeks. Improved strength, at 6-12 weeks, can mask the lack of endurance stability, which requires a longer timeframe for metabolic and mechanical adaptations to take effect. Additionally, people fall roughly into two musculoskeletal categories, the 'floppies' and the 'stiffies'. The former are more adapt to ballistic type of movement activity, whereas the latter more to endurance. This distinction can become clinically important if dealing with synergistic muscular endurance stability post partum. A complete discussion on functional musculoskeletal stability can be read elsewhere on this site : https://www.back-in-business-physiotherapy.com/stability.html During pregnancy and immediately post partum women experience a number of hormonal and physical changes which can affect their physical and mental capacity to carry out arduous activity. These changes include Estrogen, Oxitocin, Progesterone, Human Gonadotropic Hormone, Prolactin and Relaxin hormones. Physically, the pelvis takes on a more anterior tilt, the sacroiliac joints become more mobile, the pubic symphasis load increases, the lumbar spine increases it's lordosis, superior elevation of the diaphragm with increased expansion is accompanied with increased tensioning of the abdominal muscles and consequential reductions in thoracic rotation. Stride length reduces and a perceived 'waddle' may ensue. Hormonal changes have been studied extensively in women participating in soccer. Interestingly perceived respiratory effort reduces, suggesting care must be taken when using RPE during exercise prescription. Furthermore, pregnancy can induce increases in blood pressure. In other circumstances, breathing exercises have been used to reduce blood pressure and may be considered clinically. Moreover, the sling of muscles crossing the thoracic-lumbar-pelvic-hip complex become vitally important in maintaining functionality. Muscle energy techniques and exercise regimes have been employed to maintain correct alignment and synergies. Further reading can be found elsewhere on this site : https://www.back-in-business-physiotherapy.com/we-do/muscle-energy-techniques.html In the clinical scenario, the influence of physical, hormonal and emotional changes need to be taken into consideration if dealing with musculoskeletal dysfunction and exercise prescription. Specific interventions pertaining to assessment and treatment techniques can be found here : https://www.back-in-business-physiotherapy.com/we-treat/pregnancy-back-pain.html Hormonal changes, specifically those which increase ligamentous laxity can not only change the dynamics of the pelvis, but may affect foot pronation, knee angles (knock knee) and the thoracic rings, even the neck. Moreover, pre-existing conditions may be amplified during pregnancy. Elite athletes quite often need to time their pregnancy on world championship and Olympic cycles. They may also feel pressured to return to sport prematurely, both at a physical and psychological level. The prescribing physiotherapist needs to perhaps considered techniques in CBT and NLP when designing exercise programs. However, they may also need to show high levels of moral and ethical standards when dealing with athletes coaches, sponsors and managers, if the time isn't right to return to sport. Please see elsewhere, using post knee trauma as an example : http://cdnback-in-business-physiotherapy.r.worldssl.net/images/pdf/RTS_ACL_consensus_2020.pdf There is a lack of evidence available to develop best-practice guidelines for the care of pregnant and postpartum elite athletes and women employed in arduous occupations. Hereby, the support needed, is given through experienced professionals, such as musculoskeletal sports physiotherapists, rather than guidelines. Each case needs to be treated individually by dividing people with 'complications' vs 'no complications'. Medical-Psychological-Musculoskeletal status should be established by considering, the type, scope and extent of activity wanting to be achieved and more importantly, the realistic timeframes and feedback mechanisms to be used to ascertain such a status. Good communication amongst a team of multidisciplinary specialists must ensue for optimal outcomes to be achieved (Jackson T et al 2022 Ex Sp Sc Reviews, 50, 1, 14-24). In this model, different specialists are required at different stages of the athletes journey, as a mother and as a returning 'super human'. During pregnancy, later as lactating breast feeding women and finally as an athlete, the importance of the nutritionist, will also need to be integrated into the process. Currently, a pro-active approach to pregnancy and arduous activity only occur if pain or other medical complications occur. This is ingenuous to these very special women. A system of care should be established, involving situational specific functional criteria, as well as that of routine maternal care. Musculoskeletal assessments should probably be performed on, at least, a temporal trimester basis. Athletes themselves, should assess their appetite for sport participation risk through Psychometrics such as the Canadian Society of Exercise Physiology "Get Active Questionnaire for Pregnancy". Contrary to popular belief, complications associated with pregnancy such as low back pain and urinary incontinence can be prevented, or at least, not left until post partum to be treated. In arduous occupations the duration of standing and walking should be restricted to 4 hours and the weight lifted to under 100kg (Cai C et al 2020 Am J Obst Gyn, 222, 3, 224-38). This does not consider the persons individual needs and shows an obvious deficiency in the guidelines. Post partum, the uncomplicated pregnancy, can go through the three phases of individualised rehabilitation, as espoused by Bo et al (2017, Br J Sp Med,51, 21, 1516-25) and updated by Deering et al (2020J Orthop Sp Phys Ther, 50, 6, 281-4), whereby active recovery is followed by training and performance. The first phase deals with being a mother and health-birth related concerns. The training phase emphasises functional sports specific exercise, whilst the final phase of 'performance' relates to athletic abilities all the way to the competitive and recovery cycles of sport. This phase encompasses endurance training, periodisation, heart rate variability, psychological stages of injury and recovery, as well as immune considerations and can be read elsewhere on this site : https://www.back-in-business-physiotherapy.com/endurance-training.html . Importantly, these considerations shouldn't be restricted to elite athletes but also considered in women with arduous occupations. Crucially, in an athlete such as Alex Morgan, where pelvic and hip dynamics play such an important role to pregnancy itself, as well as to the integrity of the musculoskeletal system around the knee and back, truly functional exercises need to be integrated into the training program, which are appropriate for the stage of pregnancy and later the recovery and build up into the competitive season. Core stability and lumbopelvic - knee exercises are a critical part of this process. Uploaded : 26 February 2022 Updated : 27 October 2022 Read More -
Vascular System and Musculoskeletal Physiotherapy
Important vascular issues include those of the vertebral artery in the cervical spine. A commonly held belief is that these incidence (-catastrophic or otherwise) are rare with a prevelance of 1 : 100 000. However, the true number may be much greater, as many catastrophic incidents are under - reported due to medico-legal reasons. In my clinical experience, by 2008 I had seen approximately 12 clients with VBI and a further 8 who had petit mal seizures or vaso-vagal syncope with mobilisations to the first rib. The majority of the clients with the 'classic' symptoms of VBI had either a prior incidence from manipulation of the C/S or had a major accident involving the neck - car accidents prior to seat belts, and horse riding incidents were frequently reported. Even a train crash was reported. By 2008 I estimated that I had seen approximately 60 000 clients. Hence, my 20 : 60 000 ratio suggest a 1 in 3000 chance of coming across a client with VBI. A form of pins & needles in the feet during cycling may be due to claudication. Such claudication may be the result of damage to vessels of the abdominal aortic. Additionally the branches of the abdominal aorta descending into the leg as well as the leg vasculature may be damaged by trauma and/or systemic complications (e.g. Marfan's syndrome, vascular diseases, etc). These problems may be a medical emergency whereby immediate consultation with a vascular surgeon is imperative. Virchow's Triad in the aetiology of thrombosis may also be of assistence with differential diagnosis. The 3 variables include Changes in vessel wall (endothelial damage) Changes in blood flow (flow volume/stasis) Changes in blood constituents (state of coagulability) The latter may include screening questions for blood disordes (thrombolytic ones, C-reactive protein , Leiden Factor V, as well as Thalasaemia and Sickle Cell Anaemia), systemic inflammatory conditions (such as Lupus and Scleroderma), the use of oral contraceptives, smoking, diet and frequent flying. Taylor & Kerry (2005) quote a paper from Sise et al (1989) reporting an average 2 year delay in diagnosis in young people where 93% could have been diagnosed with simple palpation of peripheral pulses. from Gray's Antaomy Vascular complications are potentailly overlooked causes of symptoms. This in part may be due to their relative infrequency compared with other conditions seen by physiotherapists. Futhermore, the symptoms of vascular compromise may mimic those of symptoms arising from musculoskeletal structures. Compromise of a blood vessel to the spinal nerve results in radicular pain. A colleague reported the incidental finding of a family friend's teenage boy whose mother was about to take him to the chiropractor for low back pain. What he noted was the boy had 3 socks on his left foot!!! Immediate examination of the lack of pedal pulses and referal to the A+E department confirmed a diagnosis of spinal artery thrombosis. Unfortunately, most peoples friends aren't astute clinicians that recognise "something which doesn't make sense". Arterial kinking of the external iliac artery during hip flexion whilst cycling (and rowing, skatting and Fjell running) have been known to produce pain affecting the buttock, anterolateral thigh, calf and foot with feelings of paraesthesia and numbness in the toes. Cyclists may also describe the feeling of 'fullness' in the leg and lack of power, cramping and/or ischeamic like fatigue. Although anterior/posterior and lateral compartment syndromes are commonly associated with vascular complications in running, similar type (not necessarily area) of symptoms associated with iliac artery, femoral artery and popliteal artery can be missed during the clinical reasoning process. Generally, symptoms are associated with exertion and external compromise of the blood vessel. Apart from the iliac artery already mentioned other examples include the femoral artery in the adductor canal (b/n the adductor magnus and vastus medialis), and the politeal artery interfacing with the medial head of gastrocnemius. Generally, these conditions are associated with anatomical anomalies whereby the external pressure from repetitive movement gradually damages the external lining of the blood vessel. Besides repetitive microtrauma, any external trauma from an accident needs to consider possible vascular damage or the formation of scar tissue and adhesions which could lead to vascular damage. Other clinical examples, include aortic aneurysm which may be due to valsava type maneuvers. Familial history may also be important in differential diagnosis. Additionally, a history of heavy smoking can lead to internal blood vessel pathology. Similarly, women who take the pill may also be at risk. Aortic stenosis may manifest as a result of arterosclerosis or due to underlying congenital defects. These are screening questions which need to be asked during the subjective examination. During the physical examination, the femoral and pedal pulses should be examined at rest but usually need to be assessed immediately after exercise or in the compromising posture where symptoms normally manifest. Further testing should include ankle blood pressure monitoring of each side. Taylor & Kerry (2005) recommend 20 minutes of rest before testing systolic blood pressure in the left and right brachial artery, posterior tibial and dorsalis pedis and then using the "Ankle to brachial pressure index = Ankle systolic BP / Brachial systolic BP". 1 - 1.2 considered normal, 0.75 - 0.9 indicates moderate disease, 0.5 - 0.75 severe disease and <0.5 is limb threatening. (see: Taylor AJ, Kerry R (2005) Vascular syndromes presenting as pain of spinal origin. Ch 36 in Grieve's Modern Manual Therapy: The Vertebral Column. Ed Boyling JD & Jull GA Elsevier Churchill Livingstone). The Upper Limb and vascular compromise from Grays Anatomy The posture of the cyclist (and rower) may also make these athletes particularly prone to upper limb and head/neck vascular conditions. Additionally, one of the most common cycling injuries involves landing on the shoulder or outstretched hand resulting in possible neurovascular traction injury, direct trauma and/or clavicular fracture. The latter has been associated with trapezius muscle dysfunction which can be a precipitating variable leading to Thoracic Outlet Syndrome (TOS). Symptoms of TOS can include typical symptoms of neck, shoulder, elbow and hand pain. Occasionally, people describe a sense of swelling (or fullness) in the arm, with/without concommitant pins & needles or numbness. Vascular components of TOS may be less prevelant than neurological ones. Yet this may be due to mis-diagnosis as the plethora of tests (Adson's, Allen's Halstead's manoeuver, Roos's EAST test) may be falsely positive or negative and variable b/n examiners. Hence, the examination must use the multitude of variables at the clinicians disposal, both Subjective symptoms & Physical signs - inductive and deductive reasoning, to make sense of the clincal picture. When in doubt and further investigations are required, by using the weight of probability from many variables, it may also make the argument for further testing more convincing to a medical colleague. Paget - Schroetter syndrome is a deep venous thrombosis of the subclavian - axillary venous system, also known as "effort thrombosis" (Rutherford 1998, Zell et al 2001) and may account for about 3-7% of all DVT's (Taylor & Kerry 2005). The average patient is in their late 20's to early 30's and males present 3 times more commonly than females. Most commonly complain of quick insidious arm pain (70% in dominant arm), with possible supraclavicular fossa and ipsilateral neck pain. Most commonly occurs in activity with repetitve upper arm, over shoulder height, movements. The usual aetiology is Virchow's Triad which means that specific screening questioning is required. Additionally, other risk factors may include thoracic outlet factors such as cervical rib, anomalous first rib, hypertrophy of the anterior scalene, subclavius or pectoralis minor as well as endogenous factors such as activated protein C resistance and anticardiolipin antibodies (Ellis 2000 in Taylor & Kerry 2005). Taylor & Kerry suggest that observable signs of vascular compromise may include skin pallor or cyanosis - both resting and positional, swelling, and/or superficial venous dilation. Corneal arcus or xanthelasmas (yellowish raises skin changes) around both eyes may be associated with hyperlipidaemia and hypercholesterolaemia. Staining of fingers may be a more accurate indicator of tobacco consumption. Obesity and state of mental awareness may also reflect underlying cerebrovascular state. Hand and digital examination should also include nail squeezing - indicative of capillary refilling time. These should be perfomed in various positions of potential vascular compromise. Nail abnormalities may be present. Pulses should be tested, stethescope auscultation should be undertaken and the pressure cuff sphygmomanometer and hand held doppler or automatic blood pressure monitor used (Taylor & Kerry 2005). Taylor & Kerry (2005) argue quite strongly that vascular examination is such a miniscule part of both under-graduate and post-graduate degrees that we may be implicated in delayed diagnosis and initiating innapropriate treatment. Clinical example : Facial Numbness Blood Disorders Thalassemia (British English: thalassaemia) are forms of inherited autosomal recessive blood disorders that originated in the Mediterranean region. In thalassemia, the disease is caused by the weakening and destruction of red blood cells. Thalassemia is caused by variant or missing genes that affect how the body makes hemoglobin. Hemoglobin is the protein in red blood cells that carries oxygen. People with thalassemia make less hemoglobin and fewer circulating red blood cells than normal, which results in mild or severe anemia. Thalassemia can cause significant complications, including pneumonia, iron overload, bone deformities and cardiovascular illness. However this same inherited disease of red blood cells may confer a degree of protection against malaria, which is or was prevalent in the regions where the trait is common. This selective survival advantage on carriers (known as heterozygous advantage) may be responsible for perpetuating the mutation in populations. In that respect, the various thalassemias resemble another genetic disorder affecting hemoglobin, sickle-cell disease. Factor V Leiden, also known as Leiden Factor 5 (and sometimes factor VLeiden) is the name given to a variant of human factor V that causes a hypercoagulability disorder. In this disorder, the Leiden variant of factor V cannot be inactivated by activated protein C. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst Eurasians Uploaded : 17 November 2017 Read More -

Male fertility and exercise
Male fertility and physical activity Male fertility is dependent upon a balance between testosterone levels and REDOX reactions, which define sperm quality. With regular exercise, anti oxidant stress becomes more regulated, which in turn is thought to impact the mitochondria. The type of exercise appears to be important, as acute intense exhaustive exercise decreases male reproductive potential, whereas a combination of endurance and resistance training may be a successful therapy for male fertility. Exercise, in general has an impact on hypothalamic-pituitary gonadal axis. There are also 4 broad categories of spermatogenesis (spermatogonia, spermatocytes, spermatids, and spermatozoa) which all require different types of mitochondria as an intermediary. A parallel association between structural changes, cell localization and metabolic status during spermatogenesis has been postulated, where the number and size of mitochondria cristae is increased by an increase in respiratory activity. Furthermore, exercise stimulates testosterone which plays a major role gamete mitochondrial production in Leydig cell steroidogenesis. Evidence moderate aerobic treadmill training improves semen quality in obese men (Rosety MA et al 2017 Nutr Hosp., 34, 3, 603-7) moderate intensity continuous training was more beneficial than high intensity continuous or high intensity interval training at both 12 and 24 weeks after training (Hajizadeh Maleki et al 2017 Reproduction, 153, 2, 157-74) 1026 sedentary men attending a fertility clinic were reported to have improved sperm quality with moderate aerobic exercise (Hajizadeh Maleki et al 2017, Cytokine, 2017, 92, 55- 67) training at higher intensities seems to diminish sperm quality especially amongst cyclists, mountain trekkers and runners (Hajizadeh Maleki et al 2017 Reproduction, 153, 2, 157-74 ; Hajizadeh Maleki et al 2015 Clin J Sport Med, 25, 6, 535-40; Hajizadeh Maleki et al 2014 Clin J Sport Med, 24, 4, 302-7; Vaamonde D et al 2006, Int J Sp Med, 27, 9, 680-9) in some cases it's the type of exercise which impacts sperm quality, such as the gonadal irritation from heat, tight clothes and mechanical loading during repetitive long distance cycling Mechanisms The common target of physical exercise affects, such as oxidative stress and testosterone are gamete mitochondria, as these control energy metabolism and oxidative homeostasis. Mitochondrial Leydig Cells must be functional to synthesise testosterone. Dysfunction results in oxidative damage to macromolecules (lipids, proteins, mtDNA) and cause a decrease in ATP levels. When proteins and membrane lipids are damaged and mtDNA is fragmented the process of oxidative phosphorylation is severely affected, causing a decrease in energy production, with subsequent meiotic arrest and abnormalities in sperm morphology. Additionally, high levels of reactive oxygen species (ROS) leads to the release of cytochrome c, which induces apoptosis and a decrease in sperm number. Reference Lunetti P, Capobianco L, Zara V, Ferramosca A (2021) Physical Activity and Male Reproductive Function : a new role for Gamete Mitochondria. Exercise and Sports Science Reviews, 42, 2, 99-106 Uploaded : 3 February 2022 Read More -

What is Patellofemoral Pain Syndrome?
What is Patellofemoral Pain Syndrome? PFPS is an umbrella term for pain in and around the patella (kneecap). It is sometimes called “runner’s knee” or “jumper’s knee” because it is common in people who run or play sports, but it can affect anyone. PFPS is most commonly caused by vigorous overuse of the knee, and jogging, squatting, even climbing stairs can be culprits. Suddenly changing or increasing the amount of physical activity you do can also put excess stress on the knee, leading to PFPS, as can using inappropriate equipment or footwear. PFPS can also be caused by incorrect alignment of the patella. If you’re experiencing PFPS, you’re likely to have pain in your knee that gets worse when you sit, climb stairs, run or squat. The pain can be felt anywhere around the knee. What can you do about PFPS? If you’re experiencing pain in your knee that you think could be PFPS, stop doing the activities that are causing you pain until you feel better. This might mean switching to low impact exercise for a while. Use the POLICE method: Protect – avoid making the painful knee worse by stopping the activity you are doingOptimal Loading – keep moving the joint as pain allows (don’t become a couch potato!)Ice – use cold packs for 20 minutes, two to three times per dayCompression – a knee bandage can help prevent swelling (your physio can advise on the best one)Elevate – whenever you can, rest with your knee supported in a position higher than your heart See your physiotherapist to check the severity and type of the injury and see what needs to be done to help you recover. How can a physiotherapist help with Patellofemoral Pain Syndrome? Your physio will examine you to determine exactly what is causing the pain and where the specific problem lies. As there are a number of tendons and muscles in this area that could be affected, you need to know exactly what the problem is before it can be addressed. Depending on the nature of your problem, there are a range of exercises that your physio might suggest to help strengthen and stabilise the area, as well as helping you regain movement. Manual therapy and massage may also help reduce pain and recover motion. Your physio will be able to advise as to whether you need any bandages, taping or support equipment, and which ones are right for you. They will also advise on whether you’re wearing the right shoes, using the right equipment and following the best training regime to reduce the likelihood of the problem coming back. Frequently, the muscle synergy around the knee becomes altered. The cortical representation of the muscle attaching to the inside of the knee cap (vastus medialis) is frequently diminished and relocated to another aspect of the cortex, making normal muscle contractions very difficult. Retraining the brain becomes important, to enhance the vastus medialis activity. see below for further explanation on Cortical Resource Mapping and Game Theory Exercises which are designed to 'unload' the knee joint become important. These include synergistic loading of the upper 2/3 of the hamstrings/quadriceps as well as gluteal activation. Furthermore, calf strength is of paramount importance, as the calf absorb up to 70% of the load when landing on the ball of the foot. Frequently, continuous hopping and skipping are the last functional dynamic exercise outcomes used to determine full return to sporting activity. reverse lunges sideways lunges Swedish squat quads hover hip hitches core stability and gluteal one legged bridges hopping and skipping Leaning forward, through the rotation in the hip, with a straight back, should take the pressure out of the knee, whilst doing sideways and reverse lunges, as well as the quads hover. Importantly, with the quads hover, the movement of the knee is forwards and backwards, NOT up and down. Perfecting reverse lunges, is the precursor to other lunging activity. Progression, should be reverse lunge, diagonal reverse lunge, sideways lunge. Initially using a slider on the floor and ultimately progressing to a small step. What can you do to prevent PFPS? If you think you might be at risk from Patellofemoral Pain Syndrome, the best things you can do to reduce your chances of injury are: Introduce a new training regime or a change in activity slowly – get physiotherapist advice on putting your activity plan in place Get expert guidance to make sure your footwear is appropriate and supportive, and that you’re using any equipment correctly Maintain a healthy weight to avoid putting excess strain on your knees Warm up thoroughly before exercising Stretch your quads and hamstrings before and after exercise Don’t push yourself – if you’re exercising and your knee (or anything else for that matter) begins to hurt, stop, and get on the phone to us! Muscle coordination within and between limbs Researchers have demonstrated the importance of intra-limb coordination for the development of peak sequential power from knee to hip to ankle, and the reliance on multiple muscles to produce torque. At back in Business Physiotherapy, we use a very comprehensive approach to treating the spine and pelvis, whereby, even improvements in areas of the body not traditionally associated with leg dynamics, such as ribcage biomechanics, will improve power output in the legs. Treatment of pelvic asymmetries and low back conditions can frequently relieve recalcitrant chronic knee pain. These issues have been addressed elsewhere on this website. Game theory and the curious concept of immune - muscle synergies It is interesting to speculate that both the novice and elite orienteer are more susceptible to infection because they both have more rigid motor patterns, are less inclined to take risk and therefore are less likely to be confronted with error generating patterns of correctability? The assumption underlying game theory is that there is a resource over which there is a conflict. A factor which the orienteering paradigm partially defines, and identifies, is the freedom of thought and movement. That fact that many investigations are looking at exercise and the immune system, using captive animals, might be problematic in itself. These animals are in a predictable environment, which for this purpose is ethical, reductionist and conforms with rigorous scientific research protocols, which is practical, as it reduces the number of 'dependent' and 'independent' variables. However, from an evolutionary point of view, and from the perspective of the example used here, where in orienteering, more may be learnt and fine-tuned, in an unpredictable variable environment, whereby the use of caged animals may be limiting the validity of the paradigm (deterministic chaos) which is under investigation. Moreover, in terms of cognition, confinement is a stressor. Moreover, the calmness and clarity of thought needed in the freedom of orienteering (running and navigating) through the landscape can be considered the antithesis of the caged animal. Our ancestors were striving for energy security through appeasement, subjugation or dominance over other life forms, both internally and externally. In this sense, the 'freedom to navigate and move' paradigm, suggests that our evolutionary forefathers, used their muscles, to propel themselves out of Africa, for 'greener gut biome pastures'. Therefore, maintaining good health in new and potentially 'dangerous environments', involved an unpredictable deterministic variable. As it pertains to cognition, it is an intriguing idea that a motor-sensory curiosity, drove a mechanism, which simultaneously caused muscle hypertrophy, and endowed the muscles with enhanced glutamine and cytokine concentrations, which were needed, if an immune response to pathogens was encountered. Additionally, it is conceivable, that the gut biome was driven by the laws of thermodynamics, in the search for energy. Subsequently, the gut-environment interface provided the interaction needed, to both provide energy for movement, allowed the immune system the encounters needed to flourish, and achieved the abundance of gut species required, in a variety of situations, from feast to famine. Therefore, the gut - muscle - brain cognitive pathway, was driven at a conscious and subconscious level to meet the demands of thermogenesis and immune competency, resulting in collective gain amongst all cells which required energy. Akin to Zen Buddhist philosophy, suggestions are, that the constant sensation of mild hunger, drives the clarity of thought needed, to strive for all encompassing meaning and ultimate enlightenment. Yoga, using animal poses, to stretch muscles and enhance breathing, whilst calming the cognitive state, may be based on the same primeval paradigm, of what is good for muscles is also good for the gut and brain. The 'dove and hawk' paradigm in game theory is interesting. If a hawk and dove compete over the same resource, direct open conflict of the dove with the hawk would be suicidal. Hence, one would think it's better to be a hawk. However, what if two hawks meet, there will be only one winner and potentially both could be injured for the same net gain. Whereas, if two doves meet, they may postulate and gesticulate and eventually one may retreat or they may even share the resource, with the less risk of injury. Hence, the stakes for the Hawk are much higher. Humans have always been in conflict for resources. Does this mean that the immune system is tuned by adaptation to 'individual' resource dominance? Or, as people developed and evolved as tribes, into communities did our immune systems come to share pathogens, which may have entailed 'herd immunity' but at the same time, gave humans a lack of species variability, making them more vulnerable to 'novel' pathogens? Even more intriguing, is the notion that within a group of similar, the weakest may be driven out, seeking new resources, which in this case means new environments and new pathogens, invoking an 'immune enriching' response? Continuing with the 'hawk dove' analogy, if we have too many hawks in a population, the consequences are constant conflict. If too many doves, constant compromise. In fact, a single dove in a hawk environment might be totally ignored, as might a single hawk in a dove environment. Thus, the apparent weaker species could be at an advantage when it's the outlier? To carry this further, we could postulate that the hawk is more prone to injury. Does this mean that in humans, the more dominant 'aggressive' individuals have an immune system which is more in demand for potential or actual injury? Whereas, the postulating dove, activates it's immune system minimally when it's performing some form of escape or deception? Interestingly, most animal conflict encounters, go out of their way to avoid injuries to themselves. Regardless, it's likely, that in both 'stressful' situations, the immune and musculoskeletal systems are activated, in a proportionately preparatory manner. Thus, the stronger the variability in the individual, the more proportional, and therefore robust their immune response. Needless-to-say, a balance between hawks and doves needs to be established for mutual gain to take effect. In terms of the human genome, it's very underwhelming, yet it has evolved to a complex multi-cellular life form, still totally dependent upon trillions of unicellular life forms within the individual gut biome. This flies in the face of Darwinian evolution and the survival of the fittest, in that simple life forms keep complex life forms alive. Even, within the gut biome, there appears to be a symbiotic relationship with parasites and a healthy immune system (i.e. parasitic exposure appears to reduce auto-immune disease such as allergies). A 'simple' multitude (gut biome) balanced with a 'complex' minority (human DNA). Humans eat to feed their gut, their gut breaks down energy from food, which in turns propels the human, with the energy gained, to find more food. A net win win situation using the gut-brain-muscle axis. In terms of muscles, a simplistic view, (using this analogy) would be that the glycolytic (fast twitch) muscles are the 'hawks', whereas the oxidative (slow twitch) muscles are the 'doves'. The glycolytic muscle fibres tend to be ballistic two joint (mechanical) energy straps which propel the body, whereas the oxidative endurance (metabolic energy) muscles are one joint deep muscles tending to stabilise joints and prevent injury. Therefore, the 'hawks' make the large perturbations whereas the 'doves' dampen them. Luckily, there is a muscle glycolytic fibre type which can become more oxidative (endurance power). Hence, 'hawks' which can be tempered towards a 'dove' like mentality....a balance between metabolic and mechanical energy systems, where the mechanical perturbations stimulate the metabolic-immune response. In terms of neurophysiology, this analogy could potentially be taken further, where the sympathetic nervous system is the 'hawk' and the para sympathetic nervous system are the 'doves'. Fortunately, within the sympathetic nervous system there are self modulating ('dove' like) perturbating mechanisms. But it could be envisaged that putting a 'hawk' amongst the 'doves' wakes them up from a state of complacency. Similarly, 'staleness' is an 'existential threat' to any training regime and to any 'immune system'. Read more : Muscles, Deterministic Chaos and the Immune System Cortical 'resource' representation, mapping, in knee muscles, after injury In the context of physiotherapy, a simple model of game theory might be applied to the problem of anterior knee pain. Commonly, this problem is associated with pain at the front of the knee when it is in flexion (a bent position), such as stair climbing, cycling, squats, etc. The conventional wisdom is that the patella (knee cap) is mal-aligned due to a lack of medial (VMO) muscle activity pulling the patella inwards and too much activity of the lateral thigh muscle (VL) pulling it outwards. Game theory could be applied here as the muscles compete for finite cognitive territory to represent their individual (rather than mutual) function, where ultimately neither muscle gains, both loose out to pain generating cortical representations, reducing fidelity and increasing noise in the system. However, if the muscles were to readjust for a functional outcome, they would do so through gaining a synergy of proportionally shared resources (power sharing), hereby a dominance over pain and dysfunction is gained. Physiotherapists, use functional electrical muscle stimulation (FEMS) to give added 'resources' to the VMO, which then can be used during functional exercise training. As the system adjusts, the pain improves and the gain experienced by all the muscles convinces the VL to fire with the VMO, hamstrings and gluteals in a functional synergy for stairs, cycling (see previous), squats, etc. Hereby, game theory would suggest all have won and injury has been avoided. Investigations in Australia, by the Brazilian, Abrahao Baptista (2014), looking at 40-50 year old women with chronic knee pain, demonstrated the significant reduction in the volume of muscle representation in the cerebral cortices, as well as changes in the location of these muscle representations (see below). Moreover, in the context of neurons who 'fire together, wire together' it would be of utmost importance to find exercises that act as functional synergies and relate in a real or a 'virtual' manner to the environmental context in which they need to fire. This also becomes particularly important in psychological behavioural issues of 'fear avoidance' and disuse atrophy. Ideally rehabilitation stimulates 'wiring and firing together' of goal-oriented regions of the brain rather than those which are directed at fearing and avoiding movement. Therapist must instil confidence through their choices of treatment whereby they outline and hence monitor the expectations of outcome. In this picture, it is clear that, the volume of the quadriceps muscle representation in the cortex of people with anterior knee pain (PFP = patello femoral pain) is dramatically reduced. Not seen here, but demonstrated in other research, is the phenomenon of pain processing altering cortical activity in various brain areas (see below). Individuals with patellofemoral pain (PFP) had reduced map volumes and an anterior shift in the M1 representations, greater overlap of the M1 representation and a reduction in cortical peaks across all three quadriceps (RF, VL, VMO) muscles compared with controls.(Te et al 2017 Pain Medicine, pnx036, https://doi.org/10.1093/pm/pnx036). Physiotherapists use FEMS (30HZ functional electromuscular stimulation) to enhance muscle cortical representation in the brain, which improves function and in turn improves pain. FEMS stimulation readjusted cortical mapping to that seen in asymptomatic individuals. Alternatively, therapists use trans-cortical stimulation of the pre-frontal cortex to improve 'executive function' and pain. Brain activation related to spatial discrimination of noxious stimuli is distinct from that related to perceived pain. These images are located at x = 0 mm, x = 30 mm, z = 5 mm, and y = –30 mm in standard stereotaxic space. IPL/SPL, Inferior parietal lobule/superior parietal lobule; GP/PT, globus pallidus/putamen; M1, primary motor cortex; DISCRIM., discrimination. (Oshiro et al 2007 J Neuroscience, 27, 13, 3388-3394) Abrahao Baptista (2020) and his colleagues are conducting research into trans-cortical stimulation and vagal (para-sympathetic) nerve stimulation in the treatment of patients with COVID-19. They are basing their assumptions and working hypothesis on some positive results a rheumatologist has had with this methodology for the treatment of auto-immune inflammatory disease. COVID-19 has many of the hallmarks of an auto-immune disease, including the cytokine storm. This treatise has argued that sympathetic, rather than para-sympathetic, stimulation is necessary to add a deterministic chaotic input which perturbs the immune system into action. It would be intriguing to speculate a large perturbation between sympathetic and para-sympathetic can also activate the immune response. In this case, the illness has already set the sympathetic nervous into a heightened chaotic state, which needs additional buffering (redundancy) from the vagal nerve stimulation. References 1. Physiopedia. 2021. Patellofemoral Pain Syndrome [Onlinehttps://www.physio-pedia.com/Patellofemoral_Pain_Syndrome2. OrthoInfo. 2020. Patellofemoral Pain Syndrome [Onlinehttps://orthoinfo.aaos.org/en/diseases--conditions/patellofemoral-pain-syndrome/ Uploaded : 23 January 2022 Updated : 7 April 2022 Read More -

Back to School Health Tips
Back to School Health Tips Here we go again! The kids are heading back to school, and it’s either a huge sigh of relief or an inward groan depending on your perspective and situation. But whether you’re bundling out the door, preparing for another round of homeschooling or tearfully waving your little angels off at the school gate for the first time (it’ll get easier fast, trust us), there are a few things you can do to get this term off to the healthiest possible start. 1. Get the right backpack Obviously your kid is going to want the one in the coolest colours with this month’s favourite character on the front, but it also needs to be sturdy enough to carry all their belongings, and comfortable for them to wear. Look for one with wide shoulder straps, make sure they wear it on both shoulders, and adjust the straps so that the weight of all those books is supported evenly and securely. 2. Set up their homework environment Whether you’re homeschooling your kids permanently or temporarily (thanks Covid), or you’re just looking for somewhere for them to do their homework in the evenings, make sure they’re not sprawled on the sofa or the floor but have an environment that supports their back and joints. Their desk and chair need to be at the right height so they can sit with their back straight, feet flat on the floor, elbows at right angles and hips slightly open. An adjustable desk and chair can be a good choice so they can last your growing child. Make sure the top of any screen they’re working from is at eye level so they are looking straight ahead with their neck held softly. And get them to take regular breaks from the screen! 3. Check their shoes Why do kids grow out of everything so fast?! School shoes are one of the most annoying things to keep replacing because they’re expensive and you can’t get away with ones that are just a tiny bit off like you can with their other clothes. But it really is important to make sure their shoes fit correctly. Badly fitting shoes can damage the development of the foot and affect the way they walk – which can cause injuries in other areas of the leg, knee, hip… you name it. Get their feet measured regularly, choose shoes that are comfortable and easy to move around in, and ones with non-slip soles that can help reduce the likelihood of falls. Good luck, parents! References 1. American Academy of Paediatrics. 2015. Backpack safety. [Onlinehttps://www.healthychildren.org/English/safety-prevention/at-play/Pages/Backpack-safety.aspx#:~:text=1%20Always%20use%20both%20shoulder%20straps.%20Slinging%20a,up%20the%20muscles%20used%20to%20carry%20a%20backpack. [Accessed 14 December 2021] Upload : 23 January 2022 Read More -

Osteoarthritis
What causes hip osteoarthritis? Osteoarthritis is a result of a gradual degeneration of the cartilage that lines the ends of bones that join to form joints. There is no one specific cause. Almost any joint in the body can develop osteoarthritis, but load-bearing joints (such as the knees, hips and spine) are the most susceptible. One in ten people over the age of 65 will experience hip osteoarthritis, although it can develop from the age of 45 (it is highly unlikely, but not impossible, to develop earlier). If you have a family history of osteoarthritis, have had a hip injury or hip function problems in the past, are overweight or have a job that involves long periods of standing or heavy lifting, then you are at increased risk of osteoarthritis. What are the symptoms of hip osteoarthritis? Hip osteoarthritis thins the cartilage of the hip joint and makes the surfaces of the hip joint rougher. This can lead to pain and swelling in the area. People with hip osteoarthritis often experience at least some of the following: ● Progressively increasing pain in the hip● Pain felt with movement (although it may ease off with continued movement) and at rest● Pain that is aggravated by cold weather● Pain in the groin or thigh that radiates to the buttocks or knees● Stiffness of the hip or a “locking” sensation in the joint● Decreased range of motion or an affected walking pattern (i.e. limp) However, approximately 50% of patients with hip osteoarthritis do not have these symptoms, so any changes in your movement as you get older are worth getting checked out, just in case. How can hip osteoarthritis be treated? One of the most effective ways to treat osteoarthritis is with exercise. We can work with you to develop an exercise program that will strengthen the muscles around your hip, stabilise and protect the joint, increase your range of motion, improve your posture and reduce any additional strain on the joint. We will also take a look at the physical activities you are doing day-to-day, and advise you how best to structure them so that you are keeping your hip moving but not overdoing it. It’s important to keep moving when you have osteoarthritis, but breaking up physical tasks into chunks rather than doing too much at once can help to reduce the pressure on your joints. There may also be insoles, walking aids or other forms of supportive equipment that we can recommend to take stress off your hip, as well as changes to your lifestyle and home/work set-up that may help. Manual therapy and massage are also frequently used to reduce pain and increase movement. Massage may include myofascial trains and dry needling to improve the 'slings' across the hip and pelvis. Additionally, Muscle Energy Techniques are also employed aiming to re-align the pelvis and hips. When it comes to osteoarthritis of any kind, the sooner you get treatment, the better. In the worst-case scenario, hip osteoarthritis could require surgery or even a total hip replacement. So come and see us early before the pain gets too severe. How can hip osteoarthritis be prevented? The sooner you start to look after your hips, the more you can reduce your risk of developing osteoarthritis. Here are a few things you can start doing right now: ● Regular exercises to strengthen the muscles around the joint and stretching to improve mobility will help to protect the hip from degeneration. ● Make sure you always use the correct technique to lift heavy items, and don’t lift excessive loads. ● Maintain a healthy weight, as obesity puts strain on your hips. ● If you are sitting for long periods of time, ensure that your chair provides adequate support and that your hips are slightly higher than your knees. Try to avoid crossing your legs. Take regular breaks to move around. Do lots of 'buttock ups' Diet Diet can be very useful in preventing and ameliorating osteoarthritis. Simple weight loss programs such as the 16 : 8 diet (fasting 16 hours whilst eating lunch and dinner), can lead to weight loss, but may also be aimed at reducing cholesterol. As we know cholesterol can block the arteries. As the joints are at the end of the circulatory chain, then even minor blockages can be a problem. we also know that many tendinosis/bursitis in the hip may be due to immune-metabolic compromise. Supplementations have been controversial, however 1000mg of EPA/DHA fish oil have been recommended, as have New Zealand green lip muscles, forest berry and cherry anti-oxidants. Apart from the anti-oxidant properties, fish oil has an effect on blood viscosity. Additionally, if glucosamine is taken, the minimal dose is 1200mg glucosamine with 800mg MSM and 800mg of Chondroitin. However, the latter may have an effect on any thyroid issues. Further Reading : https://www.back-in-business-physiotherapy.com/we-do/nutritional-supplementation.html References 1. Physiopedia. 2021. Hip Osteoarthritis [Onlinehttps://www.physio-pedia.com/Hip_Osteoarthritis2. OrthoInfo. 2021. Osteoarthritis of the Hip [Onlinehttps://orthoinfo.aaos.org/en/diseases--conditions/osteoarthritis-of-the-hip Uploaded : 25 November 2021 Read More -

Sleep
Have yourself a sleepy little Christmas The most wonderful time of the year is nearly upon us… and for some of us, that means sleepless nights! A U.K study revealed that on average, we lose 21 hours of sleep in the week leading up to Christmas, and U.S research found that 53% of parents lose sleep over the festive period, with 70% getting less than six hours on Christmas Eve. And that’s just the adults. We know sleep is incredibly important for our overall physical and mental health, so what can we do to get more rest during one of the most exciting (and sometimes stressful) times of the year? 1. Introduce wind-down time Alcohol and watching TV are two things guaranteed to disturb your sleep. But festive drinks and seasonal movies are staples at this time of year. We also spend a lot of time on our phones, keeping in touch with friends and family. Try to stop drinking and turn off all screens an hour or two before bed, to give your brain and body time to wind down. You can make this part of a calming nighttime routine, including elements like a hot bath, some light stretching, reading a book or listening to relaxing music to help you prepare to drift off. 2. Get organised Two of the biggest causes of seasonal insomnia are excitement about everything that’s coming up and worry about how to organise it all. Organise as much as you can in advance. Make lists of what you need to do and any deadlines for when you need to do it. Start buying and wrapping presents early and start to prepare food in advance where you can. You can also make writing your next day’s to-do list part of your nighttime routine, so that all your thoughts about tomorrow aren’t racing around in your head when you’re trying to settle down to sleep. 3. Move your body When you’re rushing around trying to get everything prepared for the holidays, your exercise routine can easily fly out the window. Exercise helps you to sleep better and deeper at night, and helps you to feel more energetic during the day. Try to get at least ten minutes of vigorous activity each day, even if it’s just a brisk walk. The good news is, dancing around your living room energetically to Christmas songs totally counts! 4. Take time out The festive period can be a hectic time, with lots of demands on you physically and emotionally. Amongst everything that’s going on, take some time for yourself. Try to put aside just five or ten minutes in the day to practice mindfulness or meditation to calm, rest and focus your mind. References 1. Banbury Guardian. 2012. Are you getting enough sleep over the holiday break? [Onlinehttps://www.banburyguardian.co.uk/news/are-you-getting-enough-sleep-over-holiday-break-23588932. SleepCycle. 2018. Parents sleep less and drink more during the holidays [Onlinehttps://www.sleepcycle.com/sleep-science/parents-sleep-less-and-drink-more-during-the-holidays/ Uploaded : 25 November 2021Sl Read More -

Postural Orthostatic Tachycardia Syndrome (POTS)
Postural Orthostatic Tachycardia Syndrome (POTS) POTS is a condition of exercise intolerance in positions other than the horizontal. Clients will often present, complaining of symptoms of dizziness in standing, whilst feeling comfortable in sitting and lying down. In the older person it can be a result of cardiovascular deconditioning where the Heart Rate and Stroke Volume do not produce enough cardiac output (CO=SVxHR). In the younger individual, it may present as part of a condition from a different aetiology. In people who have suffered a Whiplash Associated Disorder (WAD) - anterior sympathetic cervical ganglia, or in a person with concussion, POTS symptoms may arise. Additionally in people who have Ehler Danlos Syndrom (EDS) or Joint Hypermobility Syndrome (JHS) POTS like symptoms due to autonomic dysregulation may present with POTS at any stage of life. Any thoracic ring issues which affect the peripheral sympathetic ganglia may also result in POTS like symptoms. Essentially, a person may have low blood pressure and elevated heart rate (Tachycardia) as a compensatory mechanism. POTS is frequently misdiagnosed and requires a tilt table and blood pressure monitoring to aid in the differential diagnosis. The heart plays a pivotal role or orthostasis, where left vetricular untwisting mechanics is critical for tolerating central hypovolaemia (as a result of reduced cardiac filling during orthostatic stress) in both high and low physical fitness people (Shibata S et al 2021, Ex Sp Sc Rev, 49, 2, 88-98). Causes of POTS interesting to physiotherapy include cardiovascular autonomic dysregulation, where tachycardia occurs due to decreased stroke volume from low blood volume (hypovolemia). Exercise conditioning results in increased stroke volume. However, all factors of exercise prescription need to be addressed including hydration and diet. sympathetic peripheral neuropathy where the calf blood vessels don't vasoconstrict sufficiently. Additionally, the calf muscles don't produce enough venous return to effectively act as the second 'pump' of the body. Exercise conditioning in supine (Pilates and Yoga) may be particularly useful for the venous return. hyperadrenergic activity in standing (increased noradrenergic activity).Yoga (stability) and Alexander style activity with a meditation component. Feldenkreis may also be useful for mind-body awareness joint hypermobility (EDS and JHS) with specific physiotherapeutic interventions See Fu & Levine (2019) for a detailed review The Children's hospital in Philadelphia has simplified the Dallas POTS exercise program to that which follows. Chronological factors in rehabilitation Where a person begins will depend on their current condition. Months 1-4 you should only exercise in a horizontal position, here are examples:o Recumbent bikingo Rowing Ergometero Swimming laps or kicking laps with a kickboard Month 4 you can begin to use the upright bike if it is available Month 5 is when you can begin further upright training (elliptical or treadmill) Use the calendars as a week by week guide. You may need to move training sessions around, but please complete all of the recommended training sessions within that 7 day period. You will need to do this in order to move forward to the next week. One requirement is that after Maximal Steady State’ workouts you must always complete a ‘Recovery’ workout the next day. A ‘Recovery’ workout is when you do anything active, but keep your heart rate below the zone prescribed. Examples of recovery workouts include: low cycling at a low level on the recumbent bike- Using a kickboard to leisurely kick laps in the pool Taking a walk outdoors Playing in the yard Anything active that gets you moving continuously for the prescribed amount of time If for some reason you miss a period of workouts (illness, injury, etc.) then you should go back in the calendar and repeat the workouts. For example: If you miss more than 2 cardio workouts then repeat the full week If you miss a week, back up and repeat 1 week If you miss more than 2 weeks, you should restart from the beginning of the month that you are currently in. If this is too hard then you may need to back up further. The program gets progressively more difficult. When you take time off, you lose some of your hard-earned conditioning so it is important to repeat workouts. You may also need to return to horizontal modes of training (i.e. recumbent bike, swimming, rowing) before moving forward in the program again. TIPS: Use the equipment you have access to and can tolerate training on, but starting with one horizontal mode of training is key. Rowing with the rowing ergometer is preferred because it mimics open water rowing. People who row in the open water tend to have the largest,strongest hearts out of all competitive athletes. Rowing is great to strengthen your heart muscle! If you are unsure how to use it ask someone toshow you. Keep the workouts spread out throughout the week. This is more beneficial than bunching them up and then taking several days off fromexercising. Try not to take more than 2 days off from exercising. This is KEY!! If you cannot complete all the sessions for that week, you need to repeat that entire week again before moving forward. The Basics of the Strength Training The strength training sessions prescribed should take you 20-30 minutes to complete. All weight training should be done using body resistance or onseated equipment. If you are unfamiliar with strength training then you should consult with a trainer to help you use proper form and technique oneach machine. It is recommended that you keep a log of your exercise. The strengthening exercises are mainly for the lower body and core, and thisis intentional. Lower body muscles act as pumps when they contract (as you are walking about in daily life) to return blood to your heart. Increasedmuscle mass in your legs means more blood returned with each step you take. TIPS: Strength training can make you sore in the beginning (especially 1-2 days after the workout). Some people find that they can only get to the gym 3-4 days a week. It is fine to do your strength training at the end of your cardio workouts instead of on separate days, if you prefer. If this causes you to become symptomatic then you should try to perform on separate days. Take at least a day off between strength training workouts. You need to allow your muscles at least that day to recover and to build muscle. We do not recommend the use of free weights until you have been able to build your strength and are able to perform with good form. If you have joint hypermobility then you should consult with a physical therapist prior to beginning your exercise program. The therapist can teach you how to protect your joints when you exercise Exercises The Basics of the Horizontal to Upright Cardio Training Months 1-3 = Horizontal or Seated training When beginning this exercise program you need to use equipment where you are seated or horizontal in position because upright positions will likely make your symptoms worse. Examples include: o Recumbent bikeo Rowing ergometero Swimming (or kicking with a kickboard)o Seated stepper machine Month 4 = Upright bike Month 5= Upright exercise - Elliptical (begin without arm motion and then add after a few weeks)- Treadmill walking (no incline at first) Month 6-8 = Upright Training - Add in use of arm motion on the elliptical and incline on the treadmill- Make more challenging during this time as tolerated Jogging and stair stepping can be tried only after you have performed either elliptical with use of arms or treadmill walking on an incline and did not have an increase in symptoms. You do not ever have to jog if you do not want to. Warm Up and Cool Down: - Can be done on any piece of equipment and should NEVER be skipped.- At the end of your warm up you should have your heart rate approaching the target heart rate range for your workout.- For the cool down, simply remove all resistance from the piece of equipment you are using and slow down. In the beginning, your heart rate will take a long time to recover, but as you train more it will lower more quicklyTry performing stretching during or after your 10 minute cool down is complete. You should hold each stretch for 30 seconds and repeat 3-4 times on each side. Only stretch to the point where you begin to feel resistance. It should feel a little uncomfortable, but it should not hurt. Supine Exercises Exercises lying on your back, allow the blood pressure to remain even throughout the body. It also enables you to be able to build strength without cardiovascular compromise. The standing exercise for calf muscles should be done, when tolerated to aid the calf blood flow pumping mechanism. Mixed Postural Exercises Upright Exercises Leaning forward, pivoting through the hip in exercise 2 and 3, will lead to better hamstring, gluteal and quadriceps engagement. The Sideways Lunge should only be down once the Reverse Lunge is perfected. The use of a slider on the floor and progressing from reverse lunge, to diagonally sideways lunge and eventually sideways lunge may need to proceed lunges with steps and certainly before forward lunges. Aim, is to re-orient the motor learning systems to efficiency of movement both metabolically and mechanically. Monitoring your Heart Rate We recommend you purchase a heart rate monitor set (a watch with a chest strap) to monitor your heart rate during cardio exercise training soyou can exercise in the proper heart rate zones. These can be found online or at a large sporting goods store. You do not need to purchase anexpensive model. Each cardio workout is prescribed to be within a specific heart rate range (see Training Guidelines sheet from your healthcareprovider), and it is important that you complete the workout in that heart rate range. You may notice that your resting heart rate decreases withtraining. Or, it could be unchanged, but your heart rate response to upright posture is lower.TIPS:• Some monitors work even while swimming in the pool.• If you ever question what the monitor is reading (equipment can go bad or need new batteries), simply feel your pulse at your neck or wrist andcount the beats for 15 seconds and multiply by 4 (heart beats per minute). If you are unsure how to take your heart rate this guide can help you:§ http://www.move.va.gov/download/NewHandouts/PhysicalActivity/P09_HowToTakeYourHeartRate.pdf Long Term Maintenance Cardio Training Months 6-8 of training is different for each person. Some people choose to maintain the level of training laid out in Month 5 forever, but we recommend trying to push forward. After you have completed the program you should continue to exercise to maintain what you have worked for. During this time you can use whatever modes you enjoy most. High intensity interval training, is a fancy name for the training that begins in calendar Month 6. It has been shown to provide great benefits to the heart and lung’s response to exercise for healthy individuals and several patient populations. We have found it to be beneficial to patients with POTS when it is introduced at a time when they are ready for it and responding well to their training. Here is an example of this training- Step 1: 10 minute- warm up to get your HR up to Base Pace zone- Step 2: 1 minute- go “all out”, hard and fast, increasing the resistance and speed on the mode you are using, and trying to get your HR upto your race pace zone- Step 3: 1 minute- remove all resistance, slow down, and actively recover. Take this time to get a drink, but keep moving on the piece of equipment. It doesn’t matter what your HR gets down to.- Step 4: Repeat steps 2 and 3 for two to three more trials- Step 5: 10 minute cool down- Step 6: 20 minute Recovery workout. TIPS: • Begin with the upright bike, rower, or elliptical as these are safer than the treadmill for interval training. Try to treadmill only when you are ready.• You can add any strength training you want, and try other things like yoga, aerobics classes, returning to competitive sports as you feel able (we do not recommend any exercise in the heat).• Consider yourself on a path to wellness and do what you feel you can do! We often hear that symptoms continue to decrease with long term training.• Remember each patient progresses through the program to upright exercise at a different pace and that is okay! What to Expect Getting Started This program is not an easy fix to having POTS, and if exercise made everyone feel better in a matter of weeks, everyone would be doing it. The real results will be seen after several committed months of training. The first month may be very difficult, and you may feel increased fatigue during this month. This is not surprising, so do not give up! You are challenging your system to do things it CAN do, but is not USED TO doing. The second month may still be tough. The hope is that you’ll feel less fatigue, begin to sleep better, and suffer from fewer POTS symptoms in your daily life than you did before beginning the training. This is the goal!!! TIPS: • Your commitment and mental toughness are key.• When you begin with a new mode of training, it is not uncommon to feel increased fatigue. Listen to your body. Push forward when you can, or repeat a week if you feel you need to.• If you are anything like the individuals we’ve met with POTS, you probably do not feel good most of the time, and have tried several other things to make your condition better, Here is the question we are proposing to you: Why not give this program your utmost effort for 3-5 full months before deciding if it helps you or not? Remember the benefits of training occur after months of training and not just days or weeks.• Write down a list of things you want to resume in your life, tape it to your bathroom mirror, and read it every day. Read it especially on the days you do not feel like going to the gym - allow it to help motivate you to get your quality of life back.• Get a workout buddy if you need one! They can’t follow your heartrate zones, but they can work out with you!• Ensure your family is on board with supporting you in this journey. Help them understand you may feel more tired in the beginning, but the hope will be to feel better in the long run.• Family support is important, but YOU need to be the one to take the responsibility to make this change happen. Exercise as Your Lifelong Therapy If you feel that exercise is helpful for you in any way, maintaining exercise will then be important for you to keep the benefits and continue to see further improvements in your health and quality of life. Furthermore, you will experience the benefits of regular exercise in many other areas of your life and health, as well. Many patients successfully resume caring for their children, full-time work, full-time school, or enter college when previously they thought that these things might be impossible. We sincerely hope that this is the case for you as well. Keep in mind that according to the American College of Sports Medicine (ACSM) every healthy adult should perform 30-60 minutes of exercise more days than not. Most of ourpatients adopt exercise as part of their daily personal hygiene program. Some patients feel that daily exercise is needed to avoid developing symptoms again. If you have an illness, setback, or quit exercise, and realize that you felt better while training, this is actually a good sign! Do not be discouraged. You have a good response to exercise and you know that it makes you feel better! Just start again. You likely need to begin with horizontal modes of training, but you will know how to progress yourself through the program again. Physiotherapy Physiotherapy can consist of 'hands on' mobilisations of the spine, thoracic rings, myo-fascia as well as guidance and feedback on exercise execution and progression. Additionally, the application of lumbar mechanical traction can lead to mobilisation of the thorax and it's peripheral sympathetic ganglia. Moreover, the post traction exercise protocol, reinforces the mode of action of the postural stabilisers and spinal mobilisers before a person gets up from the treatment table. Post Traction Exercises are essentially those described above, whereby abdominal and bridging exercise in supine are complemented with oscillations of the pelvis and hips. From Supine, exercises in side lying, then in 4 point kneeling, are followed by isometrics in sitting and finally oscillatory movements in standing, including the wall plank, queen mum and Alexander breathing exercises. Supine exercises can also include Pilates style hip and core stability, as well as simple cycling. These have some cardiovascular conditioning effect as well as promote blood flow from the calf. Uploaded : 15 November 2021 Updated : 2 February 2022 Read More -

Types of Exercise
What types of exercise are there? and what are the differences? If you’re looking to introduce more exercise into your routine, you might be a bit confused by all the different exercises out there. Which ones should you be doing? We’ve created this guide to help you make sense of it all! What types of exercise are there? There are four main types of exercise that you need to know about: ● Aerobic exercise - a workout that speeds up your heart rate and breathing● Strength exercises - building muscle mass● Stretching - maintaining flexibility● Balance exercises - improving your, well… balance! Aerobic exercise Aerobic exercise has a lot of all-round health benefits, and everyone should aim for 150 minutes of moderate intensity or 75 minutes of high intensity aerobic exercise every week. Some of the benefits of aerobic exercise include:● Improved heart health and reduced risk of heart disease● Lower blood pressure and reduced risk of heart attack or stroke● Weight management● Reduced blood sugar levels and reduced risk of type 2 diabetes● Improved brain function and reduced risk of dementia● Improved mood and reduction of depression and anxiety You can get aerobic exercise from walking, running, cycling, swimming, dancing or specific aerobics classes. Strength exercises Strength training isn’t just for body builders - as we age, we all lose muscle mass, so it’s important to build it back up. Muscle strength is vital for a number of everyday tasks, like carrying shopping, picking up heavy objects, and even standing up from a chair or walking up stairs. Strength training helps to:● Stimulate bone growth, reducing your risk of fractures or osteoporosis● Reduce stress in the lower back and joints● Improve posture● Manage chronic conditions like arthritis, back pain, diabetes, heart disease and depression● Make you - surprise! - stronger Some examples of strength training include free weights, weight machines at the gym, resistance training, and body weight exercises (such as push-ups, pull-ups, planks and squats). It’s a good idea to get advice from a physiotherapist before you introduce a strength training routine, particularly if you have any health concerns. Stretching Stretching is vital for reducing the risk of injury from other types of exercise, and can be a valuable part of injury recovery, but it also has a lot of benefits of its own. Regular stretching lengthens your muscles, which helps to prevent muscle cramps and pain, muscle strains, joint pain, and falling. It also keeps you flexible, which increases your range of motion and enables you to do everyday activities like bending down to tie your shoes. There are a huge number of different stretches you can do that all target different areas, so have a chat with us to figure out the best ones for you. Balance exercises As you get older, the systems within your body that control your balance begin to break down. Balance exercises are important to help to reduce the risk of falls and keep you steady on your feet. A physiotherapist will help you determine your current level of balance ability, which is really important for figuring out which exercises you need. Exercises like standing on one foot, walking on uneven surfaces, leg lifts or standing knee lifts can help with balance, but your physio will recommend the ones that will best suit you and tell you how to do them safely. We can help you with advice on the types of exercise that you need, particular exercises that you can do and the right techniques to get the most out of your routine (and avoid injuries). Give us a call or email us. References 1. Brukner, P. and Khan, K. 2017. Clinical Sports Medicine. Australia: McGraw Hill Education2. Harvard Health Publishing. 2019. The 4 most important types of exercise [Onlinehttps://www.health.harvard.edu/exercise-and-fitness/the-4-most-important-types-of-exercise3. Medical News Today. 2019. What are the benefits of aerobic exercise? [Onlinehttps://www.medicalnewstoday.com/articles/327100 4. Mayo Clinic. 2021. Strength training: Get stronger, leaner, healthier [Onlinehttps://www.mayoclinic.org/healthy-lifestyle/fitness/in-depth/strength-training/art-20046670 Uploaded : 4 November 2021 Read More -

Skier's Thumb
What is Skier’s Thumb? The terms Skier’s Thumb and Gamekeeper’s Thumb both refer to injury of a ligament at the base of the thumb. The ligament is called the ulnar collateral ligament (or UCL). Whilst Gamekeeper’s Thumb refers to a chronic condition caused by repetitive stress to the UCL (think using a wrench or wringing out cloths), Skier’s Thumb is an acute injury, usually caused by a fall. What causes Skier’s Thumb? Skier’s Thumb usually occurs when a person falls on an outstretched hand whilst holding something - ski poles will do it, which is how the injury got its name. However, football, hockey, basketball and rugby can also be culprits. Falling from a bike or motorcycle is actually the most common cause, and even a firm handshake can sometimes be enough to rupture the UCL! The force of impact while the thumb is extended is what causes the damage. What are the symptoms of Skier’s Thumb? Skier’s Thumb accounts for 86% of all injuries to the base of the thumb, so it’s a common problem. If you’ve developed Skier’s Thumb, then you’re likely to experience the following: ● Pain at the base of the thumb or in the web space between your thumb and index finger● Swelling at the base of the thumb● Tenderness to the touch● Weakness in your grip● Bruising around the thumb● Pain in the wrist (referred pain from the injury site) How is Skier’s Thumb treated? How your injury is treated will depend very much on the severity. Mild injuries may only require stretching and pain relief techniques. More serious injuries might require immobilisation for a period, whilst very severe cases may need surgery. When you come to see us, we’ll assess the damage and determine whether the ligaments have been torn or just stretched - and if they have been torn, to what degree. Elevation and cold compresses can help to reduce swelling and bruising, and if necessary, we will apply a thumb cast to immobilise the joint while it heals. Once the cast comes off, we can show you exercises to help build your strength and flexibility in the joint. If you do require surgery, we will help you afterwards to regain the function in your thumb and grip, and to shorten your recovery time as much as possible. If left untreated, damage to the UCL can lead to long-term weakness and joint instability. So, make sure you get it checked out! How can Skier’s Thumb be prevented? If you’re a regular skier, sports player or (motor)bike rider, there are a few things you can do to reduce your risk of Skier’s Thumb: ● Make sure you’re using the proper technique for any equipment, like ski poles, hockey sticks or carrying a ball - get instruction from an expert● For skiers, you can train yourself to release your pole as you fall, meaning you’re less likely to land on an extended thumb - you can also get special gloves to help with this● Wearing ski gloves or sports gloves can protect your thumb joint in case of impact References 1. Physiopedia. 2021. Skier’s thumb [Online https://www.physio-pedia.com/Skier%27s_thumb]2. Brukner, P. and Khan, K. 2017. Clinical Sports Medicine. Australia: McGraw Hill Education Uploaded : 4 November 2021 Read More -

Exercise and Ageing
Exercise and Ageing - a personal perspective and literature review Martin Krause What constitutes successful ageing? Maintenance of health, both cognitively, psychologically and physically. Remaining engaged with people, being curious, regular endurance and strength training, as well as getting out into nature. Ideally exercise is a life long undertaking. The following is a personal perspective of my own professional and private experiences from elite and professional sport to treating centenarians, in a private practice setting, as a physiotherapist. Hopefully, my personal perspective doesn't appear to be an exercise in narcissism, but rather an expose of my thoughts and feelings on successful ageing.. I have exercised almost all my life. I grew up in a household without a car. My parents bought their first car in the 1980's after I had finished school. My grandfather also didn't own a car. He walked everywhere. When I visited him in Germany, in the 1970's, a 30km walk was a normal thing to do. We even caught trains to some distant place and walked back through forests and along quiet country lanes. Unfortunately, he passed away at 73 years of age. His son, my father, is currently 83 years old, and also seems to have this long distance walking ability, as does his cousin in Germany who, at 84, just spent the previous European summer walking in the Dolomites and Alpes, 20-30km per day, which even involved going up 3000m mountains. So what is the elixir of successful ageing? South Tyrol Active transport Having grown up, always being reliant on 'active transport', I became a great believer in running and cycling everywhere I could. I discovered long distance cycle touring and orienteering around 13 years of age. Around 14 years of age, a friend and I commenced pack cycling in the school holidays, catching over-night trains several hundred kilometres away and cycling home from various places in Australia - in both heat/drought and cold (snow in the Blue Mountains). Cycling up to 300km in a day and doing Alpine marathons and 100km trail runs, as a young adult, in Switzerland. Sport took me all over the world, to see incredible places, and meet amazing people. Some of these people were astonishingly old, such as Swiss and Swedish centenarians doing orienteering in the sleet and snow of the Czech Republic, others were dour Colombians and Cubans, who in their 70's, decided to accompany me for parts of my cycling trips, let alone the guy with just one leg - a below knee amputee, in Cuba, who rode with me for a couple of hours, telling me about his grandchildren! Genetics or epi-genetics? Genetics or epi-genetics? My mother died of throat cancer at 79 years of age, whereas my grandparents died of heart failure. On both sides of my family there was a mixture of ancestors dying both old and young (great aunts and uncles dying in their 30's and 40's). My mother and grandmother survived death marches and the camps at the end of WWII, and they lived to around 80, whereas, their siblings, who were spared 4 years of terror and deprivation, lived into their 90's. Notable, they were all still active as they aged, either riding their bicycles to do the shopping or still getting farming awards for the districts (Norfolk, UK) biggest pumpkin. What they seemed to have in common, is that they also didn't seem to over-consume, in terms of calorific intake. However, they all had type II diabetes and very high blood pressure problems as well as chronic low back pain. Cognitively, they were still 'sharp' well into their 90's. Psychologically, they were a generation who grew up with hardship, expected little, and were grateful for every day, seeing 'life itself' as a bonus. Endurance vs Short Distance Intensity Now, I'm closer to 60 than 50. I still ride bicycles and run. However, long distance endurance activities have given way to short sharp fast activities. I took up 11 aside football (soccer) at 50 years of age, downhill Enduro mountain biking around a similar time. Traditional rock climbing is the most endurance oriented activity I do, which I took up in my mid 50's, as well as bouldering and some sea kayaking. My bike training involves 90 minutes of steep hills, to coincide with 90 minutes of football. Speed over endurance, seems to mean that the occasional adventure race of cross country marathon distances, only requires this speed training activity. At soccer, I'm still one of the fitter and faster ones in the O35 category, meaning I'm playing against people up to 20 years younger, albeit in a low division. This was not what I had expected when I was younger as I was taught, at university, "as you get older, your wear out", Tell that to my 98 year old client, with a rotator cuff injury (from a decade of lifting his wife in and out of the wheelchair), whose doing 'down facing dog' and high planks from yoga! Hatha Flow Yoga is another thing I took up in my 50's, where flexibility and stability meets deep breathing calm intensity. Cardiovascular deficit is thought to be a common mechanism of different types of cognitive decline. Retinal fundus photography has been proposed as a measure of cognitive decline, as narrow arterioles and wider venular diameters is associated with reduced cognitive dysfunction (with/without dementia). In a longitudinal 6 month trial, using marathon running and chronic exercise adaptation from acute bouts of exercise, investigators were able to demonstrate positive changes to arterial vasculature, as well as cognitive function. Importantly, neither acute exercise nor regular exercise fosters these adaptations, on their own, however it is the combination of the two, which stimulates vascular changes and cognitive function (Roeh et al 2021 Med Sc Sp Ex, 53, 10, 2207-2214), The effect of exercise on blood pressure Cardiorespiratory Fitness (CRF) and Muscular Strength (MS) are independently associated with reduced odds of having high Arterial Resistance (AS) in older adults (Albin et al 2020 Med Sc Sp Ex, 52, 8, 1737-1744). Both 'fit and weak' as well as 'unfit and strong' groups demonstrated reduced AS. Moreover, an additive affect seems to occur combining greater strength with better cardiovascular fitness. These results need to be treated with caution as low BMI in the 'fit and weak' group may actually be a pre-cursor to chronic disease. Investigations, I undertook into Sarcopenia, strongly suggest, that the maintenance of muscle mass is critically important, to the immune and metabolic systems, as the protein reservoir residing in muscles can be used by the immune system, whilst the muscles themselves act as a metabolic 'glucose sink' via glut 4 receptor sites. See elsewhere on this site for further information. Respiratory resistance training has also been advocated for reducing AS. Investigators found that when compared to the control group, systolic and diastolic blood pressure decreased significantly with unloaded breathing by means of 7.0 mmHg (95% CI 5.5 to 8.5) and 13.5 mmHg (95% CI 11.3 to 15.7), respectively (laboratory measures). With loaded breathing, the reductions were greater at 18.8 mmHg (95% CI 16.1 to 21.5) and 8.6 mmHg (95% CI 6.8 to 10.4), respectively. The improvement in systolic blood pressure was 5.3 mmHg (95% CI 1.0 to 9.6) greater than with unloaded breathing. Heart rate declined by 8 beats/min (95% CI 6.5 to 10.3) with unloaded breathing, and 9 beats/min (95% CI 5.6 to 12.2) with loaded breathing (Jones CU, et al 2010. An inspiratory load enhances the antihypertensive effects of home-based training with slow deep breathing: a randomised trial. Journal of Physiotherapy 56: 179–186). Read further.. From a personal perspective, higher intensity exercise seems to improve my muscle strength and agility, whilst encouraging deeper breathing. Flow style Hatha Yoga also encourages deeper breathing along with muscular stability and flexibility. I find that, when comparing the beginning to the end of a yoga session, I feel I'm breathing three times deeper!! Kayaking adds to my thoracic flexibility and abdominal length and strength, thereby freeing the diaphragm, whose myofascial attachments, to the hip flexors, allows for protective mobility around the abdominal aorta and vena cava. However, I still grapple with blood pressure issues. BMI Body mass index seems to also play a pivotal role. Too much weight versus not enough weight - endomorph vs ectomorph. Too little muscle mass versus too much 'puppy fat'. In my early 20's, when i was highly competitive, with elite orienteering and road cycle racing, my ideal body weight was 73kg and when I wasn't as fit, it went down to 69kg. Now I hover around the 76kg range, whilst being 188cm (6'3'') tall. We know that belly fat increases insulin resistance. We also know optimal exercise improves the power to weight ratio. Optimal Exercise What constitutes optimal exercise? In my experience, there is nothing healthy in elite exercise. Blinded one eye dogged determinism to achieve some form of 'singularity' at an 'event horizon' certainly is seen as a noble attribute, steeped in the history of 500 Spartans fighting an entire legion of Romans, gold medals at the Olympics and other heroic feats of athleticism. Whilst, creating a great story, which can mobilise an entire generation to become active, as was seen in Spain after the Barcelona Olympics, it can come at a price in some athletes. During the Sydney Olympics, I was talking to the dentist at the Olympic Village Medical Clinic and he stunned me, when he told me that some of the American athletes had borderline scurvy and gum disease let alone poor teeth. He felt that, although they were often on college scholarships, they were trained hard, and only good for one Olympics!!. Only good for one Olympics is what Charlie Walsh, the legendary Australian track cycling coach, said in Adelaide (2009), as the toll on the body, was too severe to expect more than an Olympics and maybe a World Championships out of an athlete. High Desert, Argentina 1990 - on the way to Passo de Aguas Negras I started long distance cycle touring, or pack cycling, at 12 years of age. At 26 years of age, school friends and I cycled half of South America on the very first versions of Mountain Bikes. Altitudes of up to 5000m, temperature in access of 50C during the day, below zero at night, bikes weighing 30-40kg, due to the need to carry spare parts, food for up to 10 days, water for 2-3 days. An amazing experience on the back of a lifetime of endurance training. We now know, that such extremes can lead to heart damage (Cardiomegaly), stress fractures, skin cancers, excessive weight loss, etc. I remember a client, the late Hilton Harris, who I had known in Wentworth Falls, in the Blue Mountains. He was 99, and still played 10 rounds of golf. He even bought a house at the top of the 2nd fairway. He told me that the secrete to musculoskeletal longevity were a 'good pair of boots and a good pair of socks' and don't do anything in the extreme. Another 97 year old client, the late Mr McAlpine, was still playing competitive lawn bowls and he felt that 'active exercise had to be interactive'. Dolf, the 95 year old Swiss Orienteer took up serious, regular, cross country skiing in his 60's, because a doctor told him that it would be good for his chronic low back pain. He even went as far as to buy a farm house in Kandersteg to do so. He was recently interviewed on Swiss National Television. Currently, I have an ex Naval Admiral, who at 98 years of age, is looking to buy a treadmill for his home, and whom I've gotten to a point where he is doing 'down facing dogs', high planks and 'up facing dogs' from yoga for his rotator cuff injuries. He was on a British Battle Cruiser. The Repulse, which was sunk off Singapore, 3 weeks before it fell to the Japanese in WW!!. He has a remarkable attitude to life. What I find with the current half a dozen or so centenarians whom I'm treating, is that they are cognitively incredibly astute, can hold a conversation, still have that curiosity to learn new things and are socially adept and active. None of them had easy lives, surviving war and the great depression. The late Margaret Palmer, was still travelling the world until 98 years of age. At 95 she went to French language school for a month in Strasbourg. The teacher even took her to an Etappe of the Tour de France. At 96, I suggested she go to Hakone hot springs in Japan - which she entertained but ended up going to Hamner Springs in New Zealand instead. Muscle memory Muscle memory is something which has been often talked about, but remained only anecdotally proven. I came to fatherhood, late in life. I was 40 when my son arrived. Because, my wife and I, were surrounded by much younger people, we adapted our physical activity to accommodate the younger mindset. When my son was 5 years of age, I commenced coaching his soccer team, which I did till he was 12. During that process of teaching kids every trick, I realised that, although I wasn't a good player when I was young, I was very good at learning how to do things when I was older. Attention to detail and technique are some of the benefits of teaching. This lead me into playing full 11 aside soccer at the age of 50. In the same year, when I turned 50, I participated in the Quebrante Huesos cycling Etappe (205km, 4000m climb) in the Pyrenees, with Angel and an ex Tour de France cycling buddy of his, from Barcelona. I cycled back to Barcelona over 5 days after the event. Some 800km and 17000m of climbing later I decided that long distance cycling was no longer for me. Although a great and unforgettable experience, where I met lots of really interesting people, both on the road and in hotels, I'd realised this was too much. Many of the French people I met were curious about 'le Kangaroo avec la sac a dos'. Quite often I was seriously late for the Plat du Jour, where in one instance, the barman looked at me and said 'I suppose you'll eat anything!". He made me the worlds biggest baguette and in the same establishment, I met a young couple from New York, whom at a whim, bought charter flight tickets to an airport near Barcelona so they could walk the entire length of the Pyrenees. The girl was the instigator of their adventure, full of expression and excitement and wanting to know more about my adventure, whereas the boy looked like he was about to die. Ironically, I was probably looking at my own reflection, because how he looked, was the exhaustion I was feeling. I will never forget that moment, which is etched into my memory. Muscle memory is probably a combination of neurophysiological-cognitive factors as well as muscle - immune peptides. Researchers have found that exercise induces different molecular responses in trained and untrained human muscle (Moberg et al 2020 Med Sc Sp Ex, 52, 8, 1679-1690). Their findings demonstrated that several key regulatory genes and proteins involved with muscle adaptation to exercise are affected by previous training history. I consider the human evolution out of Africa as a classic example of using our muscles to propel us forward, hunt and gather, whilst encountering new pathogens and dealing with injuries on the way. Could the long distance cycling experience, or the objective of ageing, also be a journey of survival? The interactivity of group activity, leading the cycling peloton amongst friends may presumably drive the immune response, whilst the gym workout, maintains the strength needed for the endurance activities to take place? Fine tuning the immune response of muscles through exercise Community . Hunter and Gatherer - Nomads Arresting cognitive decline Arresting cognitive decline is a key ingredient to successful ageing. Dr Phil Cremer, neurologist at RNSH, has often told his clients to walk every day to help prevent cognitive decline. Exercise is perhaps one of the best preventatives of cognitive decline due to the thermogenic nature of it's activity. The Laws of Thermodynamics, conservation of energy, and oxidative stress are all at work within the musculoskeletal system. Together with the brain and gut, these sensors unleash the most powerful immune regulatory system. The human gut has more species and biota than there are stars in the universe. The muscle energy metabolism establishes a symbiotic relationship with the gut energy biota, whilst the brain drives the muscles in the need for the acquisition of food. In our 'hunting and gathering' days, this was all nicely balanced out, today we can order our groceries and even pre-prepared food, on-line. Essentially, stress of hunger and hence hunting, was dealt with, by the immune system interacting with the brain, muscles and gut. How does the immune system deal with stress in the modern world and without physical and interactive social activity, is it this, which drives cognitive decline? Group activity, exercise and cognitive responses The more we feel cognitively and physically in control within our environment, the 'Goldilocks' sweet spot of stress can be found. Allostasis is our ability to adapt to various psychological and physiological stressors. Cycling through extreme heat and altitude in South America with some dehydration and calorific compromise might be just such an allostatic process, whereby, in my case. I adapted nicely due to my prior training background and because I was with friends. Whereas, my OTT Pyrenees cycling experience, I actively sort out company, as the trip back to Barcelona was on my own. I wonder whether my mother, at 6 years of age, would have survived on her own, if she weren't with her 8 year old brother and later their mother during WWII? Their mother definitely wanted to end their lives by jumping into an ice crater (January 1945), created by a bomb on the frozen river, only that her children protested 'wir wollen leben' - we want to live. Exercise activates key cellular energy sensing pathways which can directly and indirectly influence other hallmarks such as glutathione (GSH), and vascular endothelial growth factor (VEGF). Brain Derived Neurotrophic Factor (BDNF) release improves glial cell activation and modulation of inflammation, increases neurogenesis and neuronal connectivity, improves neural stress response, calcium homeostasis and DNA repair. Furthermore, habitual exercise improves regulation of oxidative stress and general central nervous system mitochondrial function and regulation (Wahl D et al 2021 Novel Strategies for Healthy Brain Aging. Ex Sp Sc Re, 49, 2, 115-125). Aerobic fitness and cognition As mentioned earlier, a lot can be learnt through the assessment of the eyes. Spontaneous eye blink rate (sEBR) mediates the association between aerobic fitness and executive function through pre-frontal aerobic efficiency via a brain dopaminergic functional pathway (Kuwamizu et al 2021, Med Sc Sp Ex, 21, 7, 1425 -1433). Stress makes us blink! Orienteering is a very good sport where the demands of moving through terrain are both physical and mental. Belonging to an orienteering club is like belonging to a big family. Moreover, people can do this sport into their 90's. Read more ... Contextual memories, health, allostasis and muscular immune response Successful ageing isn't for the faint hearted. A myriad of musculoskeletal and health issues can arise, as well as questions of ones own self-worth in a tribe. From my anecdotal and professional experience, I would be inclined to say that the best way to age successfully, is through group physical activities which are cognitively engaging, stimulate the muscle-immune-brain-gut axis and take people on a journey of self discovery and ideally involve nature. Uploaded : 30 September 2021 Updated : 07 November 2021 Read More -

Osgood-Schlatter Disease : Osteochondritis Dissecans
Osgood-Schlatter disease Despite the name, Osgood-Schlatter Disease (OSD) is not a disease at all - it’s a common knee injury that affects children and teenagers. If you thought that “growing pains” were an old wives’ tale, then think again. Growth spurts in adolescence can cause a number of painful conditions, and OSD is one of them. What is Osgood-Schlatter Disease? Children have a lot of growing to do, which means their bones, muscles and tendons have a lot of growing to do too! To enable this process, many of the bones have a growth plate, which is a soft area of cartilage at the ends of long bones. The shinbone is one such bone. During puberty, when the muscles, bones and tendons are all growing at different rates, the tendon that connects the shinbone to the kneecap can pull on the growth plate at the top of the shinbone. Since this is also a time when children are particularly active - playing sports, playing with their friends, and generally running around and jumping about at any opportunity - the tendon can be further stretched by frequent repetitive movements. All of this causes swelling and irritation, known as Osgood-Schlatter Disease. In 1903, an American orthopaedic surgeon called Robert Osgood and a Swiss surgeon called Carl Schlatter both independently described the condition, and it was named after them both. What are the symptoms of Osgood-Schlatter Disease? OSD usually affects children between the ages of 10 and 15. It is more common in boys than girls and can happen in one or both knees. If your child has OSD, they will likely experience some or all of the following symptoms: ● Pain in their knee that gets worse with physical activity● Pain in their knee when running, jumping, squatting, kneeling, walking upstairs, or walking up hills● Tenderness around the knee● Swelling below the kneecap How is Osgood-Schlatter Disease treated? If left untreated, the pain from OSD can last a very long time. The good news is that OSD will go away altogether once your child stops growing, but until then it can cause a great deal of discomfort, so it’s important to give your child the best possible treatment while it’s occurring. Rest is important, and your child will most likely be advised to either limit or modify their level of sports activity for six to eight weeks. After that time, they may continue to participate in their normal activities as long as they rest if the pain becomes too severe and the pain subsides after a day of rest. If it doesn’t, they’ll need to be checked out. You should also watch out for any signs of limping or difficulty walking after activity. Ice application after activities can reduce the pain, and stretching the quadricep and hamstring muscles is important. As this condition is caused by excessive pulling of the tendon on the bone, stretching should be gentle and only done when advised by your physio. Foam rolling may also be effective as a form of self-massage for the leg muscles when at home. Your physio can help your child with exercises to strengthen the quadricep and hamstring muscles, and a stretching and warm-up/cool-down routine for sports activities. Our goal is to keep your child active and moving with as little pain as possible. References 1. Physiopedia. 2021. Osgood-Schlatter’s Disease [Onlinehttps://www.physio-pedia.com/Osgood-Schlatter%27s_Disease 2. Johns Hopkins Medicine. 2021. Osgood-Schlatter Disease [Onlinehttps://www.hopkinsmedicine.org/health/conditions-and-diseases/osgoodschlatter-disease3. Kids Health. 2019. Osgood-Schlatter Disease [Onlinehttps://kidshealth.org/en/parents/osgood.html Uploaded : 23 September 2021 Read More -

What is a ligament sprain?
What is a ligament sprain? A ligament sprain is usually caused when a joint is suddenly forced beyond its usual range of movement and the ligament fibres are stretched too far. In some cases, the ligament can be torn. This might be the result of falling, twisting, or sustaining a blow to the area. The most common location for a ligament sprain is the ankle, but they can occur anywhere. What is the difference between a sprain and a strain? You might hear these terms used interchangeably by amateur diagnosticians, but sprains affect the ligaments while strains affect muscles and tendons. They both cause pain, though, so it can be difficult to tell the difference when all you know is that it really hurts! How will I know if I’ve sprained a ligament? Sprains can look and feel like a break, particularly if they are severe, so it can be difficult to tell the difference between the two. You will likely experience: ● Pain● Swelling● Bruising● Limited and/or excessive movement of a joint Some patients report hearing or feeling a “pop” at the time of the injury. What should I do about it? You’ll need POLICE - no, not the ones in blue uniforms, these ones: Protection - avoid further damage to the area through rest and, if necessary, specialist equipmentOptimal Loading – early movement to stimulate healingIce - applying an ice pack for 10 minutes can reduce swelling and relieve painCompression - the use of a compression bandage can help to avoid further swelling Elevation - keeping the area raised reduces swelling and allows waste removal from the injury site A physiotherapist will be able to help you with all of this, as well as supporting you with hands on treatment, exercises, and equipment to relieve pain, restore movement and prevent future injuries. So, your first port of call should be to book an appointment to get diagnosed early and start the recovery process with as little time wasted as possible. References 1. Physiopedia. 2021. Ligament Sprain [Onlinehttps://www.physio-pedia.com/Ligament_Sprain2. Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. McGraw Hill Education: Australia Uploaded : 23 September 2021 Read More -

Orthotics
Orthotics Orthotics can either be “off-the-shelf” standard items that are ready made and adjusted for the patient’s particular size - or custom-made, particularly in cases of more complex injuries or changes to multiple joint structures. Reasons to use orthotics There are a few reasons that your physiotherapist might recommend the use of orthotics. Generally speaking, orthotics are designed to either stabilise a body part, or assist that body part in movement. For example, if a joint is not in a functional position, then orthotics may be used to help it to function better, recover and to prevent further injury during the recovery process. Types of orthotics There are several types of orthotics. Commonly, they can be divided into soft and hard. Both can be molded, but it is more common to mold the hard ones. Both can have inserts, wedges, domes, etc, glued to them. Some are moulded after taking a cast of the foot whereas others are designed after foot platform analysis of weight distribution across the sole of the foot. Commonly, a video is also taken of the rear of the foot at push off. Try soft orthotics first. Inexpensive and frequently enough to fix the problem. Some conditions that might require orthotics include: Back pain - if this is caused by foot or leg problems that are causing uneven gait, then orthotics might help you to walk more evenly and reduce the pressure on your back Arthritis - orthotics can help with positioning of the joints to relieve discomfort Bursitis - when the fluid-filled sacs in the heels and toes become inflamed, they cause a great deal of discomfort which orthotics can help to reduce Ankle sprain – an orthotic might provide support to prevent further injury while you recover and to allow you greater movement Achilles tendonosis - take tension off the achiilles tendon esp at the insertion of the heel and it's bursa Inside knee pain - reduces the amount of rotation on the inside of the knee as the first joint of the foot is a 'ball and socket' joint. Outside hip pain and bursistis - again aids in control of rotation Common mistakes with orthotics Orthotics can be incredibly valuable tools in your recovery, but only if they’re used correctly. There are a few key mistakes that people regularly make, so we want to help you avoid them! ● You need to wear them in gradually It will probably take two to three weeks to get completely used to wearing your orthotics and, except in serious cases or unless your physiotherapist tells you differently, you will need to gradually build up the amount of time you wear them each day rather than wearing them full-time from the offset. ● You must follow your physiotherapist’s instructionsWe know it can be a hassle to have to put that wrist support on every time you play sport, but it really is important. You need to wear the orthotics in the right way, at the right time, for the right amount of time, or they may not work as effectively as they could. Your physiotherapist has given you those instructions for a reason, so it would be advised to follow them as best as possible. ● Don’t give up on them as soon as you’re feeling betterBecause it can be a hassle to keep putting them on, or because people don’t think they look particularly attractive, or because they might not be incredibly comfortable, many people are keen to ditch their orthotics as soon as possible. But just because the pain has subsided doesn’t mean the problem’s gone away. If you give up on them too soon, the problem might come back or get worse. So don’t put them away until your physiotherapist gives you the go-ahead. When you’re experiencing pain, we’re happy to talk you through all the different treatment options available, including what types of orthotics might work for you alongside our hands-on and movement / exercise-based treatments (but only if needed of course!). Give us a call on or email and we can discuss your choices. Take a look at my research - barefoot running vs orthotics : EMG and joint angle analysis read more.........see link below see https://www.back-in-business-physiotherapy.com/orthotics-and-gait.html Uploaded : 26 August 2021 Read More -

Plantar fasciitis
Plantar fasciitis If the plantar fascia becomes acutely inflamed, this is a condition called plantar fasciitis (‘itis’ = inflammation in scientific talk). This is most common in runners, and accounts for around 10% of runner-related injuries. The repetitive movement of the foot in running, particularly when you run on hard surfaces, makes this band of tissue highly susceptible to overuse. New runners who try to do too much too soon, or those who suddenly change their running regime, can also excessively strain or tear the plantar fascia. Plantar fasciosis This is a degenerative condition, which is caused by the plantar fascia deteriorating under repetitive stress. This is almost like a second stage plantar fasciitis, where if you leave the initial symptoms untreated, the condition can progress to a chronic issue where degeneration of the tissues is the main feature. Any cause of a plantar fascia problem that develops from an acute to a chronic stage can fall under the label of plantar fasciosis. Just like running can cause fasciitis, it too can lead a person into fasciosis if left for too long. Other causes include being sedentary, overweight and regularly wearing high heels for prolonged periods. People who have excessively flat or arched feet are also at risk of developing these problems . What are the symptoms of plantar fasciopathy? Whichever type of plantar fasciopathy you have, you are likely to experience similar symptoms. These include: ● Heel pain, particularly when walking after a long period of inactivity (a classic symptom includes pain on taking those first steps in the morning after waking from sleep)● Tenderness in the heel area● Difficulty bringing your toes towards your shin● Pain when climbing stairs or walking on hard surfaces If the pain in your foot occurs shortly after a sudden increase in activity, then it’s very likely to be plantar fasciopathy, but let us take a look at you and we will be able to let you know exactly what is happening. Plantar fasciopathy is most common in people aged between 45 and 65 and is slightly more common in women than men. But anyone can experience it at any time. How do we treat plantar fasciopathy? If left untreated, plantar fasciopathy can cause pain for a very long time (most cases last at least six months), and, because the pain can cause you to alter the way you walk, there is a chance of further, potentially more serious, damage being caused. So, it’s best to see a physiotherapist as soon as possible. Some form of rest or alteration to your normal routine is important, particularly for plantar fasciitis, and we’re likely to tell you to take a temporary break from running or other sports that may lead to continued excessive load being placed on the tissues, and ultimately, delayed healing. We can massage the arch of the foot and other areas of the body including anywhere from the low back to the foot, to help relieve the pain and restore some movement. There are also a number of stretches and strengthening exercises that we can work with you on to help rehabilitate the plantar fascia and any other underlying causes. We may also recommend shoe inserts, orthotics or night splints to support the area while it recovers. Read more...... In the vast majority of cases, treatment and time will be enough to combat the issue. However, in more severe cases, we may explore options such as shock-wave therapy and various types of injection into the local area of tissue. We will always aim to follow a conservative approach before making use of more invasive techniques. If you think you might be suffering from plantar fasciopathy, or you want to avoid experiencing it in future, give us a call or email to find out what we can do to help. A tight calf and Achilles issues can also be a contributing factor : read more......... Uploaded : 24 August 2021 Read More -

Muscle Stretching
The Benefits of Stretching We keep telling you to stretch before and after exercise, until you’re probably sick of hearing about it. But why? Well, there are a whole host of benefits to stretching, and they’re not just limited to exercise. Here are seven reasons to make sure that proper stretching is a regular part of your routine. 1) Reduced risk of injuryStretching warms up your muscles, increasing the range of motion, so they are less likely to be torn or strained during exercise. You are also less likely to experience pain or discomfort after exercise with a thorough warm up and cool down. 2) Increased flexibilityFlexibility not only improves your performance but is good for your overall health. Increasing your flexibility will also help to delay decreased mobility as you age. 3) Improved postureTight muscles, especially in the chest, back and hips, can cause poor posture, which can lead to pain or injury. Stretching keeps your body in better alignment and improves your posture. 4) Reduced stressYour muscles tighten in response to physical and emotional stress, and many of us hold tension in our necks, shoulders and upper backs. Stretching these muscles helps to release the tension and helps you to relax. Stretching also provides an opportunity for a moment of mindfulness to calm your mind. 5) Increased circulationStretching improves blood flow to your muscles and joints, which enables them to get more oxygen and nutrients. 6) Enhanced performanceA flexible joint can move through a wider range of motion with less energy, so stretching makes your body more energy efficient. By preparing your muscles for exercise through stretches, you are improving your performance. 7) Fewer headachesAs a great many headaches are caused by tension, releasing that tension through stretching can reduce the number of headaches you experience. If you’re interested in which stretches will suit you and want help putting a program together to compliment your activity habits, give us a call on 02 9922 6806. We’d offer to do the warm up on your behalf, but that’d be a stretch! See what we did there? Uploaded : 23 July 2021 Updated : 7 April 2022 Read More -

Frozen Shoulder
What to do about a frozen shoulder Adhesive capsulitis, more commonly known as a ‘frozen shoulder’, is a painful condition that is characterised by stiffness and a loss of motion in the shoulder. What causes frozen shoulder, what can you do about it and how can you stop it from happening in the first place? Let’s take a look! What is a frozen shoulder? The tissue that surrounds the shoulder joint and holds it together is called the capsule - when this becomes inflamed, this band of tissue becomes stiff, which restricts the movement of the shoulder. There is no clear cause of frozen shoulder, however hormonal imbalances, diabetes or a weakened immune system can make you more susceptible to joint inflammation. Long periods of inactivity following injury, illness or surgery also increase the chance of a stiff shoulder joint. What are the symptoms of a frozen shoulder? If you develop adhesive capsulitis, you are likely to experience symptoms in three stages across a period of approximately 1-3 years. Initially, the shoulder will be intensely painful, and any movement will cause pain. At this stage, movement begins to become limited. The discomfort often leads to avoiding moving the shoulder, which further increases the stiffness. When the shoulder is at its most stiff, pain may reduce somewhat, but movement becomes more difficult. Once the shoulder begins to “thaw”, the range of motion then improves. Many people say that the pain is worse at night and can keep them awake. How do you treat a frozen shoulder? Physiotherapy is the most common treatment for a frozen shoulder. A physio will help you to stretch your shoulder joint to recover the range of motion and will teach you a program of gentle exercises to do at home. While you’re waiting for your physio appointment, putting an ice pack on the shoulder for 15 minutes, several times a day, can help to reduce the pain. Another method, is to place a hot pack in your arm pit. This allows the heat to concentrate deep inside the shoulder joint, acting directly on the rotator cuff muscles. Both heat and cold stimulate heat shock proteins (HSP) which are the basic building blocks of life and the immune system. Hence, important in soft tissue repair as well as the modulation of the immune response. Taking a high concentration of EPA/DHA fish oil can reduce some of the inflammation and improve blood flow. Importantly, it's the 2000mg of the EPA/DHA which is the active ingredient of fish oil. Check the label of your fish oil for this concentration. Additionally, make sure their are low levels of mercury and other potentially toxic ingredients in your fish oil. Other anti-oxidant anti-inflammatories include tumeric, forest berries, etc. If you opt for an invasive procedure such as an injection then this must be done with imaging and go into the joint capsule. Sometimes, a severe subacromial bursitis can mimic a 'frozen shoulder' where an injection could be made there instead. Further differential diagnosis with a nerve condition from the cervical spine should also be undertaken, where a diagnosis of 'frozen shoulder' isn't clear. Normally, the history of gradually worsening, night pain and loss of range of movement with flexion at 60 degrees, abduction at 30-45 degrees, 1/4 external rotation and almost no internal rotation (hand behind back) is usually indicative of a 'frozen shoulder. Testing those movements with the head and neck in lateral flexion (side bending) could help to differentiate a neck pathology contributing to the clinical presentation. Frequently, their a familial (genetic) tendency to 'frozen shoulder'. Whilst teaching in Japan, I saw a lot of 'frozen shoulders' whereas during the 10 years in Switzerland I saw almost none. Who is at increased risk of a frozen shoulder? The following people are at greater risk of developing adhesive capsulitis: Those over the age of 50 Women People with diabetes People with thyroid conditions People with cardiovascular disease Previous shoulder injury Anyone who has to remain still for long periods of time due to illness or surgery Anyone who needs to wear a shoulder sling for a long period of time following an injury What can you do to prevent a frozen shoulder? As immobility is a major cause of a frozen shoulder, if you suffer an injury or illness that will keep you out of action for a while, speak to a physiotherapist about exercises that you can do safely to keep your shoulder moving. If you’re experiencing pain or loss of motion in your shoulder, give us a call on 02 9922 6806 or email us and we’ll talk to you about how we can help. Further reading on shoulder pathology : https://www.back-in-business-physiotherapy.com/we-treat/shoulder-problems.html References 1. Mayo Clinic. 2020. Frozen shoulder [Onlinehttps://www.mayoclinic.org/diseases-conditions/frozen-shoulder/symptoms-causes/syc-203726842. Healthline. 2016. Frozen Shoulder [Onlinehttps://www.healthline.com/health/frozen-shoulder Uploaded : 23/07/2021 Read More -

Foods for muscle recovery
Foods for muscle recovery Do you workout a lot and are looking to maximise the effects of your exercise regime by eating the best food afterwards? If you look this up online, you’ll be hit with a million and one pages to read through, with many of them saying different things. It’s a bit of a minefield and can be con-fusing to the average Joe. Fear not, because here at Back in Business Physiotherapy we have great information at our fingertips and want to share it with you. We’ll keep this simple… No fancy scientific words here to confuse the brain. There are a few foodstuffs that are particular-ly important when it comes to improving your muscle recovery following a workout. The key play-ers here are protein, carbohydrates and water. Protein Protein is the building block of every cell in our body (it’s pretty important!). During a workout, the proteins that make up muscle cells break down. After theyhave broken down, the body goes through a recovery process whereby these muscle proteins are repaired, and some new cells are built. This is how our muscles get bigger. Eating a healthy source of protein after a workout can give the muscles the building blocks they need to recover and get stronger. Good sources of protein include eggs, chicken, fish, Greek or other high-protein yoghurts, and cottage cheese. Some people also opt for protein powders and bars to help them reach their pro-tein requirements. Carbohydrates Carbohydrates (aka ‘carbs’) are the body’s main energy source. The movement we do during a workout uses energy. Our muscles store energy so that when we need it to smash out a solid weights session (or any exercise of your choice), we have it there ready to go. After a workout the stores of energy are depleted, and we need to replenish them to ensure we have more in the bank for the next thing we want to do. Good sources of carbohydrate include dark green leafy vegetables (such as kale and spinach), sweet potatoes, fruit, rice, quinoa, and pasta. Water Our bodies are made up of approximately 70% water. It is literally everywhere in the body. For all the crazy chemical process that occur in the body every second, we need water to allow it to happen. During and after exercise, the body loses water through sweating. It is vital to drink plen-ty of water after exercising (as well as before and during… Just drink it all the time, pretty please) to make sure we stay hydrated and to maximise the recovery process. Better still, good sources of water are easy to find! We recommend starting with the tap in your kitchen! 😜 A helpful tip Evidence suggests that eating a post-workout meal combining a 3:1 ratio of carbs to protein will maximise your recovery. Try brown rice with grilled salmon and kale for a powerful, nutritious meal. And drink water before, during and after exercise. We also think you should give us a call to book an appointment, so we can have a more detailed chin-wag about this if you so desire. Call us on 02 9922 6806 today! Link to in-depth analysis on Sports Nutrition - https://www.back-in-business-physiotherapy.com/we-do/nutritional-supplementation.html References 1. Healthline. 2016. Post-workout nutrition: What to eat after a workout. [Onlinehttps://www.healthline.com/nutrition/eat-after-workout. [Accessed 04 June 2020]2. Webster-Gandy, J. et al. 2012. Oxford Handbook of Nutrition and Dietetics. 2nd ed. Oxford: Oxford University Press Uploaded : 29 June 2021 Read More -

Shoulder Impingement
Injury blog: Shoulder impingement Do you have shoulder pain? Are you an office worker, professional athlete, hairdresser or full-time parent? These are just some of the types of people we see in the clinic who need help with shoulder pain. One of the most common complaints we treat here, at Back in Business Physio-therapy, is shoulder ‘impingement’ (aka subacromial impingement). “What is impingement?” we hear you ask. Read on to find out. Anatomy overview The shoulder is a pretty complex region of the body when it comes to anatomy and how it all works together to allow us to move. The connections between the arm bone ( humerus), collar bone ( clavicl’), shoulder blade ( scapula) and the rib cage, provide us with the perfect base for a limb that is able to move through an extremely wide range of motion… The most movement out of any other joint in the body. Having lots of movement is great because it means we can do lots of wonderful things like reach the back of our head to wash our hair and reach our backs too (like when tying an apron). In order to achieve this level of movement the shoulder has to be less sta-ble, and this leaves it prone to injury. The arm bone and shoulder blade form the ‘ball and socket’ part of the shoulder, where a large amount of the movement takes place. The ligaments between these bones are quite loose and a group of muscles, known as the ‘rotator cuff’ muscles, help to keep the ‘ball’ of the arm bone posi-tioned correctly over the ‘socket’ of the shoulder blade, as well as aid with certain movements, including rotation or turning of the arm. Small spaces… Over the top of the ball and socket joint sits the ‘acromion’, which is a bony prominence of the shoulder blade which creates a roof over the joint. Between the top of the ball and the bottom of the acromion is a small space known as the ‘subacromial space’. Some tendons of the arm mus-cles that create movement of the shoulder pass through this space on their way to their attach-ment site on the bones. There is also a ‘bursa’, which is a small sac of fluid which helps to keep movements around joints smooth and frictionless. There is quite a lot of tissue all crammed into one small space, and this is an important factor in the development of impingement. Causes Common causes of shoulder impingement include:• Repetitive overarm throwing or other above-shoulder movements• Long-standing poor posture or poor movement patterns• De-conditioned or weak shoulder muscles from leading a sedentary lifestyle• Heavy lifting Anything that leads to the structures which pass through the subacromial space becoming irritat-ed and inflamed can cause impingement-related pain. Inflammation can lead to swelling of the tissues in the small space and when we move our arm up or out to the side, these tissues get pinched between the bones, and we feel pain. Any of the above-mentioned structures can be-come inflamed, but there is rarely just one tissue solely responsible. If the tendon of a rotator cuff muscle is inflamed, there is every chance the bursa will also be inflamed. Signs and symptoms Signs and symptoms of shoulder impingement include:• Pain with arm movements (particularly movement in front and out to the side of the body)• Pain with shoulder rotation• Pain that radiates down the outside of the upper arm• Reduced shoulder range of motion Treatment At the root of most cases of shoulder impingement is poor and inefficient shoulder movement. When you come to see us for treatment, we will look beyond the shoulder to other areas of the body, like the spine. The neck and mid-back areas of the spine are regularly restricted and need some help to move well again. Once the spine moves well, shoulder function improves too. The shoulder blade also needs to sit correctly over the rib cage in order for the ball and socket joint (and other joints) to work efficiently. Weakness of the muscles which stabilise the shoulder blade on the rib cage can lead to poor positioning of the blade during movement, so we will aim to improve this by giving you focused strengthening and stability exercises. A solid base = good, smooth movement. Through a combination of us using our hand techniques (like massage and joint mobilisation), progressive exercises and lifestyle changes, you can expect to see positive changes quite quick-ly. The end goal of ensuring your pain doesn’t return is always a lengthier process and requires dedication from yourself (and us) to make sure the changes we make early on stay in place for time to come. We are here to help you every step of the way. Shoulder pain? Call us today on 02 9922 6806 References 1. Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. Australia: McGraw Hill Education2. Gilroy, A. et al. 2012. Atlas of Anatomy. 2nd ed. Stuttgart: Thieme Links - Rock Climbing and Shoulder Mechanics : https://www.back-in-business-physiotherapy.com/latest-news/305-rock-climbing.html - Shoulder Stabilioty : https://www.back-in-business-physiotherapy.com/joint-stability-sp-161372761.html - Shoulder Problems : https://www.back-in-business-physiotherapy.com/we-treat/shoulder-problems.html Uploaded : 29 June 2021 Updated :7 April 2022 Read More -

Shoulder Labral Tears
Shoulder injury blog: Labral tear The shoulder is one of the most complex joints in the body. It is made up of a total of four joints, numerous ligaments, joint capsules, muscles and other soft tissues. Movement at the shoulder is a complicated process and it relies on the controlled function of all the involved muscles and joints for that movement to be efficient and complete. Our shoulders are the most mobile joints in the body which is great for us because it means as humans we get to partake in fun activities like throwing sports, gymnastics and dancing, as well as movements we generally take for granted like being able to do up our bra’s behind our backs. This wide range of movement is only possible because the shoulder is less stable when compared to other joints in the body, leaving the shoulder prone to injury. This blog specifically focuses on an injury that relates closely to the ball and socket part of the shoulder joint. If you are into throwing sports, you may be familiar with it… It’s called the labral tear. A bit of anatomy…There are two main ball and socket joints in the body, found at the shoulder and the hip. Both work where a rounded ‘ball’ of one bone fits into a hollowed ‘socket’ of another. At the hip (the strongest joint in the body), the socket is very deep, and the ball part fits quite snuggly into it. This is a very stable joint. The socket in the shoulder is very shallow by comparison, and the ball part is still quite large. This is what gives the shoulder its lack of stability. Both the shoulder and the hip sockets are deepened and supported by the presence of a labrum — a rounded soft-type of cartilage. In the shoulder, the labrum completely surrounds the rim of the socket creating a ring. The very top part of this ring also acts as the attachment site for one of the tendons of the biceps muscle — a powerful mover of the shoulder and elbow joints. How does a labrum tear? The main ways labral tears occur are: • Repetitive movements such as overhead throwing• Carrying heavy objects• Dropping and catching heavy objects A tear can occur over time as the tissues degenerate over time and become weaker, or it might be from one single, forceful event. In most cases there is usually a combination of both degeneration and a large force which becomes the ‘straw that breaks the camel’s back type of scenario. As the biceps tendon attaches to the socket through the labrum, any large force that pulls on the biceps tendon (like suddenly catching a heavy object) can lead to the tearing of the labrum itself. The most common type of tear occurs across the top of the labrum from front to back, and these are known as SLAP (i.e. Superior Labrum Anterior Posterior) tears. Signs and symptoms If you have sustained an injury to the labrum in the shoulder, you may notice any or all of the following signs and symptoms: • Pain during shoulder movement (especially overhead and behind back movements)• Restricted shoulder movement• Popping, catching or grinding during shoulder movements• Tenderness at the front of the shoulder Depending on how you were injured, how severe your symptoms are, and your personal circumstances regarding work and home life, you may be sent for some imaging to confirm the tear. The tests we perform in clinic when we assess you do not always give us all the information we need to determine the best plan of action. A combination of clinical tests and imaging may give us a clearer picture of what’s going on. Can it be treated by a physio? Yes, but this completely depends on the severity of the injury and what your goals are. In most cases it is recommended that conservative therapy from a physiotherapist is tried first. Many athletes who have a labral tear can return to playing to some capacity with a non-surgical approach. The treatment aims to return the shoulder to full, pain-free range of motion through hands-on massage, mobilisation and rehab exercises that focus on range, control and strength of the shoulder girdle. For severe tears, you may require the opinion of a shoulder specialist. A labrum is not great at healing itself and sometimes needs help from a surgeon to return to normal. A professional athlete wanting to return to sport may choose this pathway, but a non-athlete who has no desire to throw a ball seriously again may be able to avoid surgery altogether. If you have a diagnosed labral tear, or have recently injured your shoulder and need help, we recommend coming to us at Back in Business Physiotherapy where we can discuss the best course of action for you and your circumstances. References: 1. Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. Australia: McGraw Hill Education2. Ireland, M. and Hatzenbuehler, J. 2018. Superior labrum anterior posterior (SLAP) tears. [Onlinehttps://www.uptodate.com/contents/superior-labrum-anterior-posterior-slap-tears. [Accessed 09 May 2020]. Uploaded : 24 May 2021 Read More -

Mental Health
COVID mental health check-in With the coronavirus outbreak still affecting millions around the world, we thought it would be a good time to check-in and see how you are all going. The news is pretty grim at the moment and you may be finding yourself asking the question, “When will there be any good news?!” This day-to-day bombardment of the effect of the virus across the world is enough to get the happiest of people down. We’re here to make sure you are keeping your mental health in check. We ask you the question… What are you doing to look after your mental health? These have been difficult and stressful times for many of us. Some of us are starting to come out of strict lockdown restrictions, some of us are still feeling the effects, and many of us will feel these effects for some time to come. It’s good to talk If you are struggling on a daily basis and this pandemic has had a real effect on your mental health, you are not alone and help is out there. Being made to stay away from family members and friends is tough and some people, especially the elderly, will have found this extremely difficult at times. Please talk. A phone call or face-to-face video call (technology is great these days!) is a simple way to stay in touch with loved ones. Speak to someone close to you if you are struggling with personal circumstances. Getting a load off your chest is sometimes enough to make you feel relief, even if it doesn’t solve the root cause of the problem. We understand that your problems may run deeper than this and talking to a loved one is simply not enough. The good news is there are lots of great people out there who are trained to work through such things with people. And even if you cannot get a one-to-one session in person where you live, many mental health professionals including life coaches, counsellors and psychologists are running phone or video sessions with their clients. Enter ‘Telehealth’. . Alternatively, chat to your GP or give Beyond Blue a call on 1300 22 4636. Please do not suffer in silence. Simple tips for keeping your mental health in check Want some other ideas to help keep your mental health in check? Check out our list below for some go to’s: • Exercise: It’s simple and well researched. Exercise helps to maintain good mental health. Even in lockdown, find a space in the house or outside in the garden and just move. Squat, lunge, hop, skip, jump, dance… We don’t care what it is, just move regularly (and safely please!).• Eat well: Keep your diet clean and hydrate every day and you’ll be doing your bit to keep the body and mind functioning well. Vegetables and fruit of the green leafy and berry varieties are packed with nutrients that can help keep the brain healthy.• Go to time-out: No, we don’t mean the naughty step, more so a quiet place where you can be with your own thoughts without the distraction of TV, tablets and other types of media. Read a book, take a bath, give the eyes and ears a rest from it all. It may be hard to break your screen habit, but trust us... It’s refreshing!• Get out the colouring pencils: Yes adults, we are talking to you. Colouring is becoming a very popular ‘escape’ for millions of adults around the world. It has been shown to help reduce the effects of anxiety and stress. Get to your local book store or newsagent today, support local shops, and start getting creative (or if you’re unable to do so safely, order online). Our message today is simple. Life is sometimes hard, but there is always action you can take to reduce the impact this has on your mental health. Talk. Move. Relax Uploaded : 24 May 2021 Read More -

Metatarsal Stress Fracture
Who is at risk from a metatarsal stress fracture? Regular, repetitive motions in the foot are the most common causes of metatarsal stress fractures, making runners particularly susceptible. If you have recently taken up running or are trying to run too far too soon, you are at an even greater risk of developing a stress fracture. Other sports, such as basketball, tennis, gymnastics and dance, that put a great deal of repeated pressure on the foot are also common causes. Whatever sport you are taking part in, you should always ensure you have the correct footwear and that it fits properly – as poor footwear increases the chances you will over-stress your metatarsals. Stress fractures can also occur as a result of a different injury entirely! For example, if you sustain damage to an ankle, knee or hip and don’t seek treatment, you may end up overloading your foot on that side to compensate for the pain elsewhere. Osteoporosis, vitamin D deficiency and certain foot problems can also lead to metatarsal stress fractures. What are the symptoms of a metatarsal stress fracture? If you do develop a stress fracture in your metatarsal you will likely experience pain in your foot that will be worse during activity but will lessen when you rest. You might also notice swelling at the top of your foot, and it may be tender to touch. There could also be some bruising or redness around the area. Some people will have balance problems or an uneven gait. What are the treatment options? If left untreated, stress fractures can develop into a complete break or lead to chronic conditions. If you suspect you have a metatarsal stress fracture, you must rest your foot. You can apply ice to ease the pain and elevate your foot to reduce swelling. Avoid tight or heeled shoes. Then make an appointment with us here at Back in Business Physiotherapy We will look at any immediate interventions that will help the healing process, such as wearing a moon boot for a short period to de-load and allow the bone to repair itself. Then we might suggest footwear modifications or advise on your exercise routine changes to prevent the issue worsening or recurring. If the stress fracture was caused by a previous injury, this will need to be addressed as well. If you’re experiencing pain in your foot, or any unexplained pains following a change in your exercise routine, give us a call on 02 9922 6806 or email us so we can check out what’s going on. See link to a clinical example https://www.back-in-business-physiotherapy.com/latest-news/266-stress-fracture-in-an-adolescent-foot.html References 1. OrthoInfo (American Academy of Orthopaedic Surgeons). 2015. Stress Fractures of the Foot and Ankle. [Onlinehttps://orthoinfo.aaos.org/en/diseases--conditions/stress-fractures-of-the-foot-and-ankle/ 2. Physio.co.uk. 2021. Stress Fracture of the Metatarsal. [Onlinehttps://www.physio.co.uk/what-we-treat/musculoskeletal/conditions/foot/stress-fracture-of-the-metatarsal.php Uploaded : 23 April 2021 ; Updated : 29 June 2021 Read More -

Vascular System
What is the vascular system? Your vascular system is made up of the heart and blood vessels, which send vital elements around the body whilst removing waste products. The vascular system consists of the following: ● Heart - pumps blood around the body● Arteries - carry oxygenated blood away from the heart● Veins - carry deoxygenated blood back to the heart● Capillaries - deliver oxygen and nutrients to the organs and tissues around the body, and pass waste back to the circulatory system Why is it important? Without the vital work of your vascular system, you couldn’t survive. Every tissue in your body needs the life-giving blood delivered by your vascular system to do its job - even nerves need a constant supply of blood to maintain function. So, if something goes wrong with your vascular system, things go wrong everywhere. The vascular system carries highly important immune substances such as platlets. There are numerous conditions associated with vascular system dysfunction, including several heart conditions, high blood pressure, vasculitis, varicose veins, blood clots and stroke. How can I look after my vascular system? These are some of the best ways to keep your vascular system happy and healthy: ● Regular cardiovascular exercise helps to keep your heart strong and improve blood flow throughout the body.● A balanced diet that includes fresh fruit and vegetables, lean protein and whole grains, and limits saturated fats, added sugars and sodium will support the health of your heart.● Smoking increases your risk of cardiovascular disease, so quitting is highly advisable.● Managing stress, for example with meditation, breathing exercises or yoga, will reduce the impact on your heart.● Sitting still for long periods of time can restrict blood flow, so make sure you get up and move around at least once an hour. Eating a diet that is high in cholesterol or fatty foods and living a sedentary lifestyle can lead to a build-up of plaque inside the arteries, which reduces the amount of blood that can flow through them! This means that organs and tissues will not receive enough of the nutrients they need, so eating well and getting regular exercise is a must! References 1. Healthline. 2020. What Makes Up Your Circulatory System and How Does It Work? [Onlinehttps://www.healthline.com/health/circulatory-system 2. Health Encyclopedia. 2021. Overview of the Vascular System. [Onlinehttps://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=P08254 Posted : 23 April 2021 Read More -

Physio at home
5 Physiotherapy Treatments You Can Do At Home Want to look after your body like a physio? Whether you’re currently having treatment and want to complement that work, or you just want to keep yourself in the best possible condition, here are five ways that you can proactively take care of yourself from the comfort of your own home. 1. Stretches Stretching a particular muscle or muscle group improves elasticity and allows you to use the muscle more effectively to build strength. Stretches are therefore very important for increasing your control, range of motion and flexibility. If you are exercising, make sure you stretch before and after to reduce your risk of injury and improve your recovery time. 2. Foam rollers If you’ve developed stiff or tight muscles from exercising, using a foam roller can reduce soreness, release tightness or tension and decrease your recovery time. They can also be used to increase your core stability. You will need to hold your body above the roller, then slowly lower the area you want to target onto the roller. You can then roll gently backwards and forwards. It should cause mild discomfort, but don’t push it so far that it causes real pain as this could lead to injury. 3. Hydration Water plays a pretty important role in your body, enabling you to regulate your body temperature, lubricating your joints, assisting your kidneys to remove toxins, and delivering nutrients to cells to give you energy. Drinking enough water is vital, especially before, during and after exercise. 4. Spikey massage balls These small spikey balls can help relieve trigger points, which are hyperirritable nodules (little knots) in muscles that can occur all over the body. They can be caused by injury, over-exercising, poor posture or joint problems. Pressing the ball into the area and making small movements with it helps to release the trigger point, and the spikes stimulate your circulation. Like foam rollers, it’s important not to push too hard on these areas, so take it easy and book an appointment with us if you suspect you need a helping (physio) hand! 5. Clean diet What you eat has a huge impact on the wellbeing and performance of your body. A clean diet, one that avoids processed foods or those high in sugars or additives, is great for taking care of your physical health. For example, proteins support the building of bone, muscle and connective tissue; vitamin-rich fruit and vegetables support cell function; and omega-3 fatty acids help take care of your joints. When was the last time you took a good look at your weekly food intake to ensure you’re giving yourself a balanced meal each day? (Maybe now is the perfect time!) Want a more personalised plan for your physical wellbeing? Give us a call or email us and let’s have a chat about approaches to support your particular needs. Uploaded : 23 March 2021 Read More -

Scoliosis
Scoliosis: what it is and how we treat it Have you ever been told that carrying a heavy backpack on one shoulder or sleeping on one side can warp your spine? This isn’t necessarily the case (although carrying heavy backpacks incorrectly, certainly doesn’t do your back any good). There is, however, a condition called ‘scoliosis’ that can lead to the spine becoming unnaturally curved. It is usually first identified in childhood or adolescence, but can affect people of any age. What is scoliosis? Scoliosis is a condition that causes the spine to curve sideways and to rotate. It can be caused by other conditions, such as cerebral palsy and muscular dystrophy, or by issues elsewhere in the body, but the cause of most cases of scoliosis is unknown. In fact, around 80% of cases have no identifiable cause. There are two main categories of scoliosis: Structural scoliosis is where there is a physical curve to the spine. Functional scoliosis is where the spine appears to be curved, but this is a result of an irregularity elsewhere in the body, such as different leg lengths. Structural scoliosis is permanent, although symptoms can be reduced. Functional scoliosis, on the other hand, can often be resolved. Most cases of scoliosis are mild, and it may take a while to notice it at all. However, the more severe the curve, the more of an impact it will have on your life. Some cases can continue to worsen over time. In severe instances, the amount of space within the chest can be reduced, affecting lung function and restricting the heart’s ability to pump effectively. The curve of the spine can also impact other areas of the body, causing pain or muscle spasms elsewhere. Scoliosis symptoms Mild cases of scoliosis cause little or no pain, but there are other signs that you can look out for. The most common symptoms of scoliosis are: ● Uneven shoulders● Uneven waist● One shoulder blade sticking out more than the other● One hip sitting higher than the other In more severe cases, you may experience: ● Trouble breathing● Back pain● Muscle spasms Cases of scoliosis are often first spotted when a friend or family member notices that the person’s clothes are hanging unevenly, or that their spine appears curved when they see them changing or in swimming clothes. Most scoliosis patients will be identified as children or teenagers - commonly during growth spurts around the time of puberty. However, some cases of scoliosis may go undiagnosed well into adulthood, and some adults will develop degenerative scoliosis as they age. The impact of scoliosis Around 90% of instances of scoliosis are considered mild, and these are often thought to not need treatment as they cause little or no pain. However, even mild curvature of the spine can lead to other issues, such as: ● Difficulty maintaining balance● Uneven gait when walking or running● Loss of alignment in the hips● Reduced range of motion due to lessened flexibility in the spine● Muscle aches or spasms● Loss of stability, increasing the risk of injury or damage to tissues● Low self-esteem if the curve is noticeable or clothes appear uneven Therefore, it’s always worth looking into what treatment options are available if and when scoliosis is first noticed. Treatment for scoliosis In some instances, particularly those of children, it may be necessary to wear a back brace to prevent the curvature from worsening. Physiotherapists will then focus on developing an exercise routine to strengthen your muscles, increase your mobility and develop core stabilisation. Massage and hydrotherapy can also help to reduce pain and discomfort. German physiotherapist, Rudolph Klapp, from 1905, developed a form of 4 point exercise called 'Klappisches Kriechen' , and were first demonstrated at the International Sport Student meeting around the 1936 Olympics. To this day, this form of therapy is still utilized in the German speaking world. Having learnt this technique in 1988-1990 in Switzerland, I devloped a profound appreciation of exercises on the hands and knees, including those found in Hatha Flow Yoga. Additional methods of treatment include myofascial trains mechanical traction muscle energy techniques rock climbing and bouldering In severe cases, surgery may be required, but this is becoming much less common practice due to advances in early detection programs and bracing treatments. Surgery is always a last resort if all other forms of therapy have not proven effective. References 1. Healthline. 2021. Everything You Need To Know About Scoliosis. [Onlinehttps://www.healthline.com/health/scoliosis 2. Spine-Health. 2017. Scoliosis Treatment. [Onlinehttps://www.spine-health.com/conditions/scoliosis/scoliosis-treatment Uploaded : 23 March 2021 Read More -

Overuse Injuries
The most common overuse injuries Overuse injuries occur when a particular part of the body is subjected to repeated demand over a long period of time. Activity that involves using the same motions over and over - particularly if these are ramped up too quickly, performed for extended periods or made using an incorrect or unsafe technique - can cause tissue damage. Below are some of the most common overuse injuries in different types of body tissue. Stress fracture A stress fracture is a small crack in otherwise normal bone that occurs when the bone has been subject to repeated impact. Stress fractures are most common in weight-bearing bones, such as the shin or foot. Often seen in runners, stress fractures can be a result of a sudden change in physical activity or increasing training without enough rest or recovery time in between sessions. To avoid stress fractures, follow a sensible training program that increases your activity gradually and allows plenty of rest time (ask a physiotherapist for advice if you’re unsure). You can also look after the health of your bones by eating a diet high in calcium and Vitamin D. Tendonitis or Tendonosis Tendonitis is irritation or inflammation of a tendon, caused by repetitive actions in that area. Activities like gardening, painting, cleaning, throwing a ball and playing tennis can cause tendonitis. To reduce your risk of tendonitis, try to build up your activity levels gradually rather than doing too much too soon. Take regular breaks and limit the amount of force you use in your actions. Tendonosis is considered more like a degenerative condition. Occurring more commonly in middle age and especially in men, due to higher levels of testosterone, leading to to 'drier' collagen fibres. Rather than inflammation, the tendon may show signs of swelling and necrosis. Blisters Blisters form to protect the skin and can be caused by repeated friction from rubbing or pressure. If you have ever had a pair of shoes that didn’t fit well or were stiff in certain places, you might have experienced a friction blister where they rubbed your foot or ankle. To avoid blisters forming, protect your skin from friction where possible (for example, by wearing socks, or wearing gloves if you are using tools that rub your hands). If you do develop a blister, keep it clean and dry and try to leave it alone as much as possible. Resist the temptation to pop it. Strained muscle Overstretching or tearing a muscle, by overusing it or using poor technique, can result in pain, inflammation and limited movement. Any muscle can be strained in this way, but it is most common in the lower back, neck, shoulder and hamstring. To reduce your risk of straining a muscle, warm up and cool down properly before and after exercise and get professional advice to ensure you’re using the correct technique. Poor posture can also strain your muscles, so consider the way you are sitting and standing, especially for long periods of time. Physiotherapists don’t just help you recover from injury - we also try to prevent you getting them in the first place. If you think you might be at risk from overuse injuries, give us a call on 02 9922 6806. and we’ll discuss whether there are steps you can take to protect your body. Proactive care may seem unnecessary at times, but it is the most pain-free (and affordable) way to manage injuries before they make themselves apparent. References 1. Oxford University Hospitals. 2018. Bone Stress Injuries and Stress Fractures. [Onlinehttps://www.ouh.nhs.uk/patient-guide/leaflets/files/41517Pfractures.pdf 2. WebMD. 2018. Tendinitis. [Onlinehttps://www.webmd.com/fitness-exercise/arthritis-tendinitis 3. Healthline. 2018. Muscle Strains. [Onlinehttps://www.healthline.com/health/strains#_noHeaderPrefixedContent Uploaded : 22 February 2021 Read More -

Carpal Tunnel Syndrome
Relieving Carpal Tunnel Syndrome Pain Carpal tunnel syndrome is a common condition, usually caused by repetitive movements in the wrist. You may associate it most with office workers who do a lot of typing, but there are a number of jobs and activities that can make you more susceptible. So, what exactly is carpal tunnel syndrome, and what can you do about it? What is carpal tunnel syndrome? The carpal tunnel is a narrow passageway in the wrist that allows several tendons and the median nerve to join the palm. Repetitive wrist motions can cause the tendons to become inflamed, or swollen, which puts pressure on the median nerve. The result is pain in the wrist or hand, as well as tingling, burning, itching or numbness in the hand and fingers. If left untreated over time, the median nerve can become severely damaged, leading to lasting numbness or weakness, so if you experience any of these symptoms it’s important to get them checked out. Who is at risk of getting carpal tunnel syndrome? Office workers who are required to do a lot of typing, causing them to regularly flex, extend and rotate their wrists, are at greater risk of getting carpal tunnel syndrome. However, any job that involves repetitive movements of the wrist can cause the same issue to occur. If you use vibrating tools or work on an assembly line where you are repeating movements again and again, you could have an increased chance of getting carpal tunnel syndrome. Similarly, activities that involve any repetitive motions of the wrist, such as racket sports or even knitting, can cause this painful syndrome. The condition is more common in women, and most often occurs between the ages of 45 and 64, although it can strike at any time. Obesity, certain inflammatory conditions (such as rheumatoid arthritis) and fluid retention (common in pregnancy and menopause) also increase your chances. So what treatment options are available? Treatment options Medication may be prescribed by a doctor to reduce the inflammation, and ibuprofen may reduce pain in the short-term. In severe cases, surgery may be required. However, here at Back in Business Physiotherapy we will do whatever we can to help you before the need for surgery arises. We can offer you lifestyle advice on how you might be able to reduce the likelihood of the issue recurring and suggest equipment that could protect your wrist if there are activities that seem to be causing the problem (such as an ergonomic mouse or keyboard). We can also help you with exercises to reduce the pressure on the nerve and strengthen the wrist. If you do end up requiring surgery, we will work with you during your recovery period, helping you to regain strength and motion in your wrist and hand. Side note: Poor posture can also contribute to carpal tunnel syndrome, so a physiotherapist may help you to improve the way you sit or stand for long periods of time (you just sat up straight didn’t you…😉) How can you reduce the impact of carpal tunnel syndrome? There are a few steps you can take to help prevent carpal tunnel syndrome, or to alleviate the symptoms: ● If your job involves repetitive wrist movements, make sure you take regular breaks and alternate tasks if possible, in order to reduce the strain on your wrist.● Use a relaxed grip and a low level of force (for example to hit keys on a keyboard) if possible. ● Keep your keyboard at elbow height or slightly lower and choose a mouse that doesn’t strain your wrist. ● An ice pack can help to reduce inflammation and relieve pain in the short term. There are also certain exercises that you can do to help look after your wrist. Here are a couple of examples. 1. Wrist bendRest your elbow on a table with your arm pointing straight up. Gently bend your wrist forward at a right angle and hold for 5 seconds. Then bend your wrist backward and hold for 5 seconds. Repeat 10 times. 2. Wrist flexHold your arm out straight in front of you, palm down, and bend your wrist down. Use your other hand to press the stretching hand towards your body and hold for 15 - 20 seconds. Then bend the stretching hand in the other direction and use the other hand to pull your fingers back. Hold for 15 - 20 seconds. Repeat 5 times. Depending on your situation and symptoms, a physiotherapist will be able to recommend specific exercises to suit your particular needs. If you’re experiencing symptoms of carpal tunnel syndrome, give us a call on 02 9922 6806 and we will do our best to help relieve your pain and get you feeling stronger as soon as we can. Now that’s something we can hi-5 to! References 1. Medical News Today. 2018. Carpal tunnel syndrome: What you need to know. [Onlinehttps://www.medicalnewstoday.com/articles/184337 2. Mayo Clinic. 2020. Carpal tunnel syndrome. [Onlinehttps://www.mayoclinic.org/diseases-conditions/carpal-tunnel-syndrome/symptoms-causes/syc-20355603 3. Chartered Society of Physiotherapy. 2017. Exercise advice: carpal tunnel syndrome. [Onlinehttps://www.csp.org.uk/public-patient/rehabilitation-exercises/carpal-tunnel-syndrome Uploaded : 21 February 2021 Read More -

Headaches and Physiotherapy
How can physiotherapists help with headaches? You might be surprised to learn that the answer is, quite possibly, yes! It just depends on what type of headache you’re experiencing - and there are a lot more than you might think! What different types of headache are there? There are more than 150 types of headache! What type you’re experiencing depends on the cause, the symptoms, the location and how often they occur. Some of the most common headaches include: ● Tension headache Usually caused by tension in the muscles of the shoulders, neck or face, tension headaches usually give a sensation of pressure all the way around the head, and can cause nausea and light sensitivity. ● Sinus headache These headaches are usually felt as deep, constant pain in your forehead, as well as your cheekbones and/or the bridge of your nose. Caused by sinus infections, they’re usually accompanied by symptoms like a runny nose, blocked ears, swelling in the face, fever and sinus pain. ● Dehydration When you become dehydrated, the brain temporarily contracts because of the lack of fluid, causing it to pull away from the skull. Which hurts. The pain can usually be felt all over the head and can be anything from a dull ache to an intense throbbing. So, keep up your water intake. ● Cervicogenic headaches These are caused by pain referred from tissues in the neck. They usually cause pain on one side of the head, from the base of the skull to the temple of the eye, and are aggravated by neck movements. ● Migraine If you’ve ever had a migraine, you’ll know it’s way beyond a standard headache. As well as a pounding, throbbing pain in the head, sufferers can experience vision disturbances, sensitivity to light, noise and/or smells, nausea or vomiting, dizziness or stomach pain. Migraines can last for several hours, or even days. ● Cluster headaches Causing intense burning or piercing pain behind or around one eye, cluster headaches can be so overwhelming that sufferers can’t sit still during one. They may cause swelling, redness or tears in the eye affected, and nasal congestion on that side. They’re called cluster headaches because they occur in groups - one to four times per day (lasting 15 minutes to three hours each time) during a cluster period, which can last from two weeks to three months. What can you do to reduce headaches? Depending on the type of headaches you are prone to, there are a few things you can do to try to reduce the frequency and intensity: ● Drink plenty of water● Make sure you’re getting enough quality sleep● Try to reduce your stress levels and make time for relaxation● Don’t skip meals and make sure to eat regular, healthy snacks to maintain your blood sugar levels● Notice if there are particular foods, drinks, smells or environmental factors (such as lighting conditions) that trigger headaches so that you can avoid these in future● If you are sitting at a desk for long periods of time, stretch your neck, shoulder and back muscles regularly● Warm up and cool down properly after exercise How can a physiotherapist help? The two main headaches that physiotherapists can help you with are tension headaches and cervicogenic headaches. In the case of tension headaches, a physio will relax and unlock the muscles, releasing the tension that is causing the pain. They will also look at lifestyle factors that might be contributing to the problem, such as stress, and help you to manage these. For cervicogenic headaches, the goal will be to address the neck issue at the root of the problem. This could involve manipulation, massage or mobilisation. They will likely teach you exercises to perform regularly, which will help to relieve the problem. Poor posture is a common cause of cervicogenic headaches, so your physio will also look at your posture and ask about your living/working space to address that problem. References 1. WebMD. 2020. Headache Basics. [Onlinehttps://www.webmd.com/migraines-headaches/migraines-headaches-basics2. Headache Australia. 2020. Headache types. [Onlinehttps://headacheaustralia.org.au/types-of-headaches/. [Accessed 19 Dec 2020] Uploaded 28 January 2021 Read More -

What is a Physiotherapist and what do they do and treat?
Physiotherapy FAQ: answers to some of your most common questions We get asked a lot of questions about our work, and we know there are a few misconceptions and misunderstandings about physiotherapy out there. So, we wanted to answer some of the most common questions and set a few things straight! What is physiotherapy? Physiotherapy is treatment to restore or maintain mobility, function or wellbeing. Physiotherapists can help you recover from or manage an illness, injury or disability, and help you to prevent injury. We also help you to maintain general fitness and use physical approaches to support your overall wellbeing. What conditions does a physiotherapist treat? The most common reasons to see a physiotherapist are injuries, disability, pain, or other issues affecting your physical mobility. However, a wide variety of problems can have causes within the body that a physiotherapist can help with. Some conditions that physios treat, that you may not be aware of include: ● Headaches caused by muscle tension or neck problems● Dizziness caused by issues with the body’s balance system● Bladder or bowel incontinence caused by weak pelvic floor muscles● Coughing or breathlessness caused by certain respiratory disorders● Pregnancy and postpartum recovery to safely increase activity levels and strengthen weakened muscles● Weight management to identify potential barriers that are preventing weight loss● Symptoms of certain chronic diseases, such as hypertension, emphysema, diabetes, Parkinson’s, ALS and arthritis, can be mitigated or managed through physiotherapy Do you need qualifications to be a physiotherapist? Yes! You need a degree and thorough training. Ongoing learning and regular upskilling is also required to maintain registration with our professional body. What does physiotherapy involve? Physiotherapists use a wide range of techniques and tools to help you with your issue. These include and are not limited to the following: 1. Hands-on techniques These are the physiotherapy techniques you’re probably most aware of and involve directly helping to restore movement to the affected area. Examples of hands-on techniques we frequently use are: ● Joint mobilisation● Joint manipulation● Massage● Soft tissue techniques 2. Exercise Physiotherapists will often work with you on exercises to strengthen your muscles, increase your range of movement and improve function. These exercises may be performed during your session, and you will most likely need to continue them at home between appointments. 3. Taping Physiotherapists may tape or strap areas to relieve pain, enhance stability or prevent further injury or damage. 4. Additional therapies Many physiotherapists are trained in additional therapies that can relieve pain, improve movement and promote healing, such as: ● Acupuncture● Hydrotherapy ● Ultrasound - using high-frequency sound waves to stimulate blood circulation and cell activity● Transcutaneous electrical nerve stimulation (TENS) - an electric current delivered to a specific area to relieve pain 5. Education and advice Physiotherapists look at the body as a whole, not just the particular issue at hand. That’s because your body works as a whole, not in separate parts, and different areas can impact one another. Therefore, we’ll look at your overall wellbeing and see what issues might be connected. We’ll also look at lifestyle factors that might be contributing to your problems, and advise you on how you can make changes to prevent further issues. We can also provide advice on avoiding injuries in the future as well as general wellbeing information. Will I need to get undressed for my appointment? We will most likely need to look at the area causing the trouble, so you may need to reveal that part of your body. Where that is will depend on how much clothing you need to remove. We recommend wearing comfortable, loose-fitting clothing to allow us to treat with ease, and to allow you to be able to do any exercises or movements that are necessary for a successful treatment session. Should I see a physiotherapist or a doctor? If you are in pain or struggling with a particular condition, you might not be sure who to see. Physiotherapy will often work alongside medical treatment, and we will refer you to a doctor if we think they are better placed to help you or that you would benefit from seeing a doctor as well. If in doubt, just give us a call and ask! Uploaded : 28 January 2021 Read More -

Reflections of a career in musculoskeletal physiotherapy
Reflections over 35 years on the development and set backs in musculoskeletal physiotherapy by Martin Krause (December 2020) Having graduated from Cumberland College Health Science, Sydney, Australia in 1986, I was fortunate. We had a burgeoning profession in the art and craft as well as the embryonic science of Musculoskeletal Physiotherapy. At my time of graduation there wasn't a single Physiotherapy PhD at the College. The college wasn't yet affiliated with Sydney University. However, it turned out, that what we were learning in Australasia, was at the forefront of physiotherapy worldwide. These included Wet cadaver labs for training in anatomy. Post graduate Manipulative Physiotherapists teaching us, under graduates, Manual Therapy. Based on Post Graduate Biomechanics qualifications, Jenny McConnell and Robyn Grote were commencing their careers, with new concepts such as patella taping, tendon proprioception, and motor control. Janet Carr and Roberta Shepard were describing the conundrums of movement control, Bernsteins degrees of freedom and Kugler and Turveys oscillatory control systems, We still learnt PNF (Proprioceptive Neuromuscular Facilitation), massage and movement analysis. World acclaimed professors, the late John Sutton and Greg Gass were teaching us work physiology. Neurophysiology was taught with an over-whelming emphasis on pain and motor control. We were some of the first graduates in a new form of teaching which involved continuous learning, project based and experiential assessment and competency criteria. Clinical reasoning was used for the first time, which meant placing value on clinical signs and symptoms, rather than a diagnostic medical lead referral system, thus leading to Australasian physiotherapists being some of the first primary practitioners in the world. Researchers and clinicains from South Australia (Geoff Maitland, David Butler, Michael Sherlock, Pat Trott), Curtin University (Bob Elvey, Brian Edwards, Lance Twomey, Max Zusman), University of Queensland (Julie Hides and Gwen Jull) were changing the world in terms of our understanding of Manual Therapy The journey This is one of the first website on physiotherapy to ever exist. Originally published in 1998, it came about after a culmination of a decade of teaching and presenting workshops around the world. These were often countries who had little to no access to Australian Manual Therapy. Although I no longer teach, I continue to regularly update this website, hoping to make an impact on my profession and all the people my profession treat. My philosophy in teaching was to 'train the trainers'. Although each update has only a hand full of readers, I had the experience, whilst cycling across Argentina, that one newspaper and radio interview with me, about my interpretation on life, can led to a film, which was presented at the Cannes Film Festival in 1992. From that moment on, I realised even an impact on just one person, may have multiplier affects, beyond our wildest imaginations. In November 1990, four friends set out on a 6 month journey, from Buenos Aires to the Chilean coast at La Serena, Ushuaia to the Bolivian Alti Plano and later the jungles of the Amazon, wetlands of the Pantanal and the Littoral of Uruguay. We were in for a few surprises, including an attempted coup d'etat and hyperinflation. This meant we needed to sleep 'wild' including staying under bridges and making use of abandoned homesteads. Luckily, the truck stops became a haven for food, as the only thing which was affordable were the parrilladas. Drivers would tell people that we were coming, in return for what seemed like bigger and bigger servings of meat, potatoes and salad, they wanted me to tell our story. Of our adventure, where we were from, Australia, and where we were going - to Patagonia!!! We were often accompanied out of town by convoys of excited people. Not only, the people of the truck stops, but journalists wanted our story. These were the days, before the internet, where story telling and the bush telegraph reigned. They were also the years immediately after the 'dirty war' (la guerra sucia), where knowledge was considered dangerous and the memories of the 'disappeared' (desaparecidos) were fresh. The interviews were sometimes quite simple, whereas at times, nothing was off limits, from philosophy to politics. Literature included 'The Kiss of the Spiderwoman' by Manual Puig, Eduardo Galeano (Age of Fire) to Jorge Luis Borges, Gabriel Garcia Marquez (100 Years of Solitude, Love in the Time of Cholera, The Genral in his Labyrinth) to Pablo Neruda and Mario Vargas Llosa (City of Dogs, Aunt Julia and the Script Writer) with the metaphorical images from the deep dark forests of the Chilean Lakes District to the Afro-Caribbean mysticism of Colombia. Politics, included contrasting Peron with, the famous son of Argentina, Che Guevara to the Sendero Luminoso in Peru. One interview, stood out in particular, where all these topics were covered, including metaphors, in the conditional subjunctive vernacular of the Argentine narrative, broadcast on the radio and written up in the newspaper. Two years later, in 1992, in the 500th year since Columbus discovered America, I was sitting in a cinema, in Basel, Switzerland. The movie, El Viaje, was showing. It was about a boy called Martin, who was cycling around South America. The opening scene was in a secondary high school, in Ushuaia, where the teacher says 'sit down Krause'. I, and my friend were stunned!!!! I cannot take the credit for the artistic brilliance of the film. I'm not even sure if I ever met with Fernando Solanas, so I'll never know if I germinated the seed of the ideas portrayed in the film, or whether he just needed a central character to have a name. Critical appraisal of El Viaje On the way to Passo de Aguas Negras and La Serena, Argentina/Chile, 1990 Oscillations - manual therapy and motor control I spent 1986 delving into the conundrum of shoulder stability - the control of a system with almost an infinite number of movement permutations. Here, some of the giants in human movement research were using the oscillatory pendulum and Hooke's mass - spring as an explanation to motor control. An inflection point of stability, weighted by muscular tone and balanced forces allowing for the ranges of movement needed, in the shoulder, for the huge range of activities, we as humans, put our shoulders through. Similarly, I used an anatomical dissection to explain knee stability. Three and half decades later I examined the same principle of oscillatory systems but now with an emphasis on deterministic chaos theory, redundant systems and their interplay based on physiological, neurophysiological and immune 'outliers'. The outlier which dampens, modulates and moves nearby oscillatory systems. Oscillations continued to fascinate and impress. Australian Manual Therapy had been derived from the Grand Masters, James Cyriax (London, UK), James Mennell, Alan Stoddard and Greg Grieve (Norwich, UK). There was a famous meeting in St Thomas's, London, in 1967 where the greats of physiotherapy met and discussed the later creation of IFOMT (International Federation of Manual Therapy) in 1974 (Montreal) and the first meeting in Gran Canara in 1975 . People in attendance included Geoff Maitland, Freddy Kaltenborn, Stanley Paris, and Robin McKenzie. The first home office of IFOMT was by Ian Searle, a New Zealander. Later, other greats such as Bob Elvey (Western Australia) became involved. Although, this appears like a coming together of 'minds', there was a fundamental clash between the biomechanics based sustained stretch of Kaltenborn and their Nordic Technique (OMT), with the oscillatory movements, advocated by Geoff Maitland in Australia. When I arrived in the UK in early 1988 I found a job, at the Norwich & Norwich hospital, where Greg Grieve had been working. Physiotherapists were the main 'port of call' at A&E. I learnt a lot from the physiotherapists as well as guest international speakers. The NHS was a great place to learn and work in a collaborative manner. A responsibility seldom given to physiotherapists at that time. Later that year, whilst in Switzerland, I was fortunate enough to gain invaluable experience at the Medizinisches Zentrum, Bad Ragaz, where I met Geoff Maitland and was able to attend courses with Peter Wells, where spinal manipulations were taught. Maitland examination procedure circa1986 - 1991 The Maitland technique, chased the pain, whereas Kaltenborn chased the biomechanical dysfunction. Both were very precise and both had their merits and limitations. Luckily, in Bad Ragaz I was able to work with OMT trained physiotherapists and learn from them, combined movements, 'locking off and adjusting' spinal joints. Later, in 1991, I had the opportunity to attend a course with David Lamb (Canadian, previously from the UK) where i learnt the OMT method of cervical manipulation. Meanwhile, the Post Graduate program of Manipulative Physiotherapy had been developing in Australian Universities since the early 1980's and was a much sort after qualification, which I completed in 1994. Later, in 1995, I was able to learn mobilisations with movement (MWM) from Brian Mulligan (a New Zealander). He was a very pragmatic and very funny fellow, whose niece I happened to meet, serendipitously, as a client many decades later. All these encounters allowed me to mix and match the best of all worlds and eventually impart that knowledge in the form of Manual Therapy workshops in Chile, Brasil, Japan and Europe. Teaching in La Serena, Chile 1996 Adverse Neural Tension : passive to the active By 1988, I was seriously interested in the nexus between the assumingly 'passive' manual therapy approach and their amazing results (with very little, almost imperceptible loading), and active approaches using motor control and exercises. Bob Elvey and David Butler came onto the scene with Adverse Neural Tension (ANT) whereby mobilisation of nerves improved clinical signs and symptoms. Remarkably, a very 'passive biomechanical' explanation was used. My Masters Treatise, in 1995, was examining the immediate effects of Mechanical Traction on ANT within a very precise dosage range, using a 'descending modulation' neurophysiological argument. In the early 1990's I attended the International Association Study Pain (IASP), in Paris, where the seminal work of French researchers, on the descending modulation of pain, took the emphasis away from the 'pain-gate' Wall and Melzack theory of peripheral - spinal cord modulation and added an extra dimension of descending noradrenergic pathways. This was the first time the pain brain function was being imaged using the new technology of PET and MRI scans. This made a lot of research, in manual therapy, using double blind studies redundant, as it became increasingly obvious that the patient is actively involved in recovery, even when a passive device such as Mechanical Traction is applied. In fact, Geoff Maitland was thought to have said that 70% of the examination process was the 'subjective' examination, with it's inductive and deductive reasoning, 20% the physical examination and the remaining 10% treatment. Luckily, I had close interactions with Bob Elvey, Max Zusman, and later David Butler where ideas and visions could germinate further. Proprioceptive Neuromuscular Facilitation (PNF) and functional movement control by Klein Vogelbach (FBL) Bad Ragaz, also gave me exposure to PNF trained physiotherapists. These were a generation of physiotherapists, on the cusp of retiring, who'd gone to Vallejo, California in the 1970's to learn PNF and become teachers in their field. Simultaneously, another group of physiotherapists, in Bad Ragaz, were involved in teaching FBL, where movement analysis and the ability to describe in words what was being seen 'statically' or 'in action' determined specific choices from a plethora of exercises. Primarily, only known in Switzerland, some of these exercises became world famous in the form of the Swiss Ball. Although PNF techniques were originally designed for neurological patients, these strengthening and mobilising methods were morphed into musculoskeletal injury management, where PNF techniques were often combined with Swiss Ball and FBL techniques to optimise (sporting) outcomes. Teaching in Salvador da Bahia, Brazil 1998 PNF techniques morphed into Muscle Energy Techniques (MET), as learnt from David Lamb. MET, I still use today for the treatment of pelvic, hip and back dysfunction. Concepts of form and force closure and the influence of the thorax were later developed by Canadian Physiotherapists Linda Joy Lee and Diane Lee, both of whom I attended courses with. The latter had worked closely with David Lamb earlier in her career. Research, publications and presentations Stabilometry, EMG and kinematic telemetry in Achilles and ACL surgical post operative rehabilitation Magnesium and Multodextrene supplementation in elite athletes Immune compromise in Swiss Female Elite athletes Dysmenorrhea and stress fractures in Swiss Female Elite athletes Improved range of movement of upper limb tension testing after anteroposterior cervical spine mobilisation Cognitive and physical dimensions in elite orienteering Cycling kinematics, bike fit and EMG activity Publications in the International Journal of Manual Therapy on Mechanical Traction and the Chilean Journal Kinesiolgia on neurophysiological considerations when using clinical reasoning in Manual Therapy Sarcopenia - muscle as an immune organ Presentations from 1993 - 2001 in Switzerland, Germany, Portugal, Spain, Holland, Japan, Zimbabwe, Brazil, Ecuador, Chile and the USA on Clinical Reasoning in Manual Therapy. Including key note speaker addresses at IFOMT of WCPT in Yokohama, Japan, La Serena, Chile and New Master Rome, Italy. Taught functional anatomy and biomechanics on the Diploma of Massage course of TAFE NSW Cycled South America which may have inspired a film? Three TV interviews - -Workstation Ergonomics with Ms Megabyte Morning Show Channel 9, Sydney 2001 - VHS video only - Early Treatment intervention - Prime 7 TV Country NSW 2010 (https://m.youtube.com/watch?v=I_WqKpsTaf8) - Peptides and doping in sport - Sky News, 2014 (https://m.youtube.com/watch?v=0rppkK_j0CA&t=21s) Therapeutic application of Whole Body Vibrations - book co-authored with Alfio Albisini Technology This was one of the first website in world on Physiotherapy. Some of the content from that 1998 website can still be found here. At the time, the URL was www.acay.com.au/~mkrause/welcome.html ,which represented my practice in Wentworth Falls in the Blue Mountains as well as my International Teaching. It was born from a clinical reasoning software (CAI) which I had developed the previous year, during my Post Graduate Health Science Education course. I had undertaken a DOS 5.0 programming course in 1993, whilst using Word Perfect and Harvard Graphics and Lotus 123 during my research at the Rennbahn Klinik, Basel, Switzerland. 40mB hard drive with 5'1/4'' inch 'floppies' and 4mB RAM. That was my first computer and preloved by one of my clients. At the time, word processing required meta-tags, which meant that by 1998, HTML tags and creating a website were almost second nature. I supplemented my knowledge with Java 1.0 and javascript. The Computer Aided Instruction (CAI) was based on website design and Desktop Publishing. The latter was a TAFE course I undertook, during the last year of my Masters in Manipulative Physiotherapy in 1995. Interestingly, in the early years of this website, it was possible to see where the people were, who were reading it. Readers included people on US Battleships and even a person from HR in the US State Department got in touch!!! Teaching, Sports and Travel I left Australia in 1987 to pursue a job in Switzerland. During 1986-1987 I worked in the Illawarra Area Health System, where I met a British Physiotherapist, Bridget, who had worked so closely with James Cyriax, that she was able to apply shoulder injections. She had also worked and travelled with the Royal London Ballet. Fortunately for me, she put me in contact with a Rheumatologist in Basel, Switzerland, who sent my CV to Bad Ragaz, where I was offered a position, starting in April 1988. This left me with 6 months to travel in South America, where I wanted to learn Portuguese and Spanish, with the ultimate aim of working there or in Mozambique or Angola. At the time, Spanish was the only viable option to learn in Australia. I did this, via correspondence, which the NSW Department of Health paid for. I had a friend, Beatriz Oliviera Gomez, who had just graduated from medicine, in Rio de Janeiro, and I figured Spanish would become a conduit to learn Portuguese when I was in Brazil. School French, Spanish, Portuguese, German and later Italian and some Dutch became very useful for working in Switzerland, later teaching, in some of those languages, around the world. When I arrived in Bad Ragaz, I was almost immediately asked to teach. I had no more than 16 months clinical experience. This became a recurring theme, where Rolf Baeni and I would give workshops in South America and in particular Chile, but also Brazil and Argentina in Spanish and Portuguese. These workshops included Jenny McConnell's methods, Clinical Reasoning and the Maitland techniques, Neural Mobilisations, Muscle Energy Techniques, Bad Ragaz Ring Method for Hydrotherapy, conference presentations, etc. This reflected the high standing Australian Physiotherapists had in the world. Bad Ragaz was a place famous in the 'old world' for the thermal springs. Prior to the war, aristocracy would come to spend 3 weeks recuperating and rejuvenating in the springs. Even, in the late 1980's 'the old world' living in the 'new world' would arrive from far flung places such as Tel Aviv, Buenos Aires, Montevideo, Santiago and New York. Bad Ragaz was also famous in the physiotherapy world for the Jim Halliwick hydrotherapy program. He worked with astronauts and cosmonauts on their rehabilitation after extended space missions. Combining the buoyancy and resistance of water for mobility and strength. Bad Ragaz also had a school for physiotherapy workshops and training which had been set up by Dr Zinn. Furthermore, Dr Hohmeister was treating Pope John Paul's knees, as well as other celebrities, including people who would later facilitate us getting contacts in South America, of physiotherapists, who would host our workshops. These were pre-internet days and we needed to 'train the trainers' in order to change the world. A colleague and friend, Pia Baake was a student supervisor in Bad Ragaz, when a young Swiss Italian speaking student named Alfio Albisini turned up. Together we taught him clinical reasoning in the Maitland methodology, as well as neural mobilisations, in Italian and German. He was almost expelled from his school, in Basel, as a heretic, when he described what we had taught him!!!! We were also reprimanded for teaching avant guard methodology to a student from the Nordic School of Manual Therapy.. A few years later, whilst living in Basil, I encouraged Alfio, to pursue the Australian way, where he went to Curtin University in 1995. He met Bob Elvey, Tobby Hall, Kim Robertson and Max Zusman there. Together with Peter Michel, my old boss and colleague whom I'd introduced the McConnell method to, Alfio became a McConnell instructor which he taught all over the world in multiple languages, including some Arabic. He convinced me to come to a conference in Rome, in 2005, where he invited 'the who's who' of musculoskeletal physiotherapy, including all the famous Australian presenters (Gwen Jull, Jenny McConnell, Bill Vincenzino, Michael Shacklock, Tobby Hall) as well as Freddy Kaltenborn and Ron Melzack, The latter was famous for the 'pain-gate theory'. This was a culmination of his teaching of the McConnell technique as well as his interaction with Tobby Hall and Kim Robertson. Later, he was able to teach the Mulligan technique and with Michael Shacklock the ANT methodology. Alfio has taught these courses for a greater part of two and half decades all over the world. The countless physiotherapists whom he taught and who in turn used their knowledge for the betterment of their clients is hard to imagine. He continued to work as a physiotherapist in his own clinic, whilst still teaching. An amazing achievement. I went to Switzerland to compete in Road Cycling and Orienteering. I managed to do that as my prime objective for being in Europe. However, the great people around me, especially Pia Baake, Peter Michel and Rolf Baeni, they seriously encouraged me to be more than just an athlete who happens to be a physiotherapist. I liked the travel with Swiss National Teams, working and training with professional athletes, mixing languages, becoming involved with Reto Wenzil and psychological team building, Olympic development, biomechanics research (Stabilometry, Telemetry, Force Platforms and EMG analysis in Knee and Ankle surgery, as well magnesium and carbohydrate supplementations) at the RennBahn Klinik, Basel, Switzerland and in Magglingen. The Rennbahn Klinik was the conduit to players from AC Milan, Lazio Roma, VFB Stuttgart, Werder Bremen, and FC Basel. We were even made an offer to set up a physio clinic in Milan. These were halcyon days, of a young professional, as well as the climactic ones, where the sky seemed to be the limit. Dr Bernhard Seggesser was the Olympic team doctor and a well known orthopaedic surgeon seeking out perfection. Although a self admitting flawed personality, it was interesting to be working with a genius....and like Bad Ragaz, people would come from all over the world to see us. Underbelly On the darker side, I saw the underbelly of the Sydney Olympics. Coaches, managers and athletes having nervous breakdowns before or after the Olympics.....some people (including a doctor) committing suicide, coaches being committed after being found running around the forest stark naked and seeing 'demons' or to the more mundane psychological depression 'let down' after such a major event. The re-adjustment to normal life and the need to re-define themselves and finding new meaning in life was a terrible thing to see. Working with Tour de France cyclists, National Gymnasts, Olympic Skiers, Rowers, Soccer Players we had seen the impact of anabolic use in the 1980's, yet we turned a 'blind eye' to EPO doping in the 1990's as it was seen as oxygen supplementation where the prevailing attitude was that everyone else is doing it. Later. similar arguments were made with 'recovery' and peptide use. The latter, frequently involved substances which weren't banned but also weren't approved for human use. Sadly, there was a medical doctor, who missed a pre-existing knee injury, in a very expensive soccer transfer. He had a fatal car accident. Whilst teaching in Zimbabwe, the lady who hosted me, agreed to treat two journalists who had been tortured by Robert Mugabe's henchmen. They were so brave and for the first time in my life I actually encountered real fear. The fear that we could all be dragged out of beds in the dead of night, the gnawing tightness in the stomach and the tremor in my hands. On the same trip, a few weeks later, a similar experience, where the night watchman, shot dead an intruder. The intruder and the night watchman happened to be brothers of leaders of two opposing gangs in the local Favela (Brazilian slum). Cover up of where it happened, and to whom followed. to prevent escalation of the situation. After these two closely followed events and witnessing the AIDS ward, with it's smell of death, in Harare General Hospital, I decided to stop teaching. Sport Thanks to my own involvement in high level Cycling, Mountain Running and Orienteering I had the opportunity to cycle with TDF cyclists and thanks to my job, I was taught to ski by Swiss National Ski Team members. Training and interacting with high performance individuals made me understand the process and pitfalls of training from a personal and professional perspective. At one stage I even managed some significant time out, where I cycled a mountain touring bike around 2/3 of South America in 1990-91, so that the altitude and endurance training would change my physiology for life. Demographics What is surprising is how demographics can influence your specialisation. Whilst teaching in Japan, I noted that a lot of people have 'frozen shoulders', whereas in Switzerland I didn't see a single 'frozen shoulder' but it seemed like everyone had Scheuermans Disease. Whilst working in the Blue Mountains, people were generally Blue Collar workers and out door types, pulling sleds to the South Pole or climbing Mt Everest, whereas in the early days in North Sydney, the predominant white collar IT workers had very little muscular physique. Sports specific injuries and physiques are also an interesting variation, where I seemed to generally see people from 'individualistic' type of sports, with the exception of soccer. Interestingly, when working with elite and professional athletes, I'd often come across people who were in the latter part of their career and who had never really been injured enough to see a physiotherapist. This was the case with a tennis player, who at the time was playing doubles with Boris Becker. he was in his late 20's and came to see me with some hip pain. He was such a natural talent, that his abilities were serendipitously discovered, whilst playing ice hockey, with a friend, at 13 years of age. He managed to be ranked 14th in the world rankings and never have an injury! We often aspire to be an elite athlete and we look at them for perfection, yet in the science of physiotherapy, we are frequently trying to establish a norm. What is it that these 'outliers' can tell us, for the treatment of the general population? Many programs have now been set up, for injury prevention. An example includes FIFA 11 Plus in soccer as well as the modification of sport such as the reduction of ball heading to prevent concussion like injuries. Since, deterministic chaos uses 'outliers' as does game theory, I formed an interest in these areas. Health advocacy Even whilst still at school, I lobbied for cycling infrastructure and recognition as an equal road user. Back in the 1970's, where the car was king, we cyclists were a fringe community, who generally knew someone, or knew of someone, killed on the road whilst cycling. As such, I cycled all over the world and saw how things were done elsewhere, I was also a part of the fledgling mountain biking and pack cycling scene. Additionally, road cycling gave me the opportunity, to work and ride with Tour de France cyclists as well as Swiss National Team track and road cyclists. Whilst visiting Montreal for a Biomechanics conference, I discovered the Route Verte of Quebec, with my life long friend and famous Belgium physiotherapist, Jean Louis Thonnard (Catholic University of Louvain, Belgium). This was 1998 and I was living in the Blue Mountains, west of Sydney. We had one of the busiest highways, in Australia, crossing the Blue Mountains, which was getting an upgrade and it followed the railway line. Next to the railway line and through various National Park tracks, there was the opportunity to develop a Trans Blue Mountains Cycling Trail. I created a small group of advocates where we defined our submissions to government, based on the health and economic value of cycling to the community. One quarter of a century on, we're still fighting and gradually getting results. Read more : the Sea to Sky Cycling Trail. Muscles and the immune system Having worked at the highest level of sporting endeavours I noticed the link between muscles and the immune system. Moreover, an older person asked me "why are my muscles falling off me?" When I didn't know the answer, as I'd always done in life, I went looking for the answer. The answer was Sarcopenia. In 2002, I had never considered the muscle anything more than a prime mover, but suddenly it was a protein sink for hormones and immune substances. The most important organ of the immune system! The nexus was now complete, muscle-immune-neurophysiology, pain and inflammation. I'd examined hormones and exercise in regards to the thyroid gland, pro-opiomelanocortin, and the locus coereleus back in the day in Bad Ragaz in the late 1980's. One of the first courses I'd ever attended, was on myofascial releases, with Francine St George, where I felt a serious immune reaction to such techniques. Years later I learnt about Myofascial Trains and in 1998 I started Dry Needling. Later, in the mid 2000's, Jay Shah, demonstrated fibroblastic movement activity during dry needling and the release of immune substances!! Anecdotal clinical observations were followed by the scientific evidence, not the other way around! Paradigm shifts The paradigm on graduation in 1986 was that physiotherapists don't massage, we do joint mobilisations and use electrotherapy modalities. In 1987 I learnt the power of massage from Francine St George and her myofascial release techniques. Trigger point massage followed. Australian Physiotherapists weren't particularly good at exercise prescription, whose void was filled by the introduction of Exercise and Sports Science courses around that time. However, the manual therapy approach was being blended with concepts of motor control by Jenny McConnell. The passive treatment approach paradigm was further confronted when i reached Switzerland, where German speaking physiotherapists had a Krankengymnastic (Remedial Gymnastics) background, where exercise was used for all forms of musculoskeletal dysfunction. As the Iron Curtin fell, the East German physiotherapists, who were frequently graduates of the Sports Science Academy of Moscow added to the strong exercise treatment philosophy. They wanted to learn from me, whilst I was learning from them, functional stabilisation and mobilisation was being used, which for all intents and purposes was core stability. A concept, later made famous by Queensland University researchers (Paul Hodges and Gwen Jull) in the mid 1990's. Classification of low back pain, based on movement disorder, was further developed, by Peter O'Sullivan at Curtin University, in the late 1990's. I was teaching in Japan, in the mid 1990's, where I saw Kinesiotape for the first time being used. Later, whilst teaching in Portugal, I met physiotherapists researching the effect of Kinesiotape. In many countries, whilst teaching, I learnt that many physiotherapists had never used a tendon hammer, yet we could all learn from one another, different approaches to similar problems. In the 1980's, the concept of University training, in many European countries, was embryonic, let alone the use of clinical reasoning, where medical practitioners dictated diagnosis and treatment prescription. In Switzerland, some friends and colleagues undertook Osteopathy training to make up for this lack of autonomy and lack of University education. Some Chilean colleagues became chiropractors. By the early 2000's, muscles became an organ of the immune system, which could be stimulated through exercise, myofascial releases and trigger point dry needling. The imaging of pain which had begun in the early 1990's was being taken to the ultimate level by Lorrimer Mosely and his treatment of Sudek's Atrophy (CRPS). In the 2010's, functional cortical stimulation was being used for the treatment of chronic knee pain by my friend and ex-student Abrahao Baptista in Brasil. By 2020, those oscillatory systems of joint mobilisation and motor control from the 1980's were being taken, by me, to the level of 'deterministic chaos' where the 'outlier' defines the health of the system. An incredible journey from the passive joint oscillations to the immune system and eventual 'deterministic chaos theory' in 2020. The best profession ever!!!...at least for me it has been such....and added to these major developments, in thought and knowledge, have been all the positive experiences, I've had with teachers, colleagues and clients, whom I've taught and treated along the way. Uploaded : 29 December 2020 Updated : 31 August 2022 Read More -

What’s new in 2021?
What’s new in 2021? Three activities for you to try. Good riddance 2020, hello 2021! As we say a grateful goodbye to what we can probably all agree has been the worst year in a long time, we’re starting a brand-new year filled with hope and possibility. 2021 brings fresh starts and fresh opportunities for all, making this a perfect time to try something new! Here are three suggestions for activities to unlock your potential in 2021. Paddle boarding This has become a real craze in recent years, and if you’ve ever given it a go you probably understand why. Getting out on the water is great for your mental wellbeing, promoting a sense of relaxation and calm. It can be done on almost any kind of water, so you don’t have to live close to the ocean to get involved. Pros: Paddle boarding is a workout for your whole body, but is particularly good for your core strength, arms and abs. It’s a low-impact workout, so won’t put strain on your joints. As if that wasn’t enough, it even improves your cardiovascular health, reducing the risk of a stroke or heart attack. Cons: Paddle boards are pretty big - usually around 10 feet long - so they can be pretty hard to store and transport. Inflatable paddle boards solve that problem, but they can bounce on rough water and take more energy to push. Plus, you have to pump them up. Reminder to wear plenty of sunscreen and drink lots of water while you’re out on the board to avoid sunburn or dehydration. Alternative: Don’t fancy standing up on the water? Kayaking has many of the same benefits, and you get to sit down while you’re doing it! Win-win! Dance fitness Dance is a great way to exercise without even realising you’re doing a workout - you’ll be having too much fun. There are so many different types of dance class designed to give you a workout, so whether you prefer something upbeat like Zumba or salsa that will increase your aerobic fitness and work your muscles, or something more controlled like ballet that builds your core strength and tones your whole body, you’ll find something to suit you. Pros: Dancing is a workout for the whole body, and a great way to meet new people. It improves your coordination, flexibility and balance, and it even gives your brain a workout as learning and remembering the steps is good for your cognitive function. Cons: Certain types of dance, such as ballet, can be tough on your joints, particularly your knees. Make sure you have the appropriate footwear for the style of dance you’re doing and you’ll be off to a flying start! The repetitive movements can also cause strains, so make sure you warm up before class and cool down properly afterwards. Alternative: If dance isn’t your thing, trampolining has a very similar impact on your body and is also loads of fun! Climbing Climbing can take a variety of forms, whether you prefer an indoor bouldering wall or a countryside rock face. Bouldering is easily accessible for beginners, and there is plenty of scope for you to expand your activities as your skill increases. Climbing works your whole body and vastly improves your strength. Pros: Climbing particularly strengthens your hands, forearms, biceps, back and shoulders. Your upper body strength will improve before you know it. You’ll also find your abs, glutes, thighs and calves get a pretty good workout too. There is a great community around the activity, so you’re likely to make new friends when you get involved. Cons: Not one for anyone with a fear of heights! It also takes a long time to build up the upper body strength required to get really good, so be prepared to be a beginner for a while. Climbing can also be tough on your joints and tendons, and can lead to arthritis in the hands for regular climbers. You also run the risk of falls, bumps and scrapes, and the tougher climbs you do, the more dangerous the activity becomes. See also : https://www.back-in-business-physiotherapy.com/latest-news/305-rock-climbing.html for further information on exercises for rock climbing. Alternative: If you want to keep a bit closer to the ground, gymnastics, circus or pole classes also improve your strength and helps build your muscles. Uploaded : 11 December 2020 Read More -

Tennis elbow vs golfer’s elbow - what’s the difference?
Tennis elbow vs golfer’s elbow - what’s the difference? Tennis elbow and golfer’s elbow. Two causes of elbow pain that are associated with sports, even though you don’t ever need to play either sport to experience one of these conditions. Both involve inflammation of the tendons that attach to the elbow, and are caused by repetitive motion of the arms and wrist. But what are the differences between them, and how can you tell which, if either, you have? Below we have shared the main attributes, symptoms, causes and treatments for each elbow condition, as well as what you can do to help prevent both. What is tennis elbow and golfer’s elbow? The most noticeable difference between the two conditions is the area of the elbow that they affect. Tennis elbow causes pain in the outside of the elbow and forearm. This is due to strain to the extensor carpi radialis brevis and extensor digitorum tendons of the forearm, which extend and stabilise the wrist. Golfer’s elbow on the other hand, will cause pain on the inside of the elbow and forearm as the inside tendons of the forearm (which flex your wrist and contract your fingers when you grip something) have been overused. Tennis elbow is most common in people aged 30-50, whereas golfer’s elbow predominantly affects people over the age of 40. Symptoms Both conditions will cause pain in your elbow that usually radiates down your forearm. In tennis elbow, this pain will begin on the outside of your elbow, whereas in golfer’s elbow you will feel the pain on the inside of your elbow and arm. There are a few other signs and symptoms which are common in each condition: ● Pain when you reach for, grasp or lift something● Weakness in your forearm or a weak grip● A dull ache when resting Causes Both elbow conditions are caused by repetitive movements which overuse certain muscles and tendons. ‘Overuse’ is considered to be high-level activity of 30 minutes or more, performed three or more times per week. However, the movements that cause each condition are different. Tennis elbow can be caused by impact motions, such as hitting a ball with a tennis racket (or badminton racket or baseball bat) and throwing motions (javelin and discus throwers are prone to the condition). Repetitive lifting or turning of the wrist can also lead to tennis elbow, making plumbers, painters, builders and hairdressers particularly susceptible. Regular typing can have the same effect. Golfer’s elbow is predominantly brought on by repeated lifting movements, especially where the elbow is extended and the palm is face down. Gardening, digging, assembly line work and throwing a ball are common causes, and if you are lifting weights with a poor technique then you are more at risk of this condition. The shoulder, neck and ribcage can also contribute to tennis and golfers elbow like symptoms. Neural irritation may require joint mobilisations to the cervical and thoracic spines, as well as a home programme of neural mobilisation exercises. Additionally, altered bone alignment in the elbow and wrist can create dysfunctional biomechanics leading to tennis and golfers elbow symptoms. Mulligans Movement With Mobilisations (MWM) can help eleviate symptoms. Treatments The good news is that both tennis elbow and golfer’s elbow are very treatable. There are a few things that you can do at home to reduce the pain: ● Rest your arm● Apply ice to reduce the inflammation● Take anti-inflammatory painkillers, such as ibuprofen (always check with your doctor first) However, both conditions can take weeks or even months to recover from, and can worsen if not treated effectively. Your best course of action is to see a physiotherapist, who can help you with exercises to stretch and strengthen the forearm muscles and reduce strain on the inflamed tendons. Your physio will also advise you of how you can adjust your arm movements in future to avoid this happening again. Prevention Although we’re more than happy to help you with your elbow pain, we’d ideally like you not to experience it in the first place. Here are a few steps you can take to prevent tennis and golfer’s elbow: ● Regular stretching and strengthening exercises for the muscles of your forearm● If your job involves the kinds of movements discussed above, talk to your manager about safety precautions that can be put in place● Take regular breaks from any repetitive arm motions and stretch your muscles● If you are performing regular sports activities, make sure your technique is correct and seek professional coaching or advice to improve your movements and check that your equipment is appropriate for your needs If you are experiencing pain in your elbow, do not leave it until further damage has occurred. Get in touch with us straight away by calling 02 9922 6806 and we can start your road to recovery. References 1. Orthopedic Institute of Pennsylvania. 2020. Tennis Elbow vs Golfer’s Elbow Explained. [Onlinehttps://www.oip.com/tennis-elbow-vs-golfers-elbow-explained/#:~:text=Tennis%20elbow%20presents%20with%20pain,or%20tingling%20in%20your%20fingers. [Accessed 25 11 2020] 2. NY Orthopedics. 2015. Tennis Elbow vs Golfer’s Elbow. [Onlinehttps://www.newyorkorthopedics.com/2015/08/21/tennis-elbow-and-golfers-elbow-the-causes-symptoms-treatments/. [Accessed 25 11 2020] Uploaded : 11 December 2020 Read More -

Preventing injury with physio and yoga
Preventing injury with physio and yoga Are you in a constant battle with your body to stay injury and pain-free? Maybe you’re having the same conversation with yourself over and over about how you need to be kinder to yourself, eat cleaner, and get stronger and more flexible? When you don’t have the right ingredients making up your life, this can be a difficult task to undertake. Luckily, there is an answer. Many people will visit a physiotherapist after they injure themselves. A common occurrence is to then part with the physio sessions once the pain has gone away and the person is back to their normal lifestyle. On many occasions, we see these people back in the clinic again within 3-6 months, often with the same problem rearing its ugly head. This is because pain-relief and return to function is only the beginning of the recovery and rehab phase. To avoid these repeat visits to us for the same issue time and time again, rehab should be seen through (and continued) until you are back to baseline PLUS giving yourself some “extra in the tank.” Making a real change to the body in the way you move, how frequently you move, and how strong you are takes a long time. Many injuries are years in the making and cannot be reversed in a few treatment sessions alone. So, how about having your knowledgeable physio see you through to that 110% mark so next time you take to the field, not only will you not be afraid of injuring yourself again, but you’ll be able to put more into your performance (on and off the field) than you did before. Visiting your physio on a regular basis, regardless of whether you are injured or not, is a great way to PREVENT injury, as you’ll have a movement and health expert with you at every step of the journey. There are many benefits of seeing a physio regularly for injury prevention. These include: • Having a qualified health practitioner who is able to seek out movement problems before they present to you as pain and disability• Having your very own sounding board for any frustrations you may have with your body• Knowing you have the best person to treat and provide lifestyle advice based on the most up-to-date evidence-based research• Having an expert practitioner who is able to assess, implement a short and long-term plan, and then re-assess along the way where required to ensure you are reaching your goals We understand regular treatments can be costly,but staying healthy and injury free is a much better option then constantly being plagued with injury, or possibly ending up with a life-changing, chronic condition that requires ongoing medical costs. Put it this way, why not use your private health cover to prevent injury, rather than to treat it once it arises and impacts your life? What else can I do? There are many healthy options out there that can supplement the good work you do with your physio. Not everyone is game for following strict exercise regimes set by their practitioner. A different outlet may be required, and we are trained to recognise these patients and are always supportive of any choice a patient makes if it is going to benefit their mind and body. A very popular exercise choice is yoga. Yoga has been practiced by millions of people for thousands of years (3000+ years to be more accurate!) and provides a whole body, or holistic approach to health. That is, it’s good for the mind, body and spirit. The beauty of yoga in modern times is that it is widely accessible, has different forms for different tastes, and can be enjoyed by all regardless of age. Some of the proven benefits of yoga include: • Improved flexibility and body-wide strength• Improved heart and lung health• Improved sleep cycles• Effective weight management• Effective control of stress, anxiety and depressive disorders• Effective pain management (including chronic pain states)• Enhanced overall quality of life The list goes on. We think all of these qualities perfectly complement what we are trying to achieve in our treatment plan for you. Considering trying yoga after reading this? Speak to us next time you are in the clinic, and we’ll be able to recommend a local yoga studio to try. Bonus yoga benefit… It’s a social affair, so take a friend or family member with you and you can both reap the benefits, and enjoy a coffee after class! (And ahem… please pass on our details to them too) 😉 References 1. Physiopedia. 2020. Physical activity and injury prevention in adolescents. [Onlinehttps://www.physio-pedia.com/Physical_Activity_and_Injury_Prevention_in_Adolescents. [Accessed 05 Nov 2020] 2. American Academy of Orthopaedic Surgeons. 2020. Yoga injury prevention. [Onlinehttps://orthoinfo.aaos.org/en/staying-healthy/yoga-injury-prevention. [Accessed 05 Nov 2020] 3. Harvard Health Publishing. 2015. Yoga - benefits beyond the mat. [Onlinehttps://www.health.harvard.edu/staying-healthy/yoga-benefits-beyond-the-mat. [Accessed 05 Nov 2020] 4. Woodyard, C. 2011. Exploring the therapeutic effects of yoga and its ability to increase quality of life. International journal of yoga. 4 (2). 49-54. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3193654/ Uploaded : 5 December 2020 Read More -

Healthy Heart
Your guide to a healthy heart We all know how important it is to look after our heart. If you want to live a long and active life, you need to be kind to it every day. But how kind are you to yours? Statistics suggest that many of us need to be doing a whole lot more, as cardiovascular diseases are the number one cause of death globally every year. Nearly 18 million people lose their lives annually as a result of cardiovascular diseases, accounting for approximately 31% of all deaths. Cardiovascular disease is an umbrella term used to describe any disease relating to the heart and blood vessels, including coronary heart disease (CHD) and cerebrovascular disease (e.g. stroke), as well as others. Some of the risk factors for cardiovascular disease are changeable and others are not. These include: Non-changeable factors • Advancing age• Gender – As this affects males more than females• Having a family history of heart disease Changeable factors • High blood pressure• High cholesterol• Being a smoker• Drinking alcohol excessively• Being overweight or obese• Lack of physical activity• High stress levels Your road to a healthy heart So, what can YOU do about it? The good news is, no matter where you are in life, no matter what age, you can do something today to improve your heart health. The following are some of the most important things to consider when working towards having a healthy cardiovascular system. Mizuno et al (2021) Exercise and Sports Science Reviews, 49, 3, 157-167 Keep a healthy weight Being overweight or obese is one of the modifiable risk factors that is easiest to change. You just need to ensure you are doing two things… Exercising regularly and eating a healthy, balanced diet. How many of us know this, but fail to get on board consistently? We’re all a little guilty from time to time, aren’t we? Exercise has many body-wide benefits that are too long to list in this blog but challenging your heart through exercise regularly each week is a great way to help control blood pressure and cholesterol levels. Did you know that going for a 30-60-minute brisk walk each day is all you need to keep the heart in check? There are so many other options when it comes to exercise though… Cycling, swimming, aerobics, team sports, martial arts. As well as helping you maintain a healthy heart, your body will benefit from increased flexibility and strength, and a clearer mind. see also : https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-obesity.html elsewhere on this site Combine regular exercise with a good diet and you will be winning on the weight front if you persist. There are many foods out there that hold ‘cardio protective’ properties. Meaning these foods help you reduce the risk of developing cardiovascular disease if eaten regularly as part of your balanced diet. Some of these foods include: • Those high in Omega-3 fatty acids (including oily fish, walnuts, chia seeds, flaxseed oil)• Red wine (when consumed in moderation)• Dark chocolate and green tea (due to their antioxidant content)• Fruits and vegetables (make these a big part of your diet!) A very strong relationship has been established between the role of perivascular adipose tissue (fat) and exercise on arterial function with obesity (Boateng, SY 2021, Exercise and Sports Science Reviews, 49,, 3, 188-196) meaning exercise induced up-regulation of Nitrous Oxide, Prostaglandin 2, and reduced ROS (reactive oxidative stress) as well as reduced endothelial 1, together result in improved aortic stiffness and endothelial dilation. Other handy tips include: • Replacing salt with herbs and spices during cooking• Reducing intake of foods high in saturated and trans fats which can raise cholesterol levels and lead to clogged arteries. This in turn increases risk of stroke and heart attack. Avoid eating cakes, chips/crisps and pastries excessively. Do not smoke Smoking directly damages your blood vessels which quadruples your risk of heart attack and stroke. Our advice to you is plain and simple… If you do not smoke, keep it that way. If you are a smoker, do whatever you can to begin quitting today. Quitting smoking is tough and needs to be done correctly. Speak to your doctor today for help and advice. The day you smoke your last cigarette immediately decreases your risk of cardiovascular disease and early death. Learn how to manage your stress levels Chronic stress is a major contributor to increased heart rate and blood pressure. Learning to control your stress levels can help to alleviate the effect this has on the cardiovascular system. Physiotherapists can offer advice on ways to manage stress. Some of the most popular forms of stress management include: • Regular exercise• Breathing and relaxation exercises• Meditation (including mindfulness-based cognitive therapy, as well as other forms)• Seeing a doctor, psychologist or life coach Educate yourself and get checked by your doctor regularly as you age The bottom line is your heart health is your responsibility. You must act to ensure cardiovascular disease doesn’t become a part of your life. You have a wealth of resources at your fingertips. We (and other health professionals) are here to help guide you to optimal health. We thoroughly recommend you regularly check-in with your doctor, especially as you advance through to your later years, to make sure everything is functioning well. References 1. World Health Organisation. 2020. Cardiovascular diseases. [Onlinehttps://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1. [Accessed 07 Nov 2020https://www.heartfoundation.org.au/heart-health-education/keeping-your-heart-healthy. [Accessed 05 Nov 2020https://www.healthline.com/health/healthy-heart-tips. [Accessed 05 Nov 2020https://www.heart.org/en/health-topics/heart-attack/understand-your-risks-to-prevent-a-heart-attack. [Accessed 07 Nov 2020https://www.heart.org/en/healthy-living/healthy-lifestyle/how-to-help-prevent-heart-disease-at-any-age. [Accessed 05 Nov 2020] Uploaded : 3 December 2020 Updated : 2 February 2022 Read More -

Diabetes - Type 1 vs Type 2
Diabetes - Type 1 vs Type 2 The 14th November 2020 marked the 29th World Diabetes Day. Since its conception in 1991, World Diabetes Day has been the principal worldwide campaign that raises awareness of the disease diabetes mellitus (DM). This year’s theme focuses on ‘The nurse and diabetes’, and how pivotal a role nurses play in supporting those living with this condition. Do you understand diabetes? Are you familiar with its effects on the human body? If the answer is no, this blog is for you. Facts Here’s a few startling facts about DM… In 2019, nearly 465 million adults had a DM diagnosis worldwide. This figure is predicted to increase to nearly 580 million by the year 2030. In the same year, the disease took the life of 4.2 million people with healthcare costs totaling more than $760 billion. This equates to approximately 10% of the total global spend on all healthcare, which is a huge figure! It also puts into perspective just how big a problem DM is across the planet. What is diabetes mellitus? Diabetes is a chronic, metabolic disease. The word ‘metabolic’ derives from ‘metabolism’, which refers to the body’s ability to breakdown food into energy. With DM, the problem lies with the body’s ability to breakdown sugar (in the form of glucose) into energy for the body to use. When we eat food, the body breaks it down into smaller pieces. Some of these smaller pieces are in the form of glucose, our body’s main energy source. Once in the blood, it travels around the body, being dispensed to all cells, so all of our bodily processes can be carried out and function correctly. The body uses a hormone called insulin to help in the process of converting glucose into energy, ready for use by our cells. Insulin is produced by the pancreas, an organ that is part of our digestive system. In DM, the pancreas either doesn’t produce insulin at all, or it does not produce enough good quality insulin, meaning there is nowhere for the glucose to go but stay in the blood. As a result, the glucose levels rise, which then leads to symptoms of DM. Types of DM There are three main types of diabetes: • Type 1 (DM1): An autoimmune form of the condition, meaning the body’s immune system attacks and destroys the cells of the pancreas that are responsible for producing insulin. People with DM1 must rely on a synthetic form of insulin, usually injected by the person several times a day, in order to control blood sugar at safe levels. Sometimes an insulin pump is fitted which negates the need to inject. • Type 2 (DM2): The most common form of the disease. With DM2, the pancreas either does not produce enough insulin, does not produce effective insulin, or the cells of the body do not react to insulin correctly. In the early stages, this form of the disease can be effectively managed by exercising regularly, eating healthily and making necessary lifestyle changes. Over time, the disease progresses, and people may require medication in the form of tablets, and eventually insulin injections, like with DM1. • Gestational: A form of DM that develops during pregnancy and usually resolves once the baby is born. Women who are overweight, 40+ years of age, and have a family history of DM2 are more at risk of developing this condition. This blog will mainly focus on the differences between DM1 and DM2. We will discuss gestational diabetes in more detail in a future blog. Effects of DM on the body The short and long-term effects of DM1 and DM2 are the same. The short-term effects of DM1 tend to come on quickly and may be fatal if not controlled promptly. Some of the shared and more immediate symptoms of DM1 and DM2 include: • Excessive thirst and hunger• Increased urination• Tiredness and fatigue• Skin infections and slowly healing skin wounds• Visual disturbance, including blurred vision• Mood swings• Headaches• Weight changes (DM1 is usually associated with unexplained weight loss, whereas DM2 is usually associated with progressive weight gain) If DM is not managed well, long-term complications of the disease relate to problems with the cardiovascular, kidney, nerve and visual systems of the body. This leaves a person susceptible to developing: • Heart attacks and/or stroke• Kidney disease• Poor nerve function• Ulcers that affect the limbs• Blindness Poorly managed diabetes is a common cause of limb amputations (due to the resultant poor blood flow and nerve function) and there is a strong association between diabetes and anxiety and/or depression. The key to managing DM in any form is an early diagnosis. The beauty of seeing a physiotherapist regularly is that we are constantly monitoring your conditions and general health. If we suspect there may be an underlying problem that needs medical attention, we will discuss this with you and help direct you to the right person to ensure you receive the correct diagnosis and treatment. Diseases like diabetes are usually diagnosed under supervision of your GP. If you have any questions relating to DM, and how this may affect your ability to exercise, please speak to your practitioner next time you are in. We hope you found this blog informative and interesting. The key to managing disease and injury is to first understand it. If you have any questions, let us know and we’ll be happy to put your mind at ease! References International Diabetes Federation. 2020. World Diabetes Day. [Onlinehttps://worlddiabetesday.org. [Accessed 07 Oct 2020]. World Health Organisation. 2020. Diabetes. [Onlinehttps://www.who.int/health-topics/diabetes#tab=tab_1. [Accessed 07 Oct 2020]. Diabetes Australia. 2020. What is diabetes. [Onlinehttps://www.diabetesaustralia.com.au/about-diabetes/what-is-diabetes/. [Accessed 07 Oct 2020]. Uploaded : 17 November 2020 Read More -

Foam rolling: Pros and cons
Foam rolling: Pros and cons New foam roller and wondering where to start? Have a read of this, and you’ll feel more informed. And if you still aren’t convinced or have more questions, feel free to ask us next time you are in the clinic and we will discuss it with you in person. For now, let’s keep on rollin’. Head into any sports store and there is a good chance they’ll have some foam rollers for sale. Foam rollers are widely available and have been used as a therapy aid by millions of people for years since first coming on the market in the 1980s. What is a foam roller? Foam rollers are usually cylindrical in shape, very lightweight, and range in length and firmness from long to short and soft to hard. Their design and use is simple. You simply lie the roller on the ground, choose a body part, place it on top and start rolling. But what are the actual benefits of foam rolling? Are there any potential side effects? Or negative impacts? Let’s take a look… History Foam rollers were originally used by practitioners that followed the Feldenkrais method of treating the body. Early practitioners used the rollers as a way of providing support to the body and would get their patients to stand on the rollers during balance exercises. Use of rollers progressed over the years. In 1987, their use as a self-massage tool was pioneered by physical therapist, Sean Gallagher. They are now used by millions of people across the globe, including gym goers, weightlifters, gymnasts, athletes and many others, as a tool to massage and release tight muscles. Pros Some of the benefits of foam rolling include: • Reducing muscle pain (including the management of certain pain syndromes like fibromyalgia)• Increasing range of motion around a joint• Making muscles more responsive to stretching• Relaxation• It’s a relatively safe way to self-massage tight muscles Cons Due to their widespread availability, foam rollers can be purchased by anyone, even though they may not be a suitable tool to use for that particular person. There are certain conditions and circumstances where use of a foam roller could be detrimental or damaging to a person’s body. Foam rolling exercises load and stress the underlying tissues, including nerves, skin receptors, blood and lymphatic vessels, as well as bones. People with conditions including advanced diabetes mellitus, lymphedema, varicose veins and severe osteoporosis should avoid this form of exercise, unless advised otherwise by a medical professional. When recovering from a muscle strain, a foam roller may be a handy thing to have around, but rolling over a torn muscle should be avoided in the early stages of injury and until you’ve been given the all-clear by your therapist. Rolling over an acutely torn muscle could hinder the repair of the muscle and at the very least would be incredibly uncomfortable and painful. Please note that scientific evidence supporting the use of foam rolling for therapeutic reasons is sparse and caution should be taken by anyone who uses them. Our advice to you is to ask your trusted physiotherapist if it’s suitable for you. We have the expertise to guide you in the right direction and if it’s a great option for you and your body, we’ll give you the thumbs up to rock’n’ROLL! References 1. Healthline. 2019. What are the benefits of foam rolling? [Onlinehttps://www.healthline.com/health/foam-roller-benefits. [Accessed 06 Oct 2020https://www.health.harvard.edu/staying-healthy/should-you-add-foam-rolling-to-your-workout-routine. [Accessed 06 Oct 2020https://www.researchgate.net/profile/Juergen_Freiwald/publication/308392869_Foam-Rolling_in_sport_and_therapy_-_Potential_benefits_and_risks_Part_1_-_Definitions_anatomy_physiology_and_biomechanics/links/57eb7bee08ae91a0c8d4004b/Foam-Rolling-in-sport-and-therapy-Potential-benefits-and-risks-Part-1-Definitions-anatomy-physiology-and-biomechanics.pdf Uploaded : 17 November 2020 Read More -

Rock Climbing
Climbing and musculoskeletal considerations by Martin Krause Good climbers use a combination of strength, endurance and flexibility. Power is developed by the arms through an upward throwing action of the arms, which instigates efficient eccentric muscle lengthening decelerating forces (rather than concentric - muscle shortening). Additionally, they are able to facilitate kinetic energy across the chain of movement from toes through the legs and pelvis into the trunk and torso. Ideal posture Ideal climbing involves extended arms to hang from thoracic extension, lateral flexion and rotation hip external rotation knee flexion and slight heel rise to develop power through the legs "An inch is a mile" In climbing, 'an inch is a mile' refers to delicate foot and hand placement where body length through the elongation of the thorax with thoracic ring elevation. The shoulder blade needs to elevate and allow the thorax to hang from it. Restrictions of thoracic rotation results in excessive contralateral gluteal contractions. Inadequate shoulder flexion due to limited thoracic ring extension can cause reduced contralateral gluteal activity Gorillas on the Cliff Climbers can develop a 'gorilla-like' posture due to over emphasis on grip arm flexion a '6 pack' Since the abdominal muscles cross the lower 6 ribs, sufficient trunk core stability should not compromise the mobility (especially rotation) of the thorax. Excessive development of the low thoracic - upper lumbar erector spinae can create reduced gluteal muscle strength, reduced diaphragmatic breathing, increased psoas major tightness and reduced core stability. Postural problems associated with climbing could lead to musculoskeletal injury Climbers may develop a gorilla-like appearance due to the unique nature of the sport Gorilla-like appearance alters the centre of gravity of various limb and trunk segments this may lead to shoulder injuries, headaches, neck, arm and back pain Stomach crunches or 'curls' may cause tightness of the rectus abdominis ("6 pack") and external obliques at the expense of weakness of the transverse abdominis muscle increased thoracic kyphosis (rounded back) reduced diaphragmatic lateral expansion which contributes to the gorilla posture resulting in altered thoracic biomechanics which affects active SLR and active PKB suggesting reduced lumbopelvic rhythm (gluteal : hamstring timing) reduced strength in the lumbo-pelvic-hip musculature reduced gliding of the myofascial trains extending from the superficial front line of the latissimus dorsi to the superficial back line of the thoracolumbar fascia and the gluteals Myofascial Trains Arm elevation normally results in contralateral gluteal and transverse abdominal activity in the 'wall plank' position Power = strength, speed and flexibility Training should involve functional movement patterns, whereby some muscles are used as stabilisers whilst others are used as mobilisers. The deeper lying endurance muscles tend to be the stabilisers and are frequently found to cross only one joint or work in an area of limited movement. The mobilising, power muscles, tend to be the 'energy straps' crossing more than one joint and conferring kinetic energy to the movement system. A balance between mobility and stability needs to be attained. Overhead reaching This requires extension and rotation flexibility in the thorax, as well as front of shoulder and chest flexibility. Balanced with this flexibility should be strength in the serratus anterior so that the thoracic rings can 'hang off the arms'. The serratus anterior inter-digitate with the abdominal muscles which cross the lower 6 ribs. So, as the upper rib cage and thoracic rings elevate upwards, an eccentric lower thoracic ring stabilisation must take place to bring the semi squat power of the legs into play. Development of the scapular stabilisers An interplay with the muscular slings, their stabilisers and mobilisers comes into play. The shoulder joint has a shallow socket which provides a surface for the large 'ball' (same size as the hip!) to interface. To maintain stability, the rotator cuff muscles need to provide consistent support and pressure around a centre of rotation. Since these muscles are attached to the scapula (shoulder blade), the shoulder blade requires correct and consistent orientation, otherwise the rotator cuff function is rendered useless (see example below if only the rhomboids [Rh] were used). Read more about stability elsewhere on this site Excessive and prolonged reaching results in tight serratus anterior and pectoral (chest) muscles contributing to excessive strain on the blood vessels, nerves and joints of the shoulder - neck - arm complex (TOS = thoracic outlet syndrome) creates excessive low thoracic erector spinae activity contributing to loss of costal expansion, as well as reduced diaphragmatic rhythm has been associated with impingement in the supraspinatus (superior rotator cuff and subacromial bursa) muscle leading to discomfort in the shoulder with loss of muscle power during activities above shoulder height Acromioclavicular and sternoclavicular (collar bone joints) joints may become inflamed Overhead reaching can result in excessive strain on the back and shoulder blade muscles cause the rhomboids and levator scapulae to become long and weak facilitates the latissimus dorsi to become short and strong scalene muscle tightness, rib elevation and circulations compromise, similar to Thoracic Outlet Syndrome (TOS) Training - the trapezius muscles requires synergistic (complimentary) action by the latissimus dorsi erector spinae (back) oblique and transverse abdominal muscles (not the "6-pack"!!) - the deltoid muscle requires synergistic action by the internal oblique and transverse abdominal muscles contralateral gluteal activation lumbar erector spinae activity - the serratus anterior needs synergy with the external obliques intercostals diaphragm - should replicate the combination of muscle synergies in the most climbing functional way as possible. - arm strength requires gluteal strength Bridging exercises with the Swiss Gym ball and elastic tubing allows functional activity which stretches the pectoral girdle and "6 pack" strengthening of the abdominal, spinal and shoulder blade muscles dynamic stability of the pelvis and hips allowing enhanced freedom of movement on the cliff face "Prone bridging" allows abdominal, pelvic, trunk and arm control to be trained Supine bridging can be used to develop gluteal and lower abdominal strength, especially when done, one legged. with the thighs consistently parallel. Whilst modified planks and side planks can be used to develop arm, gluteal and abdominal strength simultaneously. The following example from a client with pelvic pain demonstrates the muscle synergies required, across the body, and in particular around the pelvis, for functional integrity. These exercises and modified versions of these can be used to improve climbing ability and agility. Functional exercises In climbing, ideally there are three points of contact, meaning that three points are either statically or dynamically stabilising whilst a limb is moving off the rock. The following describes a series of exercises for stability whilst moving various body parts Modifications can be made into climbing patterns, such as semi squat rather than sitting To reduce a "poked chin" the deep neck muscles need activation and the thoracic rings require elevation through Alexander technique and lateral diaphragmatic breathing Clinical observations Clinically, people fall into two broad categories - the hypermobile or the hypomobile. Hypermobile people generally work with their ballistic power generating muscles, using inertia to stabilise. These ballistic muscles can be long and strong but also long and weak if they haven't been appropriately conditioned. Hypomobile people tend to use their slow twitch endurance muscles and have short tight ballistic muscles. General rule of thumb is that 'floppies' need to work on endurance and stability, whereas 'stiffies' need to work on their flexibility and ballistic power. It is also possible to have hypermobile soft tissue (lax joints) but tight protective overlying muscles. Floppies tend to be good at 'pulling' into themselves, whereas 'stiffies' tend to be better able to push away. Ideally, individuals should work at what they aren't naturally endowed with to gain a 'musculoskeletal' protective balance. Frequently, one finds the 'floppies' in the yoga class and the stiffies in the pilates class when it really should be the other way around. Interested readers should read the Joint Hypermobility Syndrome and Ehlers Danlos Syndrome section elsewhere on this website. Too much pulling, with too little stability can lead to shoulder subluxation and even posterior dislocation. These shoulders need to have the soft tissue at the back of the shoulder 'buffed up' and be very conscious of 'scapula setting' when commencing movements. Ideally, muscle synergies are developed where the nett gain of all muscles working at their most efficient level to gain a mutually beneficial movement outcome is what is desired. In such a scenario, the distinction between agonists and antagonists, postural muscles and ballistic muscles becomes superfluous, let alone one body part being dominant over another. Interested readers should read 'game theory' and 'deterministic chaos' elsewhere on this site Voluntary Posterior Shoulder Subluxation : Clinical Presentation A 27 year old male presented with a history of posterior shoulder weakness, characterised by severe fatigue and heaviness when 'working out' at the gym. His usual routine was one which involved sets of 15 repetitions, hence endurance oriented rather than power oriented. He described major problems when trying to execute bench presses and Japanese style push ups. https://youtu.be/4rj-4TWogFU In a comprehensive review of 300 articles on shoulder instability, Heller et al. (Heller, K. D., J. Forst, R. Forst, and B. Cohen. Posterior dislocation of the shoulder: recommendations for a classification. Arch. Orthop. Trauma Surg. 113:228-231, 1994) concluded that posterior dislocation constitutes only 2.1% of all shoulder dislocations. The differential diagnosis in patients with posterior instability of the shoulder includes traumatic posterior instability, atraumatic posterior instability, voluntary posterior instability, and posterior instability associated with multidirectional instability. Laxity testing was performed with a posterior draw sign. The laxity was graded with a modified Hawkins scale : grade I, humeral head displacement that locks out beyond the glenoid rim; grade II, humeral displacement that is over the glenoid rim but is easily reducible; and grade III, humeral head displacement that locks out beyond the glenoid rim. This client had grade III laxity in both shoulders. A sulcus sign test was performed on both shoulders and graded to commonly accepted grading scales: grade I, a depression <1cm: grade 2, between 1.5 and 2cm; and grade 3, a depression > 2cm. The client had a grade 3 sulcus sign bilaterally regardless if the arm was in neutral or external rotation. The client met the criteria of Carter and Wilkinson for generalized ligamentous laxity by exhibiting hyperextension of both elbows > 10o, genu recurvatum of both knees > 19o, and the ability to touch his thumb to his forearm Fingers, elbows and wrists are also common places for climbing injuries. Taping can be particularly useful in protecting and unloading tendinous structures. Conclusion Seek guidance from your physiotherapist as the ultimate aim is to improve your power-weight ratio without inducing an injury. An optimal combination of strength, stability, and mobility needs to be acquired across the the entire body. The following videos should give you an insight of some of the things which are possible. Laterality of thought, improvisation and proper progression of exercise should allow refinement of climbing technique as well as reduce the risk of injury. Hip stabilisation and thoracic mobilisation Several exercises exist which stabilise the hip and shoulders whilst mobilising the thorax. Swiss Ball exercises can also be used to improve thoracic ring stability Thoracic strengthening regimes should be instigated to maintain the ring alignment Stretching regimes - 'don't let the tail wag the dog' Many people stretch their limb muscles. However, if the thorax is the 'driver' of limb muscle tension, then the thorax needs to be nullified beforehand and/or involved in the process of stretching. For example both hamstrings and quadriceps can be stretched with lateral flexion and lateral breathing of the diaphragm. Classic moves out of yoga such as the 'down dog -> high plank -> warrior pose -> triangle' can involve rib cage movements. Don't forget the calf muscles! Summary of leg, back and shoulder exercises Front, back, inside, outside and spiral 'slings' References Shoulder stability : https://www.back-in-business-physiotherapy.com/shoulder.html Hypermobility : https://www.back-in-business-physiotherapy.com/we-treat/ehlers-danlos-syndrome.html Joint Stability : https://www.back-in-business-physiotherapy.com/stability.html Game Theory and Cortical Resources : https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-the-immune-system-during-covid-19.html Pelvic - Hip - Lumbar stability : https://www.back-in-business-physiotherapy.com/we-do/muscle-energy-techniques.html Thorax : https://www.back-in-business-physiotherapy.com/we-treat/thorax.html Conceptualised whilst working and living in the mountains of Switzerland and the Blue Mountains, west of Sydney, NSW, Australia (!988-2001) Uploaded : 13 October 2020 Updated : 11 December 2020 Read More -

Hip pain in the elderly
Hip pain in the elderly Joint pain in the elderly population is a common complaint, with women being affected more often than men. There are several causes of hip pain amongst the elderly. We’ve put together this quick-fire list to inform you of what can cause hip pain in our senior citizens. Joint disease One of the most common causes of hip pain in the elderly is joint disease that leads to degeneration of the joint surfaces and results in a poorly moveable joint. The most common condition affecting the hip is osteoarthritis (OA), affecting approximately 25% of the population. The hip is a weight-bearing joint and through a lifetime has to withstand a great deal of force passing through it on a daily basis. Many factors in a person's life can lead to the onset and progression of OA in the hip joint. An injury to the hip earlier in life can kick start a process of early degeneration leading to poor movement and the development of pain as a person journeys through the second half of life. Other factors that may lead to the development of hip OA include obesity and or poor exercise regimes (or lack of exercise altogether). Other forms of joint disease that can cause hip pain include rheumatoid arthritis (RA), gout and pseudogout. Bursitis The word ‘bursitis’ means inflammation of a bursa. A bursa is a small, fluid-filled sac found throughout the body around joints and areas of high movement to reduce friction. There are several bursae found around the hip. These are usually located between a bone and tendon (or other tissues) and help to maintain smooth-moving joints. Weakness or long-standing dysfunction of the gluteal and other hip-related muscles (often seen in the elderly) can lead to compression of the bursae which increases the load on them. Over time and repetition of movement, the bursae can become inflamed and cause pain, often felt on the bony, outside part of the hip. Bursitis can be treated with hands-on therapy and exercise prescription aimed at strengthening and improving movement at the joint. Frequently, bursitis has a immune-metabolic origin. Clinically, I noticed this when working with young elite Swiss sports people back in the early 1990's, that they could suddenly develop bursitis which invariably involved some sort of predisposing immune compromise. Commonly, this involved a case of diarrhea or a cold or similar, in the 6 weeks prior to the onset of the bursitis. I've continued to notice this trend across the spectrum of ages and physical activity in the decades since. A similar trend exists for tendinopathy as well. where scientific research has demonstrated invasion of immune and fatty substances. Moreover, the bursitis and tendinopathy usually co-exist. Please see the shoulder section of this website for details on the latter and see the section on immune system and chaos for the former. Importantly, the gut biome should be consider in either case. The use of pro-biotics may be considered, such as sauerkraut, acidophilus, etc Tendinopathy Tendons join muscles to bones. As we age, the health of our muscle and tendon tissue declines and the efficiency of movement is affected. Similarly to bursitis, long-standing muscle dysfunction because of a failing hip joint can place excessive load on the tendon which attaches the muscle (e.g. the gluteal muscles) to the thigh-bone. If strengthening of the muscles and tendons is not achieved in the early stages of injury or disease, the fibres that make up the tendon become degenerated and deranged, resulting in a condition known as tendinopathy. This affects the tendon’s ability to withstand high loads passing through it and can lead to pain, regularly felt before and after exercise or movement. Long standing tendinopathy can lead to a tear which is common in older persons and can be the cause of much disability. Lower back dysfunction This is a very common cause of hip pain in the elderly population. As we age, our spines and the various tissues that play a pivotal role in its functioning can become degenerated. If a degenerated bone or joint in the spine presses on a nerve coming out of the spine, it can lead to a phenomena known as ‘radicular pain’. This is pain that may be felt in the hip (or other areas of the lower limb) but actually the problem lies in the lower back. Fracture Due to the increased rates of conditions including osteoporosis (loss of bone mass) and sarcopenia (loss of muscle mass), we are more prone to falling as we get older. A fall onto the outside of the hip can easily result in a fracture of the neck of the thighbone, close to where it attaches into the pelvis. As with any bone fracture, pain is a common symptom. A hip fracture may require surgical intervention and can greatly impact the health of an elderly person with increased risks of infection and death posing a real threat. If you have hip pain and are concerned, please call us today on 02 9922 6806 to book your appointment immediately. Stay safe everyone! Uploaded : 2 October 2020 Read More -

Meniscus tears
Injury blog: Meniscus tears Hello readers and welcome to another of our monthly health blogs. This month we take a look into the world of knee meniscus injuries. Studies from the US report approximately 61 in every 100,000 people experience a knee meniscus injury every year. You are more susceptible to injuring a meniscus in your knee if you participate in sports such as football (all forms), basketball, netball, skiing, baseball and wrestling. There is also a high rate of meniscus injury seen in those who work in the military on active duty. Essentially any job or sport that requires lots of squatting and kneeling can leave you open to an injury of this kind. But what is a meniscus? Anatomy The meniscus are found inside the knee joint, nestling nicely between the thigh and shinbones. They are crescent-shaped pieces of toughened tissue (a type of cartilage) and there are two in each knee. One sits on the outside part of the knee joint (i.e. lateral meniscus) and one sits on the inside part (i.e. medial meniscus). They act as shock absorbers to the various loads and forces that pass through the knee during movement. They also have a slightly wedge-shaped appearance being thicker around the outside compared to the inside, and this provides a deepening of the joint surface to allow for a more snug-fit joint. The top of the shinbone is quite flat compared to the very rounded ends of the thighbone… The meniscus help to stabilise this slight mismatch of joint surfaces. Causes of a tear The most common cause of a meniscus tear is an excessive or forceful twisting of the knee whilst the foot is planted on the ground. This might happen as a result of landing awkwardly from a jump, or from the force of another person or opponent’s body acting on the knee. During this type of movement, if the force is too much for the meniscus to withstand, tearing may occur. The medial (inside) meniscus tends to be injured more than the lateral (outside) meniscus. This is because the medial meniscus attaches to other structures inside the knee joint, leaving it less mobile to forces acting on it compared to its lateral counterpart. Signs and symptoms The experience of a meniscal tear will vary from person to person depending on the cause. A young footballer who has been injured during a tackle with high forces involved will likely present in a great deal of pain with a swollen and restricted knee. Injuries sustained in this way are likely to be more severe with associated ligament injuries as well. On the flip side, an older person who has been gardening for the weekend spending lots of time squatting and kneeling may present to the clinic with a very different picture. There may be no high force movement involved, but instead the tear has occurred due to degenerative changes that have occurred to the cartilage tissue. Symptoms in these types of injury are less likely to be so acute and may only appear 24-48 hours down the line. Signs and symptoms you might expect from a meniscal tear may include any or all of the following: • Pain when walking, squatting or jumping• Restriction of the knee joint with or without swelling• Knee joint locking• A popping or clicking sensation (often following an episode of locking)• A feeling that the knee may give way • Tenderness around the line of the knee joint where the tear has occurred Diagnosis and treatment The first thing to do if you have injured your knee is to see a physiotherapist as soon as possible. A painful, swollen, restricted and inflamed knee following an incident is a sign something is not right, so seek help quickly. We will ask questions about what has happened and examine your knee closely. Some people will be able to move around well, others with a severe injury may be more limited. The management of meniscal tears will vary depending on how the injury happened (i.e. are we also dealing with a ligament injury?), and the age and goals of the patient. In some instances, we might suspect a small tear and a patient is presenting with pain but has good overall movement and doesn’t have any of the more severe symptoms such as locking or giving way. In these cases,; we’d use hands-on treatment and exercise prescription in order to strengthen the knee and restore full function through massage, mobilisation and whole body movement. In instances where we suspect a large tear and a patient is presenting with high amounts of pain, restriction and locking and/or giving way in the joint, we may first need the assistance of some imaging or surgery (i.e. an arthroscope) to determine the severity and clear the knee of any large tears. Some tears require removal of the cartilage tissue whereas some can be repaired. The surgeon will always try to retain as much of the meniscus as possible to reduce the impact on knee mechanics following recovery and for the future. Regardless of the initial management, rehabilitation will aim to: • Reduce pain and increase range of motion to the knee• Improve strength of the quads, hamstrings, calves and other knee and hip related muscles• Return to sport or previous duties as soon as possible without risking further injury Seeing us as soon as possible will help to limit complications and help get you back to 110% (we always like to get you back fitter than you were before the injury!) at the earliest possible opportunity. Whether your goal is to garden or return to kicking goals, we can help get you there. Call us today on 02 9922 6806 to book your appointment. And squat! Uploaded : 27 September 2020 Read More -

Sacroiliac Pain - imaging and stability testing exercises
Sacroiliac Pain - musculoskeletal physiotherapeutic clinical reasoning using imaging and stability testing exercises The sacroiliac joint (SIJ) is designed to transfer the load from along muscle energy straps of the limbs into the torso. The torso, hip and pelvis are constructed into a series of slings (front, back, side, inside and spiral) which supports those structures receiving the load. Consider a person lying in a hammock and you have an analogy, for skeletal support, by the soft tissue structures of the body. Andre Vleeming described these 'slings' in the 1990's and body work practitioners such as Ida Rolf (and Thomas Meiers) referred to myofascial trains in the 1970's. As such, a series of exercises can be used to assess and treat stability across the SIJ. People interested in the 'energy straps' across the lower limb should look at 'inverse dynamics' elsewhere on this site. Inverse Dynamics Those interested in 'hands on' treatment of pelvic dysfunction should look at : https://www.back-in-business-physiotherapy.com/we-do/muscle-energy-techniques.html elsewhere on this site Uploaded : 19 September 2020 Read More -

Tips for sleeping like a baby
Tips for sleeping like a baby Do you consistently struggle to get a good night’s sleep? Well lucky for you we’ve compiled a helpful little guide to getting the best Zzz’s’s possible. It’s easy to get caught up in life and develop nasty habits that can affect our body’s ability to get itself prepared for lights-out time. Read on for tips on taking control of your sleep. • Create a routine: Routine equals consistency. If it’s possible, try to stick to a routine of going to bed at the same time every day. This would ideally run throughout the whole week, including weekends. There will always be occasions where you won’t be able to stick to this… meals out, parties, etc. But when that happens, try to get straight back into your routine as soon as possible. Your body will respond well to routine and you may find falling asleep easier once you are locked into a pattern. Think about including some relaxation time each night where you snuggle up with a book or drink a soothing cup of chamomile tea. • Create the ideal environment: What is your bedroom doing for you? Is it too hot or too cold? Temperature is important for creating the ideal sleep environment. The Sleep Foundation recommend a room temperature between 15.5 – 19.5 degrees Celsius for optimal sleep. Also, think about keeping your bedroom as noise and light-free as possible. And of course, a comfortable pillow and mattress to support your body is a must! We can help find a suitable option when it comes to pillows and mattresses. Chat to us next time you’re in the clinic. • You get out what you put in: Try to avoid smoking, drinking alcohol and eating a hearty meal before bed. Aim to eat your last meal a minimum of two to three hours before you hit the sack. All of these things can lead to disturbed sleep and increase the risk of wak-ing up tired the next day. The saying sticks… you get out what you put in! • Bedroom = sleep: This is a big one. Technology is finding its way into our bedrooms more and more. For many people it’s the only time they get to switch off and check their social media accounts or catch up on emails. But we recommend avoiding screens. Keep your bedroom for sleep and sleep only. If you have to use a screen before bed, set aside time earlier in the evening to get this work done. The light given off by tablet or phone screens stimulates the brain, when in reality, you should be trying to relax, allowing it to switch off. • Avoid daytime naps: We all know how nice it is to have a little siesta during the day. But there is logic in the assumption that if you struggle to sleep through the night, removing your daytime nap could help to regulate your night-time sleep pattern. • Exercise regularly: Emerging research into the effect of exercise on sleep shows that light-to-vigorous exercise helps a person to fall asleep faster and improves the overall quality of sleep. It is thought that exercise helps to increase the amount of deep sleep you get, as well as helping to de-stress the mind to allow for a more relaxed cognitive state. We suggest not trying to implement all of these at once. Why not pick just one or two changes and work with them for a few weeks. It may take some time to find what works best for you. References1. Help Guide. 2019. How to sleep better. [Online]. Available from: https://www.helpguide.org/articles/sleep/getting-better-sleep.htm. [Accessed 15 Jul 2020]2. SleepFoundation.org. 2020. Healthy sleep tips. [Online]. Available from: https://www.sleepfoundation.org/articles/healthy-sleep-tips. [Accessed 15 Jul 2020]3. Johns Hopkins Medicine. 2020. Exercising for better sleep. [Online]. Available from: https://www.hopkinsmedicine.org/health/wellness-and-prevention/exercising-for-better-sleep. [Accessed 27 Jul 2020] Uploaded : 25 August 2020 Read More -

Hip flexor injury: Contusion vs strain
Hip flexor injury: Contusion vs strain Hey everyone! This month we are drawing focus on injuries that affect our hip flexor muscles. Injury to the hip flexor muscles can lead to pain felt in the front of the thigh region, as well as the hip and groin. Hip flexor injuries are common in sports, including football (all forms), basketball, hockey and athletics. What are your hip flexors? Your hip flexors are a group of muscles that move the thigh forwards and outwards, in front of the body. The main muscles involved in the movement of hip flexion include: • Rectus Femoris (one of the quadriceps muscles)• Iliacus and psoas (pronounced ‘so-ass’ — collectively known as the ‘iliopsoas’ muscle)• Tensor Fascia Latae (or TFL)• Sartorius• Some of the groin muscles known as the ‘adductors’ The most commonly injured hip flexor muscle is the rectus femoris muscle (pictured above). This is the muscle that runs from the pelvis, down the centre front of the thigh, to below the knee. This muscle not only flexes the hip, but also extends (or straightens) the knee. Types of injury The most common injuries of the hip flexor muscles (i.e. rectus femoris) include contusions and strains. Contusion: A contusion is an area of skin and underlying tissue that has been damaged by a blunt force trauma. This may come in the form of an opponent’s knee during sport, or an object like a hockey puck striking the thigh. A contusion is also known as a ‘cork’’. The impact of an object causes the tiny blood vessels under the skin and in the muscles to break and bleed. The blood collects into a space around the impacted muscle fibres creating a pool of blood. A bruise appears on the skin where the impact has occurred. Strain: A strain is a tearing of muscle fibres usually caused by a force too great for the muscle to withstand. This may occur during an explosive movement including kicking, jumping or running. Strains are either partial (where some muscle fibres tear and others remain intact — known as Grade 1 or 2 strains depending on severity) or complete (where every muscle fibre tears — known as a Grade 3 strain or in the old nomenclature Grade 3 partial complete full thickness tear, grade 4 complete tear. The latter is still commonly used in calf tears). Strains most commonly occur at the location where the muscle merges into a tendon. In the case of the rectus femoris muscle which runs vertically down thigh, strains usually occur at either the hip-end or the knee-end of the muscle. It can be difficult to distinguish between a contusion and a strain as many of the signs and symptoms are similar. A thorough case history which takes down information including how the injury occurred and how it developed over time can help your physio come to an accurate diagnosis. Signs, symptoms and features The following table compares the features seen with a typical contusion versus a strain: Treatment The way we treat a contusion and a strain are very similar. The length of treatment tends to increase for more severe strain injuries, but the principles of treatment are largely the same. As with any acute injury, the first line of treatment is to control the bleeding and swelling under the skin. This includes protecting the body part from worsening injury, loading the part appropriately (i.e. being on crutches vs full weight-bearing), ice, compression and elevation of the affected body part. Gentle stretching and contraction of the affected muscle is allowed if tolerable. The next stage is to get the knee and hip joints back to full, pain-free range of motion. We can help here with some hands-on massage and joint mobilisation. We’ll kick up the stretching and increase the amount of strength training too. You should be able to use an exercise bike and go swimming at this stage, but we’ll advise when you can do it safely. When you are back to full weight-bearing exercises with full range of motion, the aim is to progress strength and flexibility exercises gradually over a period of weeks. These will include a combination of agility, jumping and balance exercises. When you reach your exercise goals, we’ll advise when return to training/full sport participation is appropriate… If that’s what your ultimate goal is. The most important thing is to ensure the return to sport/activity does not happen too soon. Strains commonly recur, usually as a result of rushed or incomplete rehabilitation before returning to the sports field. So… taken a hit or felt a tear? Give us a call on 02 9922 6806. If you need help with a hip flexor injury, please do not hesitate to get in touch immediately. Early treatment is always preferred over the waiting game. With our help, you’ll be back hopping, skipping and jumping your way to a gold medal in no time at all. References 1. Healthline. 2019. Understanding hip flexor strain. [Online]. Available from: https://www.healthline.com/health/hip-flexor-strain. [Accessed 15 Jul 2020].2. Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. Australia: McGraw Hill Education3. Margo, K. et al. 2003. Evaluation and management of hip pain: An algorithmic approach. The Journal of Family Practice. 52 (8). Available from: https://mdedge-files-live.s3.us-east-2.amazonaws.com/files/s3fs-public/Document/September-2017/5208JFP_AppliedEvidence1.pdf Uploaded : 25 August 2020 Read More -

Whole Body Vibration
Whole Body Vibration (WBV) by Martin Krause In 2009, we (Alfio Albisini and myself) published the first book (DOI: 10.1016/B978-0-7020-3173-1.X0001-4) on the therapeutic application of Whole Body Vibration (WBV). Since that time, new research has described, some new and novel mechanisms and effects of WBV. Introduction Most human movement involves low amplitude, moderate frequency vibration (<1g, 30-90Hz). Such mechanical loading results in what is termed mechano-transduction. The transition of a mechanical load to a hormonal response, involves the stimulation of hydroxyapatite crystals (interspersed amongst a collagen matrix), which in turn has an influence on osteoclastic (bone mineral resorption) versus osteoblastic (bone mineral forming) activity. As such, the use of WBV therapy, in the treatment of osteoporosis in the frail elderly, or young individuals with osteogenesis imperfecta, has become popularised in recent decades. Additionally, within the fitness industry, entire gym programs exist, which incorporate WBV machines (e.g. Galileo), to improve strength and agility. Although, superimposing exercises on WBV is very popular, the effect of 4 weeks of heavy strength training, superimposed with WBV, have shown equivocal results, when examining corticospinal neuronal drive (Weigal AT & Kidgell DJ 2012 The Scientific World Journal Article ID 876328 https://doi.org/10.1100/2012/876328 ). Twelve participants (6 male and 6 female aged between 18 and 27) performed four sets of six to eight repetitions at 80% of 1RM, with three minutes recovery between sets. WBV was set at 35hz and 2.5mm displacement. It may well be, that WBV has more obvious effects on people with greater functional impairment. One investigation, in poeple with strokes found, the effect on muscle strength and balance and gait function, were small. However, the effect for bone metabolism and spasticity were moderate, suggesting that WBV training may provide a safe, alternative treatment method for improving the symptoms of stroke (Park YJ 2018,BioMed Research International Article ID 5083634 https://doi.org/10.1155/2018/5083634 ). Mechanisms It has been suggested that WBV works via at least two mechanisms. The first, traditional mechanism, was a direct influence on muscle mechanics. It was thought that the stimulation of working muscles stimulated the hydroxyapatite crystals and hence the osteocytes in the bone, thereby ameliorating osteopenia and osteoporosis. The more contemporary thought, is that WBV has a direct influence on the stimulation of the osteocalcin, residing on the bones, which in turn acts on the muscles, preventing or ameliorating sarcopenia, which then provides the functional strength needed for weight bearing activities and sporting accomplishments. It could obviously be both, where a cycle exists, of one influencing the other. If this were the case, then in functionally impaired people, the direct influence of the vibration on the bone will be more critical to muscle mass than in the athletic environment, where the exercises themselves, accompanied by the vibration, has a more profound direct effect on muscles, over the indirect effect from the bone? Frail elderly and athletes Apart, from the therapeutic effects on the bones and muscles of the frail elderly, WBV has also been used to improve sporting performance, in athletes, through the stimulation of muscle. At lower frequencies (<20Hz) WBV is thought to help with muscle relaxation and hence can be used during stretching routines. WBV has also been used to improve explosive strength and postural control thereby enhancing athletic performance (Fort A, et al 2012, J Strength Cond Res. 26, 4, 926-36). At higher frequencies (30-50Hz), it's been used as an adjunct to plyometric (box jump) strength training, as it is thought, that each oscillation, is the equivalent to a jump, at a neurophysiological (muscle spindle receptor - spinal cord) level. The addition of functional exercises, to the passive WBV stimulation, probably brings higher center motor control in to play. In fact, investigators have demonstrated enhanced descending modulation after 10 minutes of WBV, as well as reduced spinal cord reflex activity in the soleus muscle (Krause A et al 2016 J Musculoskelet Neuronal Interact., 16, 4, 327–338). In another investigation, it was shown that WBV, during squat exercise, compared to no WBV, led to a corticospinal facilitation concomitant with intracortical modulation, thus describing increased intracortical inhibition and diminished intracortical facilitation (Mileva KN et al 2009, Exp Physiol., 94, 1, 103-16). One could assume that these results represent enhanced motor control. WBV has also been used, in a variety of other settings, to improve implant adherence to bone, in people with bone softening (Zhaoug et al 2015 Bone, 71, 17-24, https://www.sciencedirect.com/science/article/abs/pii/S8756328214003652) , used in neurological conditions, such as stroke (Tankisheva E, et al 2014, Arch Phys Med Rehabil., 95, 3, 439-46). and cerebral palsy (Ahlborg L, et al 2006, J Rehabil Med.,38, 5, 302-8), to improve balance and muscle spasticity, to improve gait after spinal cord injury (Ness LL, et al 2009, Gait Posture. 30,4, 436-40), as well as being used to improve cosmonauts musculoskeletal health, after prolonged space missions. Children with haemophilia 30 children (aged 9-13 years) with haemophilia. were divided into 2 groups, comparing standard physiotherapy to WBV (30-40Hz, 2-4mm amplitude, 15 minutes, 3 x wk for 12 weeks) in conjunction with standard physiotherapy. Researchers found that children in the vibration training group showed significant improvement in all outcomes including quadriceps strength, bone mineral density, and functional capacity, which was evaluated using a six-minute walking test. Children in the vibration training group were able to walk an average of 325 meters in six minutes compared to only 290 meters in the standard physiotherapy intervention group (El Sharmy S 2017 J Musculoskelet Neuronal Interact, 17, 2, 19-26). Osteocalcin Traditionally, bone has been considered an inert structure. Purely, providing the frame where upon muscles exert their work, through the bony levers. However, contemporary evidence suggests that bones are more than mere mechanical levers, where in fact the reverse applies, whereby bone acts on muscles. It's been suggested that bone remodelling is an energy intensive process which requires a sensor and regulator of energy needs. This hypothesis led to the demonstration a few years ago that osteocalcin, an osteoblast-derived protein, was a hormone regulating glucose and energy homeostasis (Lee NK (2007) Cell, 130, 456-469). Such an energy system, would suggest a gut-bone and a muscle gut axis. Indeed, gut-derived hormones such as glucagon-like peptides 1 and 2 and serotonin have been shown to regulate both bone remodelling and energy homeostasis (Henriksen DB et al (2009), Bone 45, 833-842; Ma, X et al (2013) Bone Miner Res, 28, 1641-1652; Sumara, G et al (2012) Cell Metab.,16, 588-600; Yadav, VK et al (2009) Cell 138, 976-989) Osteocalcin (glutamate derived decarboxylated structural protein), resides on the surface of bones, and has several interactions with organs, thus making bone an endocrine organ. Animal models, have shown that reduced osteoclacin leads to type II diabetes, obesity, and hypertension (Moser SC et al 2019, Front. Endocrinol., 10, January https://doi.org/10.3389/fendo.2018.00794). Matthieu Ferron & Julie Lacombe (2014) https://www.researchgate.net/profile/Mathieu_Ferron2 Additionally, the review (Moser et al 2019) suggested that reduced osteocalcin affects male fertility, muscle mass (especially in the presence of sarcopenia), cognitive ability, brain development and inflammation. Even, suggestions of effects on tumours has been entertained. Apart from the effect of osteocalcin, on insulin sensitivity, described above, additionally it has been shown, in vivo mice experiments, that osteoblasts have Glut 4 receptors metabolically involved in glucose absorption, at a rate similar to that seen in muscle (Li Z et al 2016, Endocrinology, 157, 11,4094-4103). Presumably, WBV can have a direct effect on osteoblasts as well as osteocalcin, suggesting a dual mechanism of action? Moser et al 2019. Front. Endocrinol., 10 January | https://doi.org/10.3389/fendo.2018.00794 WBV, insulin sensitivity, inflammatory markers and DNA injury in white blood cells Investigators (Yin H et al 2015 Springerplus, 4, 578, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4628131/), using an animal model, demonstrated profound effects, of WBV, on markers of inflammation and glucose metabolism/sensitivity. Improved Glucose Sensitivity Reduced Inflammation Indication of DNA injury in white blood cells markedly reduced in WBV Conclusion Since publishing our book in 2009, both human and animal research has shed more light on some of the significant beneficial effects of WBV. Furthermore, the mechanism by which it has such an effect, seems to reside within bone itself and osteocalcin in particular. Further research is still required to establish dose - responses in various population groups, from the frail to elite athletes. Never-the-less, currently, stimulation <20 Hz is considered to improve muscle relaxation. Stimulation in the range 30-50 Hz improves muscle power. Stimulation at higher frequencies (>1g and >50Hz) needs to establish a risk-benefit ratio in various population groups. Currently, when considering dose, we suggest a familiarisation period of 2 weeks, with short duration sessions (10-20 minutes), incrementally increasing these up to an hour in healthy population groups. A similar strategy can be employed during rehabilitation, so long as functional outcomes are being monitored, whereby incremental increases in dose, are reflected through demonstration of continued improvement. Individual technique and fitness levels, as well as the morphology of the person (muscle mass, floppy vs stiffy) will considerably influence the selection of dosage and the tolerability of the WBV stimulus. References https://www.sciencedirect.com/topics/medicine-and-dentistry/whole-body-vibration https://www.elsevier.com/books/using-whole-body-vibration-in-physical-therapy-and-sport/9780702031731 Uploaded : 23 July 2020 Updated : 26 July 2020 Read More -

The twists and turns of torticollis
The twists and turns of torticollis Hello readers and welcome to our August 2020 blog. This month’s topic is a neck condition known as ‘Torticollis’. You may have also heard this condition referred to as ‘wry neck’. What is Torticollis? Torticollis is a painful neck condition where one of the strong muscles on the side of the neck shortens, causing the head to twist and tilt out of its normal position. The muscle we are referring to is the ‘Sternocleidomastoid’, or SCM for short. It’s easy to locate this long ‘strap’ muscle… Turn your head to the left and the SCM pops out on the right-side of the neck. Trace a line from the base of your skull just behind the ear, down to the top of your breastbone and you should be able to feel the muscle. Although the name is a bit of a mouthful, it perfectly describes the at-tachment points for the muscle on the body: • Sterno- refers to ‘sternum’ which is the name of your chest / breastbone• Cleido- refers to ‘clavicle’ which is the name of your collar bone• Mastoid- refers to the ‘mastoid process’ which is a bony lump found behind the ear at the base of the skull There is a SCM muscle on each side of the neck. This muscle helps you to:• Turn your head to the opposite site• Touch your ear to your shoulder• Bend the neck forward• Tilt the head backwards• Breathe (it is an ‘accessory' muscle for breathing - kind of like a little helper to the main breath-ing muscles) Types and causes There are two main types of torticollis—congenital and acquired.Congenital torticollis means the condition is present at birth. This problem can develop in the mother’s womb if the baby’s head is held in an awkward position, or if the blood supply to the muscle is disrupted. Sometimes the bones in the neck do not develop properly and become fused together, this can also lead to a rare type of torticollis called Klippel-Feil Syndrome. Acquired torticollis means the condition develops after birth. The condition is common in both children and adults. Acquired torticollis can be caused by injury to the muscle, or the nerve that supplies electricity to the muscle. In the majority of cases, the cause is completely unknown. As with congenital forms, there are some rarer acquired types, including ‘spasmodic’ torticollis. This type is also known as ‘cervical dystonia’ and is a form seen in adults where all the usual symp-toms are seen, but may also come with a jerking type motion of the head caused by spasms in the SCM muscle. Signs and symptoms The signs and symptoms of torticollis depend on the type, but the main features include: • Neck pain and/or stiffness• An inability to move the head in the usual way• A tilted head to one side• Swollen and tender neck muscles• Uneven shoulder height• Headaches Treatment Parents reading this who have experienced torticollis with their newborn or young child will prob-ably remember the stress that comes with seeing their helpless little human with a seemingly un-changeable head position. It really is quite unsettling. The good news is that for the majority of cases, some focused regular stretching is all that’s needed to correct the head position and re-store the muscle to its full length. Young children usually respond very quickly to hands-on treatment. Some of the rarer congenital forms of torticollis can also be treated in a similar way, but these forms may also require the opinion of a surgeon who can perform a procedure to lengthen the muscle. As with a lot of conditions, surgery is a last resort and will only be considered when all non-surgical treatment techniques have failed. Other treatment techniques used for torticollis include:• Massage of shortened and tight muscles• Heat pack therapy to increase blood flow and relax tight muscles• Joint mobilisation and manipulation For people who live with a permanent or chronic torticollis, other complications are common. These include difficulties carrying out activities of daily living, depression, social isolation and chronic pain. Treatment should be from a multidisciplinary approach. This means that as well as seeing your physio for hands-on therapy, your doctor, psychologist, friends and family will all play a part. If you or a family member are struggling with torticollis, or a neck issue of another kind, please call us here at Back in Business Physiotherapy on 02 9922 6806 to arrange a convenient time to come in for a consultation. We’d love to help unravel the twists and turns of your torticollis and get your neck feeling relaxed and happy Uploaded : 20 July 2020 Read More -

Injury blog: Shoulder impingement
Injury blog: Shoulder impingement Do you have shoulder pain? Are you an office worker, professional athlete, hairdresser or full-time parent? These are just some of the types of people we see in the clinic who need help with shoulder pain. One of the most common complaints we treat here, at Back in Business Physiotherapy, is shoulder ‘impingement’ (aka subacromial impingement). “What is impingement?” we hear you ask. Read on to find out. Anatomy overview The shoulder is a pretty complex region of the body when it comes to anatomy and how it all works together to allow us to move. The connections between the arm bone ( humerus), collar bone ( clavicle), shoulder blade (scapula) and the rib cage, provide us with the perfect base for a limb that is able to move through an extremely wide range of motion… The most movement out of any other joint in the body. Having lots of movement is great because it means we can do lots of wonderful things like reach the back of our head to wash our hair and reach our backs too (like when tying an apron). In order to achieve this level of movement the shoulder has to be less stable, and this leaves it prone to injury. The arm bone and shoulder blade form the ‘ball and socket’ part of the shoulder, where a large amount of the movement takes place. The ligaments between these bones are quite loose and a group of muscles, known as the ‘rotator cuff’ muscles, help to keep the ‘ball’ of the arm bone po-sitioned correctly over the ‘socket’ of the shoulder blade, as well as aid with certain movements, including rotation or turning of the arm. Small spaces..... Over the top of the ball and socket joint sits the ‘acromion’, which is a bony prominence of the shoulder blade which creates a roof over the joint. Between the top of the ball and the bottom of the acromion is a small space known as the ‘subacromial space’. Some tendons of the arm muscles that create movement of the shoulder pass through this space on their way to their at-tachment site on the bones. There is also a ‘bursa’, which is a small sac of fluid which helps to keep movements around joints smooth and frictionless. There is quite a lot of tissue all crammed into one small space, and this is an important factor in the development of impingement. Common causes of shoulder impingement include:• Repetitive overarm throwing or other above-shoulder movements• Long-standing poor posture or poor movement patterns• De-conditioned or weak shoulder muscles from leading a sedentary lifestyle• Heavy lifting Immune metabolic compromise can also affect the tendon-bursa complex. These include high cholestereol, diabetes, irritable bowel syndrom, etc Anything that leads to the structures which pass through the subacromial space becoming irritated and inflamed can cause impingement-related pain. Inflammation can lead to swelling of the tissues in the small space and when we move our arm up or out to the side, these tissues get pinched between the bones, and we feel pain. Any of the above-mentioned structures can be-come inflamed, but there is rarely just one tissue solely responsible. If the tendon of a rotator cuff muscle is inflamed, there is every chance the bursa will also be inflamed. Signs and symptoms Signs and symptoms of shoulder impingement include:• Pain with arm movements (particularly movement in front and out to the side of the body)• Pain with shoulder rotation• Pain that radiates down the outside of the upper arm• Reduced shoulder range of motion Treatment At the root of most cases of shoulder impingement is poor and inefficient shoulder movement. When you come to see us for treatment, we will look beyond the shoulder to other areas of the body, like the spine. The neck and mid-back areas of the spine are regularly restricted and need some help to move well again. Once the spine moves well, shoulder function improves too. The shoulder blade also needs to sit correctly over the rib cage in order for the ball and socket joint (and other joints) to work efficiently. Weakness of the muscles which stabilise the shoulder blade on the rib cage can lead to poor positioning of the blade during movement, so we will aim to improve this by giving you focused strengthening and stability exercises. A solid base = good, smooth movement. Through a combination of us using our hand techniques (like massage and joint mobilisation), progressive exercises and lifestyle changes, you can expect to see positive changes quite quick-ly. The end goal of ensuring your pain doesn’t return is always a lengthier process and requires dedication from yourself (and us) to make sure the changes we make early on stay in place for time to come. We are here to help you every step of the way. Shoulder pain? Call us today on 02 9922 6806 Uploaded : 3 July 2020 Read More -

Shoulder injury blog: Labral tear
Shoulder injury blog: Labral tear The shoulder is one of the most complex joints in the body. It is made up of a total of four joints, numerous ligaments, joint capsules, muscles and other soft tissues. Movement at the shoulder is a complicated process and it relies on the controlled function of all the involved muscles and joints for that movement to be efficient and complete. Our shoulders are the most mobile joints in the body which is great for us because it means as humans we get to partake in fun activities like throwing sports, gymnastics and dancing, as well as movements we generally take for granted like being able to do up our bra’s behind our backs. This wide range of movement is only possible because the shoulder is less stable when compared to other joints in the body, leaving the shoulder prone to injury. This blog specifically focuses on an injury that relates closely to the ball and socket part of the shoulder joint. If you are into throwing sports, you may be familiar with it… It’s called the labral tear. A bit of anatomy… There are two main ball and socket joints in the body, found at the shoulder and the hip. Both work where a rounded ‘ball’ of one bone fits into a hollowed ‘socket’ of another. At the hip (the strongest joint in the body), the socket is very deep, and the ball part fits quite snuggly into it. This is a very stable joint. The socket in the shoulder is very shallow by comparison, and the ball part is still quite large. This is what gives the shoulder its lack of stability. Both the shoulder and the hip sockets are deepened and supported by the presence of a labrum — a rounded soft-type of cartilage. In the shoulder, the labrum completely surrounds the rim of the socket creating a ring. The very top part of this ring also acts as the attachment site for one of the tendons of the biceps muscle — a powerful mover of the shoulder and elbow joints. How does a labrum tear? The main ways labral tears occur are: • Repetitive movements such as overhead throwing• Carrying heavy objects• Dropping and catching heavy objects A tear can occur over time as the tissues degenerate over time and become weaker, or it might be from one single, forceful event. In most cases there is usually a combination of both degeneration and a large force which becomes the ‘straw that breaks the camel’s back type of scenario. As the biceps tendon attaches to the socket through the labrum, any large force that pulls on the biceps tendon (like suddenly catching a heavy object) can lead to the tearing of the labrum itself. The most common type of tear occurs across the top of the labrum from front to back, and these are known as SLAP (i.e. Superior Labrum Anterior Posterior) tears. Signs and symptoms If you have sustained an injury to the labrum in the shoulder, you may notice any or all of the following signs and symptoms: • Pain during shoulder movement (especially overhead and behind back movements)• Restricted shoulder movement• Popping, catching or grinding during shoulder movements• Tenderness at the front of the shoulder Depending on how you were injured, how severe your symptoms are, and your personal circumstances regarding work and home life, you may be sent for some imaging to confirm the tear. The tests we perform in clinic when we assess you do not always give us all the information we need to determine the best plan of action. A combination of clinical tests and imaging may give us a clearer picture of what’s going on. Can it be treated by a physio? Yes, but this completely depends on the severity of the injury and what your goals are. In most cases it is recommended that conservative therapy from a physiotherapist is tried first. Many athletes who have a labral tear can return to playing to some capacity with a non-surgical approach. The treatment aims to return the shoulder to full, pain-free range of motion through hands-on massage, mobilisation and rehab exercises that focus on range, control and strength of the shoulder girdle. For severe tears, you may require the opinion of a shoulder specialist. A labrum is not great at healing itself and sometimes needs help from a surgeon to return to normal. A professional athlete wanting to return to sport may choose this pathway, but a non-athlete who has no desire to throw a ball seriously again may be able to avoid surgery altogether. If you have a diagnosed labral tear, or have recently injured your shoulder and need help, we recommend coming to us at Back in Business Physiotherapy where we can discuss the best course of action for you and your circumstances. Upload : 2 June 2020 Read More -
COVID mental health check-in
COVID mental health check-in With the coronavirus outbreak still affecting millions around the world, we thought it would be a good time to check-in and see how you are all going. The news is pretty grim at the moment and you may be finding yourself asking the question, “When will there be any good news?!” This day-to-day bombardment of the effect of the virus across the world is enough to get the happiest of people down. We’re here to make sure you are keeping your mental health in check. We ask you the question… What are you doing to look after your mental health? These have been difficult and stressful times for many of us. Some of us are starting to come out of strict lockdown restrictions, some of us are still feeling the effects, and many of us will feel these ef-fects for some time to come. It’s good to talk If you are struggling on a daily basis and this pandemic has had a real effect on your mental health, you are not alone and help is out there. Being made to stay away from family members and friends is tough and some people, especially the elderly, will have found this extremely diffi-cult at times. Please talk. A phone call or face-to-face video call (technology is great these days!) is a simple way to stay in touch with loved ones. Speak to someone close to you if you are struggling with personal circumstances. Getting a load off your chest is sometimes enough to make you feel relief, even if it doesn’t solve the root cause of the problem. We understand that your problems may run deeper than this and talking to a loved one is simply not enough. The good news is there are lots of great people out there who are trained to work through such things with people. And even if you cannot get a one-to-one session in person where you live, many mental health professionals including life coaches, counsellors and psychologists are running phone or video/telehealth sessions with their clients. Alternatively, chat to your GP or give Beyond Blue a call on 1300 22 4636. Please do not suffer in silence. Simple tips for keeping your mental health in check Want some other ideas to help keep your mental health in check? Check out our list below for some go to’s: • Exercise: It’s simple and well researched. Exercise helps to maintain good mental health. Even in lockdown, find a space in the house or outside in the garden and just move. Squat, lunge, hop, skip, jump, dance… We don’t care what it is, just move regularly (and safely please!).• Eat well: Keep your diet clean and hydrate every day and you’ll be doing your bit to keep the body and mind functioning well. Vegetables and fruit of the green leafy and berry va-rieties are packed with nutrients that can help keep the brain healthy.• Go to time-out: No, we don’t mean the naughty step, more so a quiet place where you can be with your own thoughts without the distraction of TV, tablets and other types of media. Read a book, take a bath, give the eyes and ears a rest from it all. It may be hard to break your screen habit, but trust us... It’s refreshing!• Get out the colouring pencils: Yes adults, we are talking to you. Colouring is becoming a very popular ‘escape’ for millions of adults around the world. It has been shown to help reduce the effects of anxiety and stress. Get to your local book store or newsagent to-day, support local shops, and start getting creative (or if you’re unable to do so safely, order online).....or do an amazing puzzle. They are addictive!!! Our message today is simple. Life is sometimes hard, but there is always action you can take to reduce the impact this has on your mental health. Talk. Move. Engage. Relax. Enjoy and stay safe. The Team from Back in Business Physiotherapy Uploaded : 2 June 2020 Read More -

Injury blog: Abdominal hernias
Injury blog: Abdominal hernias Mention the word ‘hernia’ and most people will think of something painful sticking out of the belly region. You’ll be pleased to know this is not always the case. Many cases are completely pain-free and are only noticeable on a person when they are in a particular position. At other times there may be no other visual sign that a hernia even exists! Read on for more information... What is a hernia? A hernia is a protrusion of the abdominal contents (i.e. intestines) through a weakened or damaged part of the muscle or tissue that holds it in place. Hernias are commonly found in the abdominal region of the body; that area between the bottom of the rib cage and the hip / pelvic area. Abdominal hernias can be broken down into two locations: • Abdominal wall location: Hernias that occur through the wall of the abdomen on the front of the belly region• Groin location: Hernias that occur lower down in the abdomen around the groin region Abdominal wall location There are a few different types of abdominal wall hernias with the most common being: • Incisional: These hernias occur in and around a scar or ‘incision’ left over from a previous abdominal surgery. During surgery, the muscles of the abdominal wall are cut to allow the surgeon to access the inside of the abdomen. This leaves a weakened area of the wall which is a potential site for herniation to occur. This type of hernia accounts for approximately 10-15% of all abdominal hernias. • Umbilical: This is a protrusion at the belly button which is regularly seen from birth. Over time these usually dry up and disappear altogether. It is possible to get these hernias as an adult too, usually as a result of being overweight or pregnant. • Epigastric: There is a tough, fibrous piece of tissue that spans from the tip of the rib cage to the pelvis in the mid-line of the body known as the ‘Linea Alba’. This forms an area of muscular attachment of the abdominal muscles. Due to a weakness in the abdominal wall above the belly button, a hernia can occur. This is common in infants, but again may happen later in life. Groin location • Inguinal: This is the most common type of abdominal hernia accounting for approximately 75% of all cases. The opening for this hernia is a region known as the ‘inguinal canal’ which allows for the testicles and spermatic cord to descend into the scrotum during male development. After this event, the canal should tighten, but in some males the muscles responsible for this do not respond as well as expected, leaving an area of weakness. As females do not forego this part of development, it rarely affects women. • Femoral: There is a space in the floor of the abdomen for a vein and artery to pass through and down into the leg, known as the femoral canal. In females this canal is wider which results in this type of hernia being more common in women than men. It accounts for approximately 10-15% of all abdominal hernias. Treatment Treatment of abdominal hernias depends on the severity and symptoms associated with them. Sometimes with a hernia, the abdominal contents inside them can become trapped and ‘strangled’, ’which can lead to loss of blood supply and ultimately death of tissue. These complications can possibly be fatal if left untreated. In these cases, and with most uncomplicated cases, surgery is the best course of action to ensure a full recovery. There is also a place for physical therapies like physiotherapy. Physio is particularly helpful following a surgical procedure to aid with strengthening of the abdominal muscles and surrounding area, supporting the area and reducing the risk of re-herniation. Scar tissue following surgery can affect our ability to move efficiently, however exercise as well as hands-on therapy can help to reduce the effect of this. If you have an abdominal hernia and would like advice on how to manage it, please get in touch today by going to our online booking website https://www.myhealth1st.com.au/find/physiotherapists/nsw/nsw-region/north-sydney/back-in-business-physiotherapy or by calling us on 02 9922 6806 to book a face-to-face or Tele Health appointment. If you require the opinion of a doctor or specialist, we'll ensure you are placed in the best possible hands. References 1. MSD Manual. 2020. Hernias of the Abdominal Wall. [Online]. Available from: https://www.msdmanuals.com/en-au/professional/gastrointestinal-disorders/acute-abdomen-and-surgical-gastroenterology/hernias-of-the-abdominal-wall. [Accessed 08 April 2020]2. Melbourne Hernia Clinic. 2018. What is a Hernia? [Online]. Available from: http://hernia.net.au/what-is-a-hernia/. [Accessed 08 April 2020]3. MedicineNet. 2020. Hernia (Abdominal Hernia) 9 Types, Symptoms, Causes and Surgery. [Online]. Available from: https://www.medicinenet.com/hernia_overview/article.htm. [Accessed 08 April 2020]4. Healthline. 2019. Everything You Want to Know About a Hernia. [Online]. Available from: https://www.healthline.com/health/hernia. [Accessed 08 April 2020] Uploaded : 28 April 2020 Read More -

Connective Tissue Disease
Connective tissue disease Hello readers and welcome to our next blog instalment. This month it’s Connective Tissue (CT) Disease. There are many different CT disorders, with too many to cover in one blog, so we’ve written a bit of an overview so you can learn the basics. The big question we hear you ask is “What is connective tissue?”. Connective tissue is the stuff in our bodies that holds all of our cells together. It's a bit like glue. It has a special role, allowing our skin and other tissues to stretch and then return back to their original state. You can kind of think of it like an elastic band that stretches and recoils over and over. Connective tissue is made of protein, and the main examples in the body include collagen and elastin. Connective tissue disease can pretty much affect any part of our body. Our bodies are made up of trillions of cells (approximately 37.2 trillion!) which all require some form of glue to ensure we are held together in our human form. There are diseases that affect our skin, muscles and tendons, ligaments, bones and cartilage, blood and blood vessels, eyes and more! Types of disease To make things a little easier to get your head around, we can break CT diseases into two categories: • Inherited diseases: These are diseases passed down to us in our genetic make-up. Most of these diseases occur due to a mutation of a single gene.• Autoimmune diseases: These are diseases where our bodies create antibodies that fight against our own tissues. In this case, it’s the connective tissues that our body is fighting against. Inherited diseases Here’s a brief overview of a few inherited CT diseases: • Ehlers-Danlos Syndrome (EDS): A group of 13 differing conditions that affect collagen in the body. Common symptoms include very mobile joints and excessively stretchy and fragile skin. People may also experience heart and lung problems as well as weakened blood vessels. https://www.back-in-business-physiotherapy.com/we-treat/ehlers-danlos-syndrome.html • Marfan Syndrome: A condition that affects the production of the protein Fibrillin-1 in the body. Symptoms are widespread, affecting the blood vessels, heart, bones, joints and eyes. Marfan Syndrome affects approximately 1 in every 5000 people. • Osteogenesis Imperfecta: Also known as 'Brittle Bone' disease. This is a condition that affects collagen (specifically Type I) and leaves bone more fragile and prone to fracture. Other signs and symptoms include a blue tinge to the whites of the eyes, hearing loss and weak joints and teeth. Autoimmune diseases Here’s a brief overview of some autoimmune CT diseases: • Rheumatoid Arthritis (RA): This is not to be confused with the more common Osteoarthritis (OA). RA is a condition typically associated with inflammation of the small joints of the body, like those found in the hands, feet and wrists. Joints become hot, red, swollen, painful and stiff as the body fights against the tissues that line and surround the joints. Over time, the joints go through degenerative change and may appear deformed. This condition may also cause inflammation around the lungs and heart, as well as affecting many other systems of the body. • Systemic Lupus Erythematosus (SLE): A condition that causes inflammation of the skin, joints and various organs of the body. Symptoms are widespread and include a butterfly shaped rash on the face and nose, light sensitivity, mouth ulcers, kidney disease and mental illness including memory loss. • Scleroderma: A group of conditions that lead to the thickening and scarring of the skin, organs and blood vessels. People may also experience Raynaud’s Phenomenon; a condition where the blood vessels in the fingers and toes go into spasm resulting in a lack of blood flow to the area. This will look like areas of white and blue over the skin with numbness being another symptom. It is not uncommon for people with one autoimmune CT disease to show signs and symptoms of other autoimmune diseases too. In these instances, a person is referred to as having Mixed Connective Tissue Disease (MCTD). Many people with these overlapping conditions go on to receive a firm diagnosis of SLE or Scleroderma later in life. We hope you found this blog a helpful tool for learning about CT diseases. If you have a CT disease or want to know more information on a particular condition, feel free to ask us next time you are in the clinic or through Tele Health. Have a great month and stay safe everyone. https://www.myhealth1st.com.au/find/physiotherapists/nsw/nsw-region/north-sydney/back-in-business-physiotherapy References: 1. Healthline. 2018. Diseases of Connective Tissue, from Genetic to Autoimmune. [Online]. Available from: https://www.healthline.com/health/connective-tissue-disease. [Accessed 08 April 2020]2. National Geographic. 2013. How Many Cells are in Your Body? [Online]. Available from: https://www.nationalgeographic.com/science/phenomena/2013/10/23/how-many-cells-are-in-your-body/. [Accessed 08 April 2020]3. Arthritis Foundation. 2020. Mixed Connective Tissue Disease. [Online]. Available from: https://www.arthritis.org/diseases/mixed-connective-tissue-disease. [Accessed 08 April 2020] Uploaded : 28 April 2020 Read More -

Physiotherapy, Exercise, Chaos and the Immune System (during COVID-19)
Deterministic Chaos Theory, Exercise, Physiotherapy Reasoning and the Immune System (during COVID-19) by Martin Krause B.Appl.Sci. (Physiotherapy); M.Appl.Sci (Manipulative Physiotherapy), Post Grad Dip Hlth Sc (Exercise and Sports), Post Grad Cert Hlth Sc (Education) Known Knowns, Known Unknowns, Unknown Unknowns - the latter is what we need to recognise Since the onset of COVID-19 many of us have asked why are there so few antivirals? The answer boils down to biology, and specifically the fact viruses use our own cells to multiply. This makes it hard to kill viruses without killing our own cells in the process. So how do we ensure cell survival, whilst priming the immune system to make antigens for its defence system. What does this even mean? Can exercise be an answer to reduce the extent of our immune response if exposed to COVID-19? Will knowing why exercise is good for our immune system motivate people to exercise more? During this time of crisis, we've been told to exercise. Exercise for physical and mental well-being. Whether in partial 'lock down' or 'full lock down' or 'opening up', exercise is still important. But Why? How do chaos theory and non-linear dynamics explain movement and the immune system? The following represents a synopsis of my past research in the field of biomechanics, pathomechanics, neurophysiology, cognition, immunology, sarcopenia and my current interest in chaos. The slides are from a Keynote presentation I made in Rome in 2005. We were born from the chaotic fire of genesis. Laws of thermodynamics dictate our existence. Evolution of heat shock proteins (HSP) means that we are our immune system. Today, human multi-cellular life is still totally dependent on our unicellular ancestors and their componentry. Trillions of species and bacteria in the gut (flora) and skin alone, associated with immune substances, attest to the importance of unicellular life in the immune system. The abundance of energy species in the gut suggests a nexus with one of the organs most in need of energy, the skeletal muscle. Importantly, muscle cells have more mitochondria than most other cells, so they can readily produce work for movement. Consequently, muscles are an energy system and an immune endocrine organ. Notably, the development from unicellular to multi-cellular life needed movement. A commonality of cellular movement and macro-muscular movements exist. Physiotherapeutic and training interventions must consider the health of the immune system and its ability to deploy and be re-deployed. Training should avoid becoming 'stale' by having enough variety (chaos) to create perturbations in the immune system which induce up and down regulation of immune componentry. Physiotherapy should be innovative and creative, whereby the physiotherapist additionally considers immune-cognitive aspects of pain and inflammation, when people seek physiotherapeutic intervention after/during a change in their training regime and/or commencement of unaccustomed exercise, or in the presence of immune compromise. Index 1. What is a stressor? 2. COVID-19 3. General Adaptation Theory 4. Nasal Heat Shock Proteins 5. Heat Shock Proteins (HSP) pictures 6. Damping Ratios 7. Sympathetic N.S. & Chaos 8. Butterfly Effect & Chaos 9. Chaos theory and Physiology 10.COVID-19 Clinical Presentation 11.Infection & HSP 12.HSP70 viral response (1) 13.Muscle-Immune response 14.Matzinger's Danger Hypothesis 15.Classes of HSP 16.HSP72 and HSP27 and muscle 17.Extracellular HSP 18.Aging, HSP and CK 19.Age, COVID-19 & thrombocytes 20.COVID-19 and Platelets 21.Pulmonary emboli 22.Exercise & Respiratory Tract 23.Exercise and Resp Tract Infections 24.HSP viral response (2) 25.HSP-90 26.Mechano-transduction & heat 27.Actin-Myosin Cross Bridge 28.Entropy 29.Bicycle Cadence and Entropy 30.Eccentric Contractions 31.Eccentric Exercise & Immune Markers 32.Sarcopenia 33.Muscle Glutamine 34.Muscle Immune Conversion 35.Over-training 36.Chaos Theory 37.Deterministic Chaos & Immune System 38.Maths & Deterministic Chaos 39.Uncontrolled Manifold Hypothesis 40.Game Theory 41.Cortical Resources 42.Exercise induced disease 43.Anti-Carcinogenic Effect of Exercise 44.Allostasis 45.Neural Componentry & Chaos 46.COVID-19 and Allostasis 47.Recovery & Sleep 48.Psychology & Immunity 49.Diet 50.Gut-Muscle Immune axis 51.COVID-19, gut and lungs 52.Dosage of Exercise 53.Motivators to Exercise and to eat 54.Leptin, Diabetes and X's 55.Leptin and Diet 56.Exposure 57.Musculoskeletal Physiotherapy 58 Low Back Pain and Entropy 59.Conclusion 60.Justification 61.Links COVID-19 vaccinations and musculoskeletal side effects - 8 August 2021 Last week, two separate clients presented with an exacerbation of injuries which I had treated previously. One was a 57 year old lady, who I had successfully treated for low back pain and nerve inflammation, a year previously. Three days after the Pfizer vaccine, she felt 'like a horse had kicked her in her back'. Luckily, her symptoms resolved after a few days. Another client, a 21 year old female, presented with severe ankle and foot pain. Similarly, three days after a Pfizer vaccination. I had treated her for a 'strange presentation' of calf and ankle swelling three years previously, for which multiple investigations found no explanation. Some form of vascular condition was suspected in the previuos presentation. This time around, her symptoms resolved within a week, however, her presenting symptoms were similar to someone with Complex Regional Pain Syndrome (CRPS) or an auto-immune disorder of the ankle and foot! Oscillatory systems Many of the things an Australian trained Musculoskeletal Physiotherapist does has to do with oscillations. Everything from joint oscillations, therapeutic ultra-sound, to repetition in exercise to Whole Body Vibration (WBV) therapy involves an obvious form of oscillation. Other less obvious forms of oscillations occur within muscles, within whole body immune systems and across body musculoskeletal systems. The following argues that the expression of oscillations can determine the health and well being of a person beyond simplistic notions of biomechanics, pathology and repair. What is a 'stressor' and why is muscle considered an endocrine immune organ? The sympathetic nervous system has traditionally been assigned the responsibility for the 'freeze, fight or flight' stress response. Regardless of mechanism, the call to action goes to muscles. Culturally, we generally consider a muscular person as the 'picture of health'. Yet, what resides and moves within muscle is as important as the work those muscles produce. When we exercise, the body adapts to a stressor, which is calorific, metabolic, physiological, immune and psychological. Phylogenetically, heat shock proteins (HSP) evolved from uni-cellular to multi-cellular life, and 'exercise' (physical activity) was associated with survival skills, such as food acquisition and defence (self-preservation). Interestingly, those same mechanisms can be 'fine tuned' to improve the age of your immune system. If we can get or maintain muscle bulk, we can maintain a reservoir of protein for immune function. If we can maintain adaptive processes to mechanical trauma and inflammation, we have a fighting chance of using similar processes to launch an appropriate immune response, fight infection, prevent cell death (apoptosis) and muscle-organ failure (cachexia). What is the mechanism behind an 'appropriate' immune response? What sets the system in motion (perturbation) and what 'dampens' it? How do the laws of thermodynamics and conservation of energy apply? What is the predicted 'chaos' in the system and how do the immune and sympathetic nervous system act as oscillating 'manifold' for chaos to 'unfold' and 'refold'? COVID-19 In March 2020, of those patients who test positive for COVID-19, approximately 14% develop severe disease requiring hospitalisation and oxygen support and 5% require admission to an intensive care unit. 10% to 20% of severe patients develop acute respiratory distress syndrome (ARDS) during 8–14 days of the illness with complications including sepsis and septic shock, multiorgan failure, including acute kidney injury and cardiac injury (Yang et al, 2020). Older age and co-morbid disease (cardiovascular disease, diabetes, chronic respiratory disease, hypertension, cancer) are associated with higher mortality rates during COVID-19 infection. There is low quality evidence to suggest exercise has no impact on the rate and duration of acute respiratory infection but may provide a small reduction in severity of symptoms. Increasingly evident, COVID-19 appears to be a disease of the vasculature, especially in the young, where thrombus formation, multi-organ inflammation and cytokine storms are evident. By October 2020, therapeutics directed at multiple organs and using anti-viral, symptom moderation medication, as well as anti-body experimental treatments have been used to improve survival rates, by reducing the severity of the disease. At this point in time, a vaccine for the spike protein is non-existent. Research in exercise immunology suggests moderate exertion may decrease the risk of acute respiratory infection in healthy adults but lacks assessment of its reliability (https://www.cebm.net/covid-19/does-physical-exercise-prevent-or-treat-acute-respiratory-infection-ari/). However, we do know that regular exercise attenuates the afore-mentioned co-morbidity. Additionally, low evidence means we should pursue the (construct validity) evidence if 'face validity' is evident. The following describes muscle as an immune organ, exercise as an 'adaptor' of that organ, based on immunological principles (from non-linear and linear mechanics) such as heat shock proteins (HSP), cytokines and platelets, importance of 'outliers' based on 'deterministic chaos' as associated with exercise, the sympathetic nervous system, as well as the gut-muscle axis associated with 'energy species'. Stress and the General Adaptation Syndrome The general adaptation syndrome (GAS) model of stress posits three stages to stress: alarm, resistance and exhaustion. In the alarm stage, the nervous system releases stress hormones to facilitate a freeze-fight-flight response. When a stressor is ongoing, like the COVID-19 pandemic, returning to homeostasis is more difficult. In the second stage — resistance — the individual’s allostatic load ideally returns to baseline. But many people will not, especially in the prolonged stress of a pandemic. Physicians should consider that patients reporting symptom exacerbations (of pre-existing issues), during this time, may benefit from stress mitigation techniques, including: Diaphragmatic breathing Guided imagery Mindfulness Limiting media exposure Progressive muscle relaxation Physical activity These techniques may include holistic approaches such as Yoga, Progressive Resistance Exercise (PRE), and endurance training. In the third stage, called exhaustion, people become overwhelmed from the ongoing stressor. This is where prolonged dysfunction can occur, and in which identifying a coping strategy becomes more difficult for the person. One would hope that intervention occurs during the second stage, when acceptance of behavioural modification is more likely. Furthermore, it is hoped that the general population remains active for life, even in the post COVID-19 era. The following is an overview of why exercise is so important, for the immune system, by using a 'deterministic chaos' theoretical approach to protect against chaos. Nasal Heat Shock Proteins Heat Shock Proteins (HSP) are found in virtually all living organisms, from bacteria to humans. They are a class of proteins which react both to heat, cold and oxidative stress. Since unicellular life, these small protein chains, have developed with evolution, and despite the complexity of multi-cellular life, they still have an important fundamental role to play in human survival. Incredibly, this, evolution, means that complex multi-cellular life, can still recognise their unicellular ancestor counterparts! Frequent confrontation of the host (human) immune system, with conserved regions of HSP, which are also shared by various microbial pathogens, can potentiate antimicrobial immunity. However, long-term confrontation of the immune system with HSP antigens, which are similar in the host and invaders, may convert the immune response against these host antigens and promote autoimmune disease. Since COVID-19 is thought to have an 'auto-immune' mechanism and has a profound impact on the airways, in symptomatic individuals, the following is an example of nasal mucosa HSP responding to heat stress. Nasal HSP's 1 hour after heat shock stimuli (Min et al 2020 International journal of medical sciences 17(5):640-646) Heat Shock Protein - what they look like Small HSP (mycobacterium) by Kim, K.K., Kim, R., Kim, S.H.(1998) Nature 394: 595-599 PubMed: 9707123 DOI: 10.1038/29106 HSP 27 by Michael H. Chiu, Chunhua Shi, Matthew Rosin, Zarah Batulan, Edward R. O’Brien (2019) HSP 72 by Osipiuk, J., Gu, M., Mihelic, M., Orton, K., Morimoto, R.I., Joachimiak, A., Midwest Center for Structural Genomics (MCSG) 2010 Damping ratio To understand energy systems we must also understand 'oscillation control' by examining 'simple harmonic motion' (SHM) in terms of linear dynamics (kinetic and potential energy ) of a mass spring and it's 'damping ratio'. Simply stated, if you hang a mass off a spring and pull down on it and let it go, in the absence of plastic deformation, the mass will 'overshoot' back and forth several times before resuming its original position. That is, it experiences a restoring force proportional to its displacement. Depending on the weight of the mass and the thickness of the spring, the non-optimised system may experience overdamping or underdamping (Wikipedia). A lower damping ratio implies a lower decay rate, and so very underdamped systems oscillate for long times. Importantly, this model applies to energy systems and hence obeys the law of thermodynamics. Traditionally, health was considered in terms of predictability. Consistent heart rate was considered good, irregular heart rate as bad. Unfortunately, it isn't quite so simple. In fact in terms of training concepts, low resting heart rate and how quickly the heart rate can oscillate with demand is used to diagnose if an athlete has become 'stale' or said in another way is in a state of 'over-training' or enhance physiological and/or psychological stress. Hence, in the light of these confounding 'beliefs', a more complex system (model) needs to be employed, involving random perturbations of an oscillatory system, if random 'outliers' are to be incorporated into our understanding of health. Simplistic versions of sympathetic vs parasympathetic tone balancing the autonomic nervous system do not explain complexity. It is difficult to reconcile that the parasympathetic vagus nerve controls all thoracic and abdominal organ function and alone counters all 'chaos' of sympathetic nervous system activity, where the latter activity has a multitude of redundancy and interacts in multiple dimensions with an interlaced muscle-gut immune system complex. The sympathetic nervous system is the tight rope, the trapeze artist, the dancer, the orchestra, forged from the fire of genesis and the evolution of heat shock proteins. To understand the development of the muscle-gut immune system complex we must understand its uni-cellular componentry. Using Alexandr Lyapunov theory of stability, in non-linear dynamic systems, the oscillations near the point of origin (equilibrium) are determined by exponential decay. That is, if the solutions that start out near an equilibrium point Xe, stay near Xe forever, then Xe is Lyapunov stable. More strongly, if Xe is Lyapunov stable and all solutions that start out near Xe converge to Xe, then Xe is asymptotically stable (As an illustration, suppose that we are interested in the properties of a function f(n) as n becomes very large. If f(n) = n2 + 3n, then as n increases, the term 3n becomes insignificant compared to n2. The function f(n) is said to be "asymptotically equivalent to n2, as n → ∞". This is often written symbolically as f(n) ~ n2, which is read as "f(n) is asymptotic to n2 "). The notion of exponential stability guarantees a minimal rate of decay, i.e., an estimate of how quickly the solutions converge. The idea of Lyapunov stability can be extended to infinite-dimensional manifolds (chaos theory), where it is known as structural stability (in mathematics, this is a fundamental property of a dynamical system which means that the qualitative behaviour of the trajectories is unaffected by small perturbations), which, in this case concerns the behaviour of different but "nearby" solutions to differential equations. Later, this will be applied, not only to EMG analysis of muscle activity, but also to cytokine interactions, from nearby solutions Sympathetic Nervous System and Deterministic Chaos The sympathetic nervous system (SNS) has, as previously stated, traditionally been associated with the freeze-fight-flight response - you fight the lion or run from the lion. A reaction to a 'danger signal' (Matzinger). However, there is a lot more to it. Never-the-less, this example describes a bi-directional nervous system, one which is driven by 'motor curiosity' and wanting to arouse sensory stimuli, whilst the other is reacting to 'sensory stimuli'. Frequently, these moments are described as an 'adrenalin rush' associated with fear, excitement and tremor. The greater the chaos and tremor in the system, the greater the perturbations and the greater the damping needed in the system. Ideally, what drives the system also dampens it. Otherwise, at 'extremely high frequencies' we would only 'freeze'. Clinically, some people believe, that right hemisphere dominant tremor tend to have a higher component of irrationality and hypervigilance, whereas left hemisphere dominant tremor may have a more rational generator of tremor. However, this simplification ignores cross-hemispheric communication systems. It is important to note that in health systems, it's the odd asynchronicity in the system which attests to it's health. That is the chaos, 'outlier', in the system. This control by chaos is relative, it's a ratio, it's a magnification, it defines itself and it 'dampens' itself. Furthermore, the outliers define what it isn't! Hence, 'deterministic chaos'. When looking at 'fractals', you can have an infinite length in a finite space. Bifurcation upon bifurcations, getting smaller and smaller ad-infinitum but within a finite space! For example, the length of the coastline of the United Kingdom is known to an error margin of + 10-20% depending on how closely one looks at it (ie at what magnification ratio or scale). As we examine the movement system, we frequently see tremor at each end of the spectrum. With fine delicate movements and with movements which require a lot of force we see a tremor. In scenarios of many repetitions and fatigued muscles, they gradually cramp up and lose their oscillatory fidelity. This can be considered as an energy or metabolic constraint. In novel tasks, we see more rigidity in movements, due to increased muscular activity, resulting in reduced freedom of movement. In the latter scenario, cognitive constraints arise at a conscious and sub-conscious level, where learning becomes important to improve the degrees of freedom, reduce the amount of muscle tension and hence lower the rigidity in the system. Are degrees of freedom, and hence variability, important for the immune system? A system dependent upon ratios of heat shock proteins, pro and anti inflammatory cytokines, immuno-globulins, lymphocytes, neuropeptides, short fatty acid chains, metabolism, descending noradrenergic and serotonergic pathways and even a balance between 'innate' and learned 'adaptive' immune responses, occurring within and acting upon, the largest endocrine organ of the immune system, skeletal muscle. Is it a coincidence that the spinal cord looks like a butterfly? Butterfly effect and chaos theory - from Wikipedia In chaos theory, the butterfly effect is the sensitive dependence on initial conditions in which a small change in one state of a deterministic nonlinear system can result in large differences in a later state. The term, closely associated with the work of Edward Lorenz, is derived from the metaphorical example of the details of a tornado (the exact time of formation, the exact path taken) being influenced by minor perturbations such as the flapping of the wings of a distant butterfly several weeks earlier. Lorenz discovered the effect when he observed that runs of his weather model with initial condition data that was rounded in a seemingly inconsequential manner would fail to reproduce the results of runs with the unrounded initial condition data. A very small change in initial conditions had created a significantly different outcome. The idea that small causes may have large effects in general, and in weather specifically, was earlier recognized by French mathematician and engineer Henri Poincaré and American mathematician and philosopher Norbert Wiener. Edward Lorenz's work placed the concept of instability of the Earth's atmosphere onto a quantitative base and linked the concept of instability to the properties of large classes of dynamic systems which are undergoing nonlinear dynamics and deterministic chaos. Chaos theory and physiology What happens if the 'flapping wings of the butterfly' dampen or calm 'the tornado on the other side of the planet'? In terms of the human organism, chaos theory refers to 'deterministic chaos'. This means that if one knows the initial conditions (state) of the system exactly, then the dynamical trajectory will be the same every time it is initiated in that condition (state). If, however, two states are 'infinitesimally' apart, then the trajectories are such that it makes it impossible to predict the future dynamics (chaos). Oscillatory dynamics is the prerequisite for many complex phenomena and the onset of chaotic dynamics. Chaos refers to complex, apparently unpredictable, dynamics that even simple deterministic dynamical systems can produce. A universal way to achieve chaos is by driving a nonlinear oscillator by an external periodic signal. When the external driving signal has low amplitude oscillations, it can entrain or synchronise the nonlinear oscillator. As the amplitude of oscillations is increased, the range of frequencies for which it can entrain becomes larger—these expanding synchronisation regions of the external amplitude–frequency parameter space are called Arnold tongues. Such entrainment/synchronisation has been observed in many different physical systems, from fluids to quantum mechanical devices, and now also in biological processes, such as cell cycles, and gene (transcription) regulatory dynamics in synthetic populations. The dynamics gets even more complex as the amplitude of the external driving signal increases further. First, Arnold tongues start overlapping, which means the nonlinear oscillator can exist in more than one entrained state with different frequencies (termed modes), and even small amounts of intrinsic or extrinsic noise can cause it to hop between these modes. Such mode-hopping has been observed in immune system (p53 tumour suppressor) and in gene transcription of the oscillatory NF-κB system, when driven by a periodically varying Tumour Necrosis Factor (TNF) signal of sufficiently high amplitude. When the external amplitude is increased even further, then chaotic dynamics is predicted (Heltberg et al 2019 Nat Commun 10, 71 https://www.nature.com/articles/s41467-018-07932-1.pdf) Shareable link https://rdcu.be/b4sU7 Nat Commun 10, 71 (2019). The significance of this is, that NF-κB is a major transcription factor which regulates genes responsible for both the innate and adaptive immune response. Upon activation of either the T- or B-cell receptor, NF-κB becomes activated through distinct signalling components. TNF is a major inflammatory cytokine player, found in skeletal muscle (MSK), produced by macrophages/monocytes during acute inflammation and is responsible for a diverse range of signalling events within cells, leading to necrosis or apoptosis. The protein is also important for resistance to infection and cancers. Furthermore, other immune ratios or interactions, based on maths and physics, are predicted, which will hopefully lead to a better understanding of why physiotherapists should encourage people to exercise muscle as a vaccine for the immune system. This discussion will include interactions between Interleukin IL-6 (pro inflammatory) driving IL-10 (anti-inflammatory) t-cell CD4+ : CD8+ ratio, HSP 27 and HSP72 HSP 10 and HSP 60 HSP 60 and HSP 70 HSP 90 as well as examining the gut biome and muscle - brain axis in terms of energy, resources and game theory. COVID-19 Clinical Discussion: 1 May 2020 The following is an abstract from an online clinical forum. It serves here to illustrate the terms used in the discussion, including 'cytokine storm' (inflammatory substances), 'viral burden', 'anticoagulants' (clot busters) and 'immunosenescence' (immune dysfunction/compromise) which have been pervading posts to this forum, about COVID-19. Bear these terms in mind for later discussion. Hence, as stated, the following dissertation will consider cytokines (inflammatory substances), platelets and HSP in relation to muscle as an endocrine organ of the immune system and examine the link with the gut biome, and in particular, the energy species within the gut, as it relates to the immune system, but also as those energy species relate to movement adaptation, within the musculoskeletal system. "We are what we eat" and "healthy mind healthy body" are common sayings which will become abundantly clearer when examining the gut-brain-muscle axis. Chaos theory as it relates to ratios, synchronous to asynchronous periodicities, and magnification of movement and inflammatory markers in response to variable 'healthy' physical demands are postulated to act as a 'muscle - immune shock absorber' when confronted by pathogens. Infection - a bimodal HSP reaction of host and pathogen When entering the host from the environment, a microbial pathogen is confronted by several changes, some of which are highly stressful. These include alterations in temperature, pH, and pO2. Moreover, the pathogen is exposed to natural host resistance mechanisms such as phagocytosis by professional phagocytes. Once engulfed by phagocytes, the pathogen is confronted with reactive oxygen and nitrogen intermediates, attack by lysosomal enzymes, and depletion of Fe2+. To protect itself against the host, the pathogen activates various evasion mechanisms including its own HSP synthesis. Infection is therefore a bimodal process determined by the host and pathogen. During infection, the pathogen as well as the host increase their HSP production. Induction of host HSP synthesis in response to an encounter with a pathogen has at least two major causes. First, infected macrophages are confronted with antimicrobial mechanisms which they have activated themselves during infection. Efficient protection against their own effector molecules (e.g., reactive radicals) becomes vital for macrophage survival. Second, once inside a phagocyte, many microbes, especially those which persist in the host, interfere with intracellular host cell metabolism. Not surprisingly, many of these pathogens are potent inducers of HSP synthesis in mammalian cells (see Ulrich Zügel, Stefan H. E. Kaufmann (2019) https://cmr.asm.org/content/12/1/19 DOI: 10.1128/CMR.12.1.19). They say, 'in life we never should forget where we came from'. This appears true for HSP, where the HSP of a multicellular host recognises and react to the HSP of unicellular pathogens. A reflection on the evolution of life on earth. Heat Shock Protein (HSP) 70 and the viral response Virus infections induce heat shock proteins (described in detail below) that in turn enhance virus gene expression. An intriguing concept is that HSP within pathogens activate HSP within the host. This phenomenon is particularly well characterized for 70 kDa heat shock protein (HSP70). However, HSP70 is also readily induced by fever, a phylogenetically conserved response to microbial infections. When released from cells, HSP70 can stimulate innate immune responses through toll like receptors 2 and 4 (TLR2 and 4). In their review, researchers (Mi Young Kim and Michael Oglesbee 2012 Cells. 2012, 1, 3,: 646–666. doi: 10.3390/cells1030646) examined how the virus-HSP70 relationship can lead to host protective innate antiviral immunity, and the importance of HSP70 dependent stimulation of virus gene expression in this host response. Beginning with the well-characterized measles virus-HSP70 relationship and the mouse model of neuronal infection in brain, they examine data indicating that the innate immune response is not driven by intracellular sensors of pathogen associated molecular patterns, but rather by extracellular ligands signalling through TLR2 and 4. Specifically, Kim & Oglesbee (2012) addressed the relationship between virus gene expression, extracellular release of HSP70 (as a damage associated molecular pattern), and HSP70-mediated induction of antigen presentation and type 1 interferons in uninfected macrophages as a novel axis of antiviral immunity. The reported antigen presentation and cross-presentation and in vitro HSP cytokine functions are a result of molecules bound to, or chaperoned by, HSPs but not a result of HSPs themselves (Tsan MF1, Gao B.2009 J Leukoc Biol.85, 6 :905-10. doi: 10.1189/jlb.0109005). Notably, intra- (IC) and extracellular (EC) HSP 72 are thought to have different functions. IC HSP 72 confers cellular protection from subsequent stressors, while EC HSP 72 has a whole-body systemic role in antigen presentation and immunity. An acute exercise bout stimulates an increase in both IC and EC HSP 72. Long-term training and improved fitness increase the rate of availability of IC HSP 72 in response to stress. Other factors that affect HSP 72 production include environmental factors, exercise mode, duration and intensity, age, Estrogen, and anti-oxidant and glycogen availability. Additionally, other HSP such as HSP27 play a role in conserving HSP72 function. Importantly, the functions and roles of HSP 72 depend on the tissue of origin (brain, muscle, etc). Ratios of HSP's will be discussed later in the context of muscle-exercise-immune responses and is represented in the following schematic (bear in mind HSP70 are a class of HSP's which include HSP72) and ubiquitin is from another class of HSP which are very small (8.5kDa) and have been highly conserved throughout the evolution of life. Similarly, the gut biome will be discussed in terms of 'energy species' and a HSP 10 and HSP 60 synergistic function. Ratios of CD4+:CD8+ appear to be critical when discussing health and disease; as will the consideration of how an acute, but not chronic, pro-inflammatory cytokines (IL-6) stimulate anti-inflammatory cytokine (IL-10) response. Muscle-immune response So, what is the role of Heat Shock Protein (HSP) in the immune system? Simply stated, early in life, we have an innate immune system, the one we are born with. It acts to protect us. It's first exposure and reaction to exposure is in the birth canal, where the cervix lining acts to induce a protective mechanism to exposure of the world. Our first 'adaptive immune response'. Antibodies are formed from exposure to antigens. These antibodies are formed from RNA into DNA, by cleaving off small protein chains from long protein chains (telomeres). It's a bit like cutting a small piece of tail off the long protein chain. We do this throughout life, with the aid of HSP's. However, as you can imagine, those long protein chains eventually become shorter and are finite. Hence, it's important to maintain our protein reservoir in our bodies by finely tuning how much and when proteins are cleaved, unfolded and refolded or deemed as useless by HSP. Since muscle consists of 90% protein, it becomes abundantly clear that we should protect it's bulk and function by training it, when healthy, and using it's reservoir of protein immune components during or after a disease. The above schematic (Krause 2004) illustrates immune reactions occurring within muscles. Immune responses are a complex interaction of cytokine signalling. Cyto = cell, Kine = movement. These signalling reactions occur in the brain, gut, liver, kidneys, thymus and muscle, in response to a perceived-safety danger signal (Matzinger 1994, review by Martin Krause 2004). Fine tuning of the cytokine reaction is important through a direct muscle cytokine 'micro-trauma' mechanical mechanism and indirectly through 'energy cycling' including metabolic mechanisms, including oxidative stress (REDOX) induced HSP. Furthermore, a multitude of cognitive stimuli can also influence (positively and negatively) the immune system. Notable, HSP must respond to the laws of thermodynamics. In the context of COVID-19, it has become apparent that those critically ill patients, have cytokine flooding in their lungs. That is, they have an uncontrolled (auto) immune response which has been referred to as a 'cytokine storm'. Additionally, there also appears to be a delayed immune response in younger individuals relating to inflammation of blood vessels and clot formation. Further, extremely low oxygenation (<50%) has been reported suggesting hypoxic metabolic stress, potentially not to dissimilar to when we exercise, only in the later we can in most cases cease the exercise without undue effects. A notable exception is Rhabdomyolysis (which is a condition in which skeletal muscle tissue dies, from over-exertion or pathogens, releasing substances into the blood stream that cause kidney failure) discussed elsewhere on this site. It will be argued that previous 'fine tuning' of the cytokine response, through exercise induced neuro-immune perturbations, leaves the host, not necessarily less susceptible to infection, but more prepared to deal with heat stress, platelet reactions as well as the infection itself. Matzinger's Danger Hypothesis - from Wikipedia In 1994 a new immunologic model was suggested by Polly Matzinger. She suggested that the immune system does not distinguish between self and non-self, rather, it discriminates between dangerous and safe by recognition of pathogens or alarm signals from injured or stressed cells and tissues. According to this theory, the most important stimulation of immune response are normal tissues. When tissue cells are distressed because of injury, infection and so on, they start to secrete or express on their surface so called "Danger signals". "Danger signals" are also introduced into extracellular space when stressed cells die by immunologic not-silent cell death such as necrosis or pyroptosis (highly inflammatory form of cell death, as opposed to apoptosis, controlled cell death). This model also suggests that, despite their potential immunogenicity, neoplastic tumours do not induce significant immune responses to induce the destruction of the malignant cells. According to the danger model, the immune surveillance system fails to detect tumour antigens because transformed cells do not send any danger signals which could activate dendritic cells and initiate an immune response. "Danger signals" are normal intracellular molecules that are not found in the extracellular space under physiological conditions. The danger model has evolved over the years. "Danger signals" include DNA, RNA, heat shock proteins (HSPs), hyaluronic acid, serum amyloid A protein, ATP, uric acid and also cytokines like interferon-α, interleukin-1β, CD40L and so on. The "danger model" suggests that, upon cellular necrosis, cryptic molecules in normal cells might be liberated from the cytoplasm into the tissue microenvironment, new molecules might be expressed on the surface of killed cells, or new molecules might be synthesized by cells undergoing necrosis. In comparison, the damage associated molecular pattern "DAMP model" suggests that any non-functional molecules (regardless of their cellular location; extracellular or intracellular) that were denatured, oxidized, or had disintegrated quaternary structures might have unique biophysical patterns such as low water-solubility or stretches of polyanions on their surface. "Danger signals" and DAMPs are together with pathogen-associated molecular patterns (PAMPs) called alarmins and they are recognized by pattern recognition receptors (PRRs) of antigen presenting cells (APC). PRRs include Toll-like receptors (TLR), nucleotide oligomerization domain (NOD)-like receptors, retinoic acid inducible gene-I (RIG-I)-like receptors and C-type lectin-like receptors.[12] They are not only at the surface of these cells, but we can find them in cytoplasm and incorporated in the membrane of endolysosomes. Stimulation of PRRs leads to activation of APC cell to process antigen, upregulate expression of costimulatory molecules and present antigens to T helper cells. The danger model is a new perspective on adaptive and innate immunity. In the past innate immunity was suggested to be a minor part of the immune system — in contrast, adaptive immunity was thought to be the most important and effective part of the immune system. According to the danger model there is no adaptive immunity without the innate part. This is because APCs like dendritic cells are essential for activation of T lymphocytes and B lymphocytes, which after activation produce specific antibodies. In the case of dendritic cells deficiency, like in common variable immunodeficiency (CVID), patients suffer from hypogammaglobulinemia and from primary or secondary defects in T-cell functions. Häggström, Mikael (2014). "Medical gallery of Mikael Häggström 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436. Public Domain. or By Mikael Häggström, used with permission. - Image:Lymphocyte_activation.png, Public Domain, Link (Matzinger, P . "Tolerance, Danger, and the Extended Family". Annual Review of Immunology. 12 (1): 991–1045. doi:10.1146/annurev.iy.12.040194.005015. PMID 8011301. https://www.ohtn.on.ca/polly-matzinger-recaps-65-years-of-immunological-theory-in-one-diagram/ Classes of Heat Shock Proteins (HSP) Heat shock proteins (HSP) play an important role during exercise and subsequently induced immune responses (Krause 2002). Phylogenetically, HSPs are the basic building blocks of life. Small protein chains of around 8–43 kDa for HSP 27 class and 72kDa for HSP 72 ranging up to 110kDa. HSP72 is abundant in muscle. HSP 27 has been shown to be released in response to muscle damage during novel or acute eccentric (muscle lengthening) exercise, whereas HSP 72 is released in response to metabolic and thermal stress, during endurance exercise, in both untrained and well trained individuals. Additionally, HSP 27 is thought to aid in the repair process of HSP 72 as well as in the repair of contractile protein myofilaments themselves (Folkerson M 2018 http://oru.diva-portal.org/smash/get/diva2:1234179/FULLTEXT01.pdf). The relevance of the latter will become apparent when examining eccentric muscle contractions later in this treatise. HSP 60 is found abundantly in the gut and in the mitochondria of skeletal muscle, in rodents. It has been demonstrated, in rodents that HSP 60 is greater in slow twitch endurance muscle, as well as in the vastus lateralis of endurance trained men (reviewed by Mattias Folkesson 2018). HSP 60 and HSP 10 will be discussed later when considering the immune system, energy species and the gut biome. Hence, HSP's have an important cellular function, commonly referred to as a 'chaperone'. The fate of proteins with non‐functional conformations after stress exposure may be either to re‐obtain the functional conformation, form aggregations with other misfolded proteins or become degraded. HSP's play a helper role in shifting the equilibrium in the direction of more functional proteins or degradation of damaged proteins. This can occur in an ATP-dependent or independent manner, meaning the latter doesn't require the normal oxidative metabolism to function, as muscle contraction does. HSP had an important, stress induced, evolutionary and ecological role. As stated, it continues to play a vital role, as it's chaperone function acts to stabilise/modify exercise induced muscle damage, including micro-trauma. Additionally, HSP's play a role in apoptosis or cell death in sedentary individuals. Essentially they react to 'stressors' which can be temperature (hot and cold) and oxidative. Importantly, these ubiquitous molecular chaperones can prevent the irreversible aggregation of denaturing proteins. Specifically, to maintain protein homeostasis, HSP complex form a first line of defence against protein aggregation, with a variety of non-native proteins in an ATP-independent manner and in the context of the stress response. In vertebrates they act to maintain the clarity of the eye lens, and in humans HSP mutations are linked to myopathies and neuropathies (Haslbeck & Vierling 2015 J Mol Biol Apr 10; 427, 7: 1537–1548). Indirectly, HSP's act on the immune system by maintaining muscle bulk, which provides the environment in which cytokines can act and where proteins can be used to build antigens for an immune response. That is, reported antigen presentation and cross-presentation, activation of macrophages and lymphocytes, and activation and maturation of dendritic cells as well as in vitro HSP cytokine functions, are a result of molecules bound to or chaperoned by HSPs but not a result of HSPs themselves (Tsan MF & Gao B.J Leukoc Biol. 2009 Jun;85(6):905-10). Another, more intriguing speculation, is that the HSP of the pathogens themselves activate the innate human immune response in the presence of fever greater then 2-3 C (reviewed by Hasday JD & Signh IS 2000 Cell Stress Chaperones, 5, 5, 471–480). Regardless, an increase in core body temperature, during fever, activates and utilises elements of the heat shock response pathway, to modify cytokine and chemokine gene expression, cellular signalling and immune cell mobilisation, to sites of inflammation, infection and injury (Hasday JD & Signh IS 2013 Intl J Hyperthermia, 29, 5, 423-435). Hence, increases in temperature during exercise may be a mechanism which uses HSP's to preserve and improve muscle fibre protein, protecting it's bulk whilst adaptively fine tuning mechanistic pathways for potential innate HSP-cytokine immune responses. Muscle and Heat Shock Proteins (Krause 2005 Rome Presentation) Muscle is an incredible and potent reservoir of protein and immune substances. It is, in effect, one of the most important organs of the immune system. HSP are a multidimensional protein which act as a protein chaperone, an antioxidant and play a role in the inhibition of cell death (apoptosis). They act on muscle protein (actin cytoskeletal) remodelling. In particular, HSP27 has been characterized with the ability to regulate actin cytoskeletal dynamics during heat shock and other stress conditions, functioning both to promote actin polymerization and as an actin capping protein. During, intense exhaustive exercise, in hot conditions, both HSP72 and HSP27 are released into the blood stream (Periard et al, 2012, Cell Stress Chaperones, 17, 3, 375-378). HSP 27 is speculated to also have a HSP 72 preserving function. Presumably, these HSP, together, have HSP and cytokine protective roles, at certain stages in the immune-inflammatory cycle. Extracellular HSP 27 and HSP 72 during exercise Extracellular HSP expression has been demonstrated during exercise. The first investigation was in humans and treadmill running (60%VO2max) under hot conditions, where increases of eHSP 72 were found (Walsh RC, et al 2001. Cell Stress Chaperones, 6, 4,386-93). Further investigations (Periard JD et al 2012. Cell Stress Chaperones, 17, 3, 375–383), using cycling and heat at 60% and 75% intensity (HR 97% of max at termination) demonstrated core temperature reaching 39.7°C in the 60% trial (58.9 min) and 39.0°C in the 75% trial (27.2 min) (P < 0.001). The rate of rise in core temperature was 2.1°C at the 27.2 min mark and was greater in the 75% trial than in the 60% trial (P < 0.001). A significant increase and correlation were observed between eHsp72 and eHsp27 concentrations at exhaustion (P < 0.005). eHsp72 was highly correlated with the core temperature (heat storage) attained (60% trial) and the rate of increase in core temperature (75% trial; P < 0.05). Therefore, in response to an acute physiological challenge under heat stress, intensity and duration can result in similar changes to core temperature. Interestingly, if these high core temperatures presented clinically, the person would be considered febrile. Fever is used as a diagnostic criterion in clinical settings, with temperature elevations as low as 39 °C being a potent inducer of HSP 70 in the human brain (Morrison-Bogorad M.et al, 1995 J. Neurochem. 64, 235–246. doi: 10.1046/j.1471-4159.1995.64010235.x). For example. a fever is a consistent sequel to measles virus (MeV) infection (Hutchins SS et al, 2004. J. Infect. Dis.189:S153–S159. doi: 10.1086/379652) where heat and/or virus-induced inflammatory cytokines may represent a means of indirect HSP70 induction. The latter is supported by findings in canine distemper virus infected dog brains, where HSP70 induction was observed in viral antigen negative as well as viral antigen positive astrocytes, these being restricted to areas of active viral replication and inflammation (Oglesbee M & Krakowka S 1993 Lab. Invest.68, 109–117). . These are strange lines of best fit (correlation HSP 72 vs HSP 27), especially from baseline (60% vs 75% VO2 max), through to recovery 24 hours, after exhaustive exercise. Let's keep this in mind when discussing 'outliers' in chaos later in this dissertation. It should be noted that these extracellular HSP's are thought not to be from contracting muscle (Febbraio et al. 2002a), but rather as a result of the brain and hepatosplanchnic tissues which are capable of releasing HSP 72 in the systemic circulation (Febbraio et al. 2002b; Lancaster et al. 2004). Importantly. its extracellular expression (eHSP 72), measured in plasma and serum, has been suggested as a potential signal, triggering innate immunity and stimulating the release of proinflammatory cytokines (Pockley et al. 1998; Asea et al. 2000; Njemini et al. 2003; Pockley et al. 2003; Njemini et al. 2004; Asea 2005; Noble et al. 2008). In humans, they believe that the contracting muscles are not the source of eHSP 72. In : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3312965/#CR44 . However, contrary to this belief on extracellular HSP, it will later be argued, that contracting muscles release localised HSP, during concentric (cycling) and eccentric (running and plyometrics) exercise, where the laws of thermodynamics and concepts of myofilament micro-trauma (respectively) are applied......and that although these intracellular HSP have a different function to eHSP, their relationship is 'continuous' In the 75% trial, the rate of increase in rectal temperature was a significant predictor variable of eHSP 72 expression. For the expression of eHSP 27, blood glucose was a significant predictor variable in the 60% trial. No predictor variables were found for eHSP 27 concentration in the 75% trial. Malondialdehyde (MDA) concentrations showed a significant reduction 24 hours after the completion of exhaustive exercise. MDA is one of the final products of polyunsaturated fatty acids peroxidation in the cells. An increase in free radicals (REDOX) is thought to cause overproduction of MDA, which wasn't seen in this investigation. MDA level is commonly known as a marker of oxidative stress and the antioxidant status in cancerous patients. Importantly, the correlation of glucose and FFA to eHSP 27 and MDA, may be an important aspect to bear in mind, when we later discuss the energy consuming species of the gut biome, REDOX and the immune system. Aging, HSP and cytokines (IL's and TNF-alpha) As we age, we lose our tolerance to heat and cold, suggesting a gradual loss of HSP over time. In community-dwelling elderly, serum HSP 70 and IL-10 concentrations were significantly lower and IL-6 was significantly higher when compared to healthy young control subjects. Elderly patients presenting inflammation (CRP serum levels ≥5 mg/L) showed significantly higher Hsp70 values; and Hsp70 correlated positively with IL-6 and CRP, but not with TNF-alpha or IL-10. A significant association was also noted between Hsp70 levels and the degree of dependency and cognitive decline in geriatric patients. This data provides evidence that serum concentration of Hsp70 decreases with age in a normal population. This study also showed that higher levels of Hsp70 are associated with inflammation and frailty in elderly patients (Rose et al (2011), BMC Immunology, 12, 24, 28 March) https://link.springer.com/article/10.1186/1471-2172-12-24. Therefore, too much IL-6 appears to be a bad thing, however, later we will discuss how increases in IL-6 in response to an acute stress induces the release of anti-inflammatory cytokine such as Il-10. Moreover, chronically elevated anti-inflammatory substances can lead to desensitisation. Therefore, it will be argued that it's the 'randomised regular intermittent impulse', whilst exercising, which tunes the system, through the laws of thermodynamics and entropy (chaos)! Age, Heat Shock Proteins, COVID-19 and thrombocytes (clots) COVID-19 seems to disproportionately affect older people. Young people, who have a more robust 'innate' and 'younger' immune system seem to be, with some exceptions (Kawasaki Disease), immune to the disease. Some people with COVID-19, aged 20-40 years old, are presenting with neurological complications from prolific clot formation. Clots are formed from thrombocytes. Thrombocytes are formed from platelets. Investigations suggest that HSP70 and HSP90 can serve as signalling scaffolds, helping regulate function, including platelet adhesion and spreading via modulation of protein phosphatase activity. HSP27, on the other hand, may be more involved in controlling actin polymerization during the platelet shape change and subsequent aggregation (Polanowska-Grabowska R & Gear AR 2000 Platelets. Feb 11, 1, 6-22). Several roles may exist for HSPs in the immune system including intracellular roles (e.g., antigen presentation and expression of innate receptors) as well as extracellular roles (e.g., tumour immunosurveillance and auto-immunity). It has been observed that exogenously administered HSP induced various immune responses in immunotherapy of cancer, infectious diseases, and auto-immunity. Moreover, virus interaction with HSP as molecular chaperones showed important roles in regulating viral infections including cell entry and nuclear import, viral replication and gene expression, folding/assembly of viral protein, apoptosis (cell death) regulation, and host immunity (Azam B & Elnaz A Clinica Chimica Acta 2019, 498, 90-100). As already stated, viruses could regulate host HSPs at different levels such as transcription, translation, post-translational modification and cellular localization. Notably, COVID-19 seems to have unprecedented auto-immune response in those critically ill patients. Platelets Platelets are anucleate cell fragments known for their central role in coagulation and vascular integrity. However, it is becoming increasingly clear that platelets contribute to diverse immunological processes extending beyond the traditional view of platelets as fragmentary mediators of haemostasis and thrombosis (clot formation). There is recent evidence that platelets participate in: enhancement of adaptive immune responses recruitment and promotion of innate effector cell functions intervention against microbial threats modulating antigen presentation. In this way, platelets should be viewed as the under-appreciated orchestrator of the immune system (Ramadan et al 2015, Curr Trends Immunol. 16: 65–78). Pulmonary embolus and venous pulmonary clots Growing clinical evidence is finding severe clotting in some individuals with COVID-19. Moreover, pulmonary clots and even strokes have been reported in young individuals (aged 20-40) by an Australian physician in New York (Washington Post 26 April 2020), In fact, the clotting was so profound that re-clotting was occurring during clot busting surgery. Pulmonary venous clotting has also been described by French physicians. A research letter (9 April 2020) from Hôpitaux Universitaires de Strasbourg published in Radiology reported that of 106 pulmonary CT angiograms performed for COVID-19 patients over a one-month period in a tertiary care centre in France, 32 patients (30%) had acute pulmonary embolus (PE). This rate of PE is much higher than usually encountered in critically ill patients without COVID-19 infection (1.3%,) or in emergency department patients (3 to 10%). In the study, a D-dimer threshold of 2660 μg/L detected all patients with PE on chest CT. A second research letter published, described a study from Centre Hospitalier Universitaire de Besancon in France pointed to high proportion (23%) of COVID-19 patients with contrast CT had PE. PE was diagnosed at mean of 12 days from symptom onset. Patients with PE were more likely require care in the critical care unit and to require mechanical ventilation. (https://www.sciencedaily.com/releases/2020/04/200423143100.htm) Therefore, there is strong evidence of a combined airway-vascular response leading to organ failure. Such a combination of a 'cytokine storm' and thrombocytic events incorporating auto-immune responses leading to respiratory failure and the need for intubation and ventilation, and even clot busting surgery, in young people. Heat Shock Proteins, Exercise and Upper Respiratory Tract Bacterial Count (Int. J. Med. Sci. 2020, Vol. 17) Exercise modifies airway immune responses and susceptibility to infection in healthy individuals. Investigators (Min et al 2020 Int J Med Sc, 17, 5, 640-646) examined the effects of exercise on HSP 27 and HSP 72 expression levels in nasal mucosa of both professional competitive athletes (volleyball) and non-athletes. Nasal lavage (NAL) fluids were collected from 12 male professional volleyball players and 6 healthy males pre-submaximal exercise (running for 30 min at 70-80% of maximal heart rate) and post-submaximal exercise. Expression levels of HSP27, HSP70, Interleukin (IL)-8, and Tumour necrosis factor (TNF)-α in NAL fluids were quantified and antibacterial assay using Staphylococcus aureus was performed to assess the immunological role of HSPs in NAL fluids. In non-athlete controls, HSP27, HSP70, and IL-8 were unchanged after exercise. In the professional athletes, HSP70 expression declined significantly (p<0.05), but HSP27 was not significantly changed. nor were IL-8 and TNF-α. Further, it was found that the number of active bacterial populations were influenced by the presence or absence of HSP27 and HSP70 in NAL fluids. Upon removal of HSP27 and HSP70, the initially observed augmentation of anti-bacterial activity in post-exercise NAL fluids was abolished. This is a super-interesting result, where reduced HSP concentrations were correlated with improved bacterial counts, suggesting that HSP can reduce 'good' or functional bacteria in the mucosa. Moreover, there seemed to be difference in the innate immune response, to exercise, in trained vs untrained. The influence of bacteria and the gut biome will be discussed later in relation to the immune system. Additionally, of even more interest is the effect of training on pre exercise HSP levels. Needless to say, a balance of HSP is required for a balanced mucosal bacteria and that the resting HSP levels in athletes is lower than in non-athletes. However, it needs to be said that the non-athlete group was only 6 compared to 12 athletes. Regardless, the trained athletes appear to have lower basal levels of HSP. Importantly, this could be the result of 'over-training' and/or it makes sense that training creates the optimised system which conserves these vital proteins for essential use. Notably, as we age, the number of HSP reduce, so ideally, our immune biological age is younger than it's chronological age. A systematic literature review (Moreira A et al (2009) British Med Bul, 90, 1, 111–131, https://doi.org/10.1093/bmb/ldp010) (of 30 studies, comprising 4 descriptive, 18 observational and 8 randomized or controlled reports, that included a total of 8595 athletes, including 5471 runners and 2803 swimmers and 1798 non-athletes) found athletes were more susceptible to upper respiratory tract infections (URT) than non-athletes after prolonged and intense exercise. They postulated that the significant immune suppression (down regulation) was a protective response to limit inflammation. Furthermore, they hypothesised that as the fitness of the athlete increased, the incidence of URT should decrease, contrary to their findings. However, they also described data in marathon runners taking Vitamin C (anti-oxidant), where it was found to reduce the incidence in URT. In one study which they reviewed, the gut biome was considered to be important, where Lactobacillus fermentum appeared to have a slight anti-inflammatory effect, reflected by a decrease in IL-6 production, which is the main inducer of C-reactive protein and a decrease in the number of monocytes, which are one of the major producers of IL-6. Consumption of carbohydrate-rich beverages during exercise appears to attenuate some of the immunosuppressive effects of prolonged exercise, but confirmation of any clinical significance in this awaits further research. Exercise and Respiratory Tract Infections A narrative review (Pederson & Toft, 2000, https://bjsm.bmj.com/content/34/4/246) highlights evidence that exercise across a lifespan seems to increase resistance to upper respiratory tract infections, whereas repeated strenuous exercise suppresses immune function. There was no assessment of the reliability of data in the included studies. In an overview, researchers (Rocco et al., 2018) analysed data from four systematic reviews (including an older version of the Cochrane review; 14 primary studies) to examine clinical effectiveness of exercise to prevent upper respiratory tract infections. The authors were able to meta-analyse five randomized trials involving only 311 participants. They observed a reduction in incidence of infection (RR 0.84, 95% CI 0.65 to 1.10; 72 infections less [157 less to 45 more] per 1000 people) in people randomised for moderate intensity exercise for 8 weeks to 12 months. The evidence was judged “very low” quality based on GRADE, meaning the findings are highly uncertain. Martin et al (2009, Ex Sp Sc Rev, 37, 4, 157-164 doi: 10.1097/JES.0b013e3181b7b57b) suggest outcomes following respiratory viral infections are improved after moderate exercise based on epidemiological evidence and animal models. They propose stress hormones stimulated during exercise reduce excessive local inflammation and skew the immune response away from a TH1 and toward a TH2 phenotype. Human studies and experimental modelling of mechanisms are lacking. Heat Shock Proteins and the 'viral' diseased state Heat shock proteins (HSPs) are recognized for their support of protein metabolism. Interaction with viral proteins also functions to enhance the development of innate and adaptive immune responses against the infecting agent. At the level of the infected cell, HSP are uniquely expressed on the cell surface, where they represent targets of lymphokine activated killer cells. Necrosis of the infected cell releases complexes of HSP and viral protein, which, in turn, binds antigen-presenting cells (APCs). One effect of binding is to stimulate APC maturation and the release of proinflammatory cytokines, an adjuvant effect, that prepares the way for adaptive immune responses. A second effect of binding is to direct the antigenic cargo of the HSP into endogenous MHC presentation pathways for priming of naive cytotoxic T cells (CTL) or activation of antigen-specific CTLs. For example, this alternate pathway of antigen presentation is essential to CTL priming following primary brain infection such as in measles (Oglesbee et al 2002, Viral Immunology, 15, 3, 399-416) Both HSP72 and HSP27 has been implicated in different disease states playing both protective and counter-protective roles. In multiple disease contexts, HSP-27, plays a role in renal injury and fibrosis, cancer, neuro-degenerative and cardiovascular disease (Vidyasgar et el 2012, Fibrogenesis and Tissue Repair, 5, 7, (https://link.springer.com/article/10.1186/1755-1536-5-7). Interestingly, HSP27 has been characterized with the ability to regulate actin cytoskeletal dynamics during heat shock and other stress conditions, functioning both to promote actin polymerization and as an actin capping protein (Guay J et al (1997) J Cell Sci, 110: 357-368; Huot et al (1996) Cancer Res., 56: 273-279). This capping function is important in respect to DNA splitting where telomeres are the caps at the end of each strand of DNA that protect our chromosomes, like the plastic tips at the end of shoelaces. Without the coating, shoelaces become frayed until they can no longer do their job, just as without telomeres, DNA strands become damaged and our cells can't do their job. HSP 70 has been associated with CNS responses to viral load from measles. Importantly, this model suggests a self-perpetuating (positive feedback) HSP expression with virus gene expression, which in turn stimulates innate immune responses in macrophages of the brain microglia (Kim & Oglesbee 2012). The extracellular HSP70 is a ligand for TLR2 and TLR4, activating signal transduction pathways that drive type 1 IFN expression (IFN-β in brain) and expression of antigen presenting complexes (MHC). IFN-β expression by brain macrophages is key to immunity against virus infected neurons (in a mice measle model). However, studies that directly examine the contribution of HSP70 to antiviral immunity and the impact upon viral virulence are lacking. When looking at the HSP70 family as a whole, their fundamental role in protein metabolism and the abundance within cells reinforces their potential support of viral replication at multiple levels. For every step, in viral replication (i.e., attachment/penetration, uncoating, transcription and genome replication, and virion morphogenesis), one can cite an example of a viral system that draws upon an HSP70 family member for support. Heat Shock Protein 90 (HSP-90), Geldanamycin and COVID-19 : 19 May 2020 An interesting article on drug repositioning (defined as the use of approved drugs for new indications), offering an unmatched opportunity to offer novel therapeutics to treat SARS family of coronaviruses (SARS-FCoVs); Researchers analysed, a dataset of patients who presented with SARS during the 2003 outbreak whereby they established a gene signature that defines differential gene expression in patients who were sick with SARS vs. healthy controls and convalescent patients. They used a robust platform to conduct drug repositioning based on clustered gene expression and pathway enrichment to identify best matching drugs. They identified 55 agents of potential benefit. In most of these drugs they were able to establish a link to previous related research, use as antiviral, or at least a hypothetical role in treating SARS-FCoVs. Most notably, the heat shock protein 90 (HSP 90) emerged as a major component that enables viruses to hijack infected cells through the process of autophagy (self devouring). Almost half of the drugs identified could be linked to HSP 90. As such, they propose using HSP 90 inhibitors, mainly geldanamycin and its derivatives, to treat COVID-19. (https://www.researchsquare.com/article/rs-18714/v1) Based on their findings, they suggest adding more drugs to the experimental arsenal deployed against SARS-FCoVs. These included the use of nontoxic drugs that are readily available for wide scale prophylaxis or for the treatment of mild cases of COVID–19. These drugs would include omeprazole, nonsteroidal anti-inflammatory drugs, colchicine, sulfoanamide antibiotics, antimalarial drugs and clozapine/chlorpromazine. For patients with serious COVID–19 illnesses, the above drugs can be combined with immune modulators like sirolimus, and direct HSP 90 inhibitors under well-designed clinical trials. Given the high pathogenicity of the current ongoing epidemic, they suggested that it seems prudent to attempt to use multiple drugs in combination if low risk toxicity and drug-drug interaction is established. Choosing a combination of drugs identified in this study or other drug-repositioning studies and careful reporting of the efficacy of these experiences can result in rapid accumulation of knowledge.(Iyad Sultan, Scott Howard, Abdelghani Tbakhi (2020, DOI : 10.21203/rs.3.rs-18714/v1). Therefore, albeit evidence from another class of HSP, it is plausible that fine tuning (down regulation from regular exercise) of HSP function is equally important to it's subsequent role as a fine tuner of cytokine - immune responses. This is an interesting finding, as one of the functions of another class of HSP (HSP 70) is the inhibition of apoptosis (cell death) which could be considered to enhance viral replication by preserving the viral factory. Inhibition of HSP 70 expression in human breast tumour cells result in massive cell death. Conversely, adenovirus infection causes a dramatic suppression of HSP 70 mRNA levels during the late phases of the viral replication cycle when the viral particles are already assembled, enhancing apoptosis in order to promote viral particle release (in Mi Young Kim and Michael Oglesbee 2012 Cells 1, 3, 646–666.doi: 10.3390/cells1030646). This suggests that HSP importance and function varies depending on the stage of the disease. A cycling dynamic of HSP outliers from the pathogen and host itself. Mechano-transduction: how does a mechanical force transduce to a thermodynamic energy system? We all know the feeling after unaccustomed exercise. Delayed Onset Muscle Soreness (DOMS); that feeling of heaviness and stiffness which worsens over a 2 day period. After the first run, on soft sand, in many years, resulting in the inability to walk down any stairs except backwards! Scientists describe it as 'broadening and streaming of the z-bands'. These are the micro-filaments between actin-myosin sliding filaments (introduced by Huxley 1957) which allow our muscles to lengthen and shorten. Additionally, an elastic element has been incorporated which is considered to be made up of passive collagen tissue (such as myofascia and tendon - which isn't quite true, as these tissues fibroblasts have motility and can change the structural integrity/density ), as well as myofilaments such as Titin. Furthermore, the cycling of ATP-ADP energy reserves give muscle another (sinusoidal) elastic element when doing exercise such as running or plyometric jumping-counter jumping. Did you know muscles require energy, in the form of ATP, to relax? Hence, the contracted rigid muscle (e.g. rigor mortice or cramp) can be considered a lower energy state than a relaxed one! Paradox? However, the eccentric (lengthened) contracted muscle, which requires less EMG activity (than concentric contractions) enhances the potential recoil for concentric (muscle shortening) contractions. In biomechanics, the Hill model of muscle thermodynamics was developed in the 1930's and redefined in 1974. Still today, it's considered as fundamental in any conservation on muscle dynamics, where an inverse relationship exists between muscle velocity and force production. This has direct bearing on the development of power (P=Fv or P=F. δ s/t). Considering energy, where Work = Power x time, it becomes apparent that the displacement of sliding filaments resulting in muscle lengthening and shortening defines the use of derivations from the laws of thermodynamics. The following is taken directly out of the seminal paper of 1974. Homsher E, Mommerts WFHM, Richhiuti NV (January 1974) The Journal of General Physiology Apart from calorific energy values, this model has practical implications, where an optimal velocity (change in displacement over time) and muscle length dependent force, develops optimal power i.e. the rate at which work is done (which, like your energy bill, is measured in Watts) Plyometrics such as the one depicted above, can induce severe muscle soreness (DOMS) in the uninitiated. However, in the trained, this form of training has been known to improve the ability to run and jump. Actin-myosin cross bridge model (Huxley 1957) Force-velocity temperature dependent model (Ranatunga KW 1984 J Physiol. 351, 517-29) Cross filament model and four kinetic phases of half-sarcomere (hs) shortening following steps to the loads indicated (Ranatunga KW 1984 J Physiol. 351, 517-29) Later, Piazzesi G et al (2007 Cell 16, 131, 4, 784-95) demonstrated that it was the number of myosin motors rather than motor force or stroke size which determined force production at varying velocities, thereby providing a molecular basis for the parabolic relationship described earlier. However, later we will describe a large micro-filament called 'Titin' which has been considered the 'spring' in the system Discrepancies exist at low and high loading when using variations and additions to Hills equation. These have been attributed to the internal kinematics of actin-myosin, as well ADP-ATP energy cycling through the sarcoplasmic reticulum. However, non-linear mechanics (deterministic chaos theory) would expect such rules to break down at the extremes...and new predictive rules should take their place. That is, the 'outliers' define what 'norm' it isn't. This sliding filament system (https://www.back-in-business-physiotherapy.com/images/videos/muscle_contraction.mp4) has been modelled into a modification of Hooke's Law, Young's modulus of elasticity (using microfilament Titin as the spring) and the oscillating mass-spring. This was extrapolated, at a later date, into Bernstein's perspective of 'degrees of freedom' and motor control (adding a cognitive perspective). As the muscle shortens and lengthen it generates heat, based on tension and displacement and the load applied. The concepts of concentric (muscle shortening) vs eccentric (muscle lengthening) muscle contractions, as related to energy and the immune system will be discussed later. Subsequently, inverse dynamics was extrapolated to describe the transfer of energy across accelerating body parts (inertia) through 'muscle energy straps'. Put simply, muscles which cross just one joint, tend to be deeper muscles and act as stabilisers across the joint, whereas the bulkier, more superficial, two joint muscles, are the energy straps. This is linear dynamics which we generally learn of at school. The following will describe this in more detail. Later I will examine non-linear dynamics and deterministic chaos elsewhere in the treatise. Therefore, the development of Τorque through the movement of body parts (inertia), conservation of momentum (energy), the production of potential/elastic energy describes a 'perfectly stable' sinusoidal system. However, it is becoming more apparent, that the imperfections in the system, are what drives a healthy and optimised process of power (P = Force x velocity) production and work (W=Power x time) output. Obtaining, transforming, and using energy to do work may seem simple. However, the second law of thermodynamics explains why these tasks are harder than they appear. None of the energy transfers we’ve discussed, along with all energy transfers and transformations in the universe, are completely efficient. In every energy transfer, some amount of energy is lost in a form that is unusable (as work). In most cases, this form is heat energy. Thermodynamically, heat energy is defined as the energy transferred from one system to another that is not doing work. However, what if that heat is activating HSP or other immune-metabolic procesess? Entropy Some energy is lost as heat energy during mechanical and cellular metabolic reactions. This is good for warm-blooded creatures like us, because heat energy helps to maintain our body temperature as well as regulate HSP. As stated, strictly speaking, no energy transfer is completely efficient, because some energy is lost in a 'so called' 'unusable form'. This is called entropy but ignores concepts from deterministic chaos. The traditional definition of entropy is1. a thermodynamic quantity representing the unavailability of a system's thermal energy for conversion into mechanical work. Often interpreted as the degree of disorder or randomness in the system."the second law of thermodynamics says that entropy always increases with time"2. "lack of order or predictability"; "gradual decline into disorder". However, the latter definition 'of the gradual decline into disorder' is not what is seen when examining high performance cycling demands or when looking at muscle paralysis. In fact, it will be shown that the supposed 'decline' into disorder of the EMG readings result in predicting a more optimised function. Entropy and Low Back Pain In Musculoskeletal Physiotherapy there has been an emphasis on 'normal'. What is normal function and what are the constraints of a functional movement pattern. Reductionist approaches are taken to ascertain the directions of movement of 'preference' versus those of 'avoidance'. Avoidance in the acute stage of an injury frequently involves 'unloading' the injured area, whereas people with chronically painful movement frequently 'overload' the area of dysfunction. Ironically enough, their movement becomes 'predictable' and less varied. Furthermore, the reduced variability leads to either 'increased control' and less adaptability, or 'reduced control' and increased loading of 'fatiguable structures' (Thiry et al Entropy2022, 24(4), 437; https://doi.org/10.3390/e24040437). Hence, the danger for the physiotherapist is to 'drill' down to the 'offending' structure or movement, but not progress rehabilitation far enough, to include the variety entailed in the full spectrum of complex movement and loading, which is required for motor control in 'predictable' and 'unpredictable' environments. Similar, to the 'Butterfly Effect' in non-linear mathematics, optimisation ultimately requires a chaotic system of control, manifested by 'outliers' which determine the 'damping' or 'amplification' of an oscillating system. Similar, to the 'Butterfly Effect' in non-linear mathematics. Cycling, concentric contractions and optimisation of cadence frequency using entropy considerations One of the key determinants of muscle co-ordination and movement efficiency during cycling is pedalling cadence consistency. Such cadence needs to occur across multiple joints and limb segments. Whereas, inverse dynamics requires changes in velocity to achieve accelerating body parts. So, in the absence of changes in cadence, how can changes in acceleration be incorporated into the model of cycling efficiency? In-order-to achieve minimal neuromuscular fatigue, optimal pedal cadence for long distance cyclists tends to be between 85 and 95 revolutions. In contrast, maximum power (as in track cyclists) is achieved with pedal cadences between 110-135 rpm. Higher pedal rates lead to shorter duration pedal cycles, coupled with longer duty cycles, recruitment of fast twitch muscle fibres and de-recruitment of slow twitch muscle fibres leading to significant inefficiencies and loss of power at higher cadence. Furthermore, people with long limbs aren't able to develop the same moments of inertia compared to shorter limbed people. To conceptualise the latter, think of the case of the ice figure skater spinning with arms close to midline vs stretched out from midline. Chaos theory would suggest that the randomization of movement pattern, requiring perturbations of periodicity, may make the scaling of muscle action/inaction important, when considering minor fluctuations in cadence and moments of inertia. Similar to the mass-spring model described previously, a system with three orthogonal axis and a fixed point of perturbation, which has a moving point of seemingly random perturbations and everything else, can be envisage. These random perturbations are the 'outliers' which traditionally have been statistically removed from linear dynamic models. However, they should be included, as only in this way can a cadence of constant velocity be used to describe efficiency. Perturbations from the manifold, new temporary fixed points of oscillation, magnify and fine tune the system As such the intrinsic firing pattern (motor unit potential shape, firing rate variability , coherence between motor units) of muscles need to be established. Additionally, their co-ordinated firing pattern across the same muscle, other muscle synergies on the same body segment and muscles of different body segments executing the same motor task, should ascertain 'extrinsic' firing patterns. That is, one wishes to determine the influence of oscillations within muscles and the influence of oscillations from not only nearby motor units but also from nearby muscles as well. The deterministic chaos of nearby oscillations influencing the prime parameter. (Krause M and Preston R 2002) A term entrotropic half life (EnHL) using EMG was coined and developed to examine what limits mechanical power output at higher cadences above 120rpm. Hodson-Tole et al (2020, Med Sc Sp Ex, 52, 1, 214-224) found that, in trained male cyclists (~ 10000km/yr, average 33yrs), changes in the individual muscle excitations can occur even when changes in co-ordination were more limited. Importantly, they demonstrated that features of the EMG change in a non-linear fashion with increasing cadence and that both 80 and 120 rpm represent inflection points, hinge points or potential manifolds critical in EnHL relations. In other words, cadences less than 80rpm and higher than 120rpm may have fewer fluctuations in muscle recruitment or firing characteristics leading to reduced application of force at the pedal. This variability is particular true for the bi-articular muscles, such as the gastrocs (medial and lateral), biceps femoris, rectus femoris, whereas the vastus medialis and vastus lateralis (one joint muscles) reached a minimum at 80rpm and did not change across the faster cadences studied. In this day and age of gears and the optimisation of mechanical ratios for optimal cadence, we lose light of the fact that cyclists once rode without gears and until only a few decades ago (1980's) elite cyclists used very high gears (12-20 teeth rear cluster) on dirt roads and mountain passes. My personal experience, of this time, is that I felt I had a number of gears within my muscle synergy, which I could call upon to change (in this case increase) my overall velocity. This internal gearing system was at the random mercy of the variable terrain which we encountered. Deterministic chaotic input generating an internalised randomised gearing ratio, preventing fatigue? In orienteering, people talk of internal calm, whilst running and thinking at maximum endurance power. Later in this dissertation we'll take a look at an 'uncontrolled manifold hypothesis' in orienteering which is employed as an experiential learning strategy to teach predictive reasoning (through map reading), i.e. the random from the non-random, in novel terrain. This is done through a process of filtering, contrasting the 'value' of the information and subsequent minimisation of certain information and magnification of predictive 'outliers'. That data used is that which doesn't 'cloud' the 'fidelity' within the cognitive domain. Later, we will also examine the effects of 30Hz electrical input into exercising muscles for the magnification of that muscles representation in the brain. Similarly, the lack of gears in track cycling has been exploited to produce endurance road world champion cyclists, potentially by forcing an internalisation of 'fidelity' to draw out the maximum (myosin motor unit) efficiency in the system. Arguably, this recruitment of motor units, is similar to a team sport, where individual players are strategically 'engaged', so as to maximise 'players', and minimise 'passengers' in the game. Game theory will be discussed later. Eccentric muscle contractions, loading, damage and adaptation : how a mechanical force transduces to a cytokine reaction We've examined potential and kinetic energy and thermodynamics in the muscle models of power production. Using concentric (muscle shortening) contractions it could be shown that the energy state change, and heat is dissipated. This heat might be what drives the heat shock proteins (HSP's) which we discussed earlier. What those models don't take into consideration are eccentric (muscle lengthening) contractions and their influence on muscle elasticity (stiffer -> less elastic = more damping) as well as the potential myofilament damaging aspects of this sort of exercise. What is also of particular interest is how eccentric contractions can exert more force for less EMG input (compared with concentric contraction) and how the concentric contraction is better if immediately preceded by an eccentric one. The latter being the principle behind plyometrics training such as jump downs and counter-jumps. Touron et al (2019) examined the impact of eccentric vs concentric training on body composition and energy expenditure. Typical eccentric exercises are plyometrics and downhill running. Eccentric training is well known for inducing greater micro tears and severe post exercise muscle soreness (DOMS). It is associated with distinctive inflammation patterns and repair processes that are particularly effective in promoting adaptations, such as skeletal muscle hypertrophy (Roig et al 2009, Br J Sports Med, 42, 8, 556-568) and mitochondrial H2O2 production ((Isner et al 2014, Muscle Nerve, 50, 5, 803-811). Eccentric exercises are, considered to be, particularly useful in cardio-respiratory compromised people, as localised muscle contractions can be made without large cardiac demands. Moreover, Touron et al (2019) found beneficial effects of exercise on body composition (lean body mass), particularly with eccentric exercise (vs concentric) at high muscular, but low cardiorespiratory, loads. The mechanical 'spring' of the muscle may be considered as that of one of muscles largest proteins 'Titin', which spans an entire half-sarcomere from Z-disc to M-line. Titin functions as serially linked springs that develop tension when stretched. There are multiple titin isoforms that vary in size and stiffness, which explains the elastic-stiffness diversity across vertebrate muscle (mouse ->elephant). Because of titin’s structural properties, its most significant role may be as the muscle spring (https://www.jospt.org/doi/pdf/10.2519/jospt.2003.33.10.557). Evidence suggests that small heat shock proteins that protect the cytoskeleton structures (e.g. titin) increase dramatically after repeated eccentric bouts (Koh TJ. 2002 Ex Sport Sci Rev. 30, 117-121). If titin is functioning as a locomotor spring, then it should be tuned to the frequency of muscle use and adapt in response to changes in physiological demand due to exercise or disease. This notion has been reinforced as titin isoform expression has been reported as an adaptable property of striated muscle (Bell SP et al 2000 Circ Res. 87, 235-240). see video : https://www.back-in-business-physiotherapy.com/images/videos/muscle_contraction.mp4 Apart from mechanical considerations, metabolic aspects of loading, energy transduction and fatigue should also be examined. We found specific fatigue characteristics with eccentric/concentric contraction regimes (Krause M & Preston R 2002). What is known, is that this muscle damaging and fatiguing process, has a very powerful and potent training effect, if repeated in a dose specific manner, using temporal and intensity considerations. What is unknown is whether randomisation (chaos) in this form of training attains better results once a person has become accustomed to it. Logic would suggest yes. It can be argued that it's this microtrauma and subsequent dyskinesia, which induces an inflammatory-immune response. However, the other hypothesis are - heat production and subsequent entropy (already discussed) - that it's the asynchronicity or 'outliers' of control (chaos) which generates an immune response as well as arguing - that it's a metabolic-immune compromise which generates the cytokine response. Furthermore, - one should consider the effect of muscle tremor whilst doing such exercise and whether this is what is needed to readjust the system to a new stable state or even reverse a gradual decay from a previously stable state? Muscle damage during eccentric exercise and immune markers Bruunsgaard H, Galbo H, Pedersen BK, et al. (J Physiol (Lond) 1997, 499, 833–41) compared concentric and eccentric ergometer bicycle exercise and found an association between increased IL-6 level and muscle damage (seen by the increase in creatine kinase). Importantly, the level of IL-6 increased more during the eccentric exercise, and a significant association was found between peak IL-6 and peak creatine kinase on the subsequent days (r = 0.722; p = 0.028). The eccentric bicycle model results in delayed muscle damage, with peak creatine kinase levels on day four or five after exercise. Researchers (Ostrowski K, Rohde T, Pedersen BK, et al. 1998 J Physiol (Lond) 508,949–53) were able to detect IL-6 mRNA in skeletal muscle biopsy specimens obtained from runners after a marathon. These data indicate that IL-6 is locally produced in response to strenuous exercise or exercise induced muscle damage. IL-1ra mRNA was not present in the skeletal muscle, but was expressed by blood mononuclear cells obtained after, but not before, the marathon, suggesting that locally produced IL-6 induces a systemic anti-inflammatory response. Sarcopenia - loss of muscle cells and hence bulk If we don't exercise regularly, our muscles atrophy, i.e. they become smaller. However, with exercise, we can reverse this process of atrophy. After a certain age, in addition to disuse atrophy, the muscles cells can be destroyed forever (apoptosis), with inactivity. This process is called sarcopenia and commences in the fourth decade of life, in sedentary individuals. As examined previously, a deterministic chaos was suggested as the TNF alpha oscillatory mediator of nuclear factor-κB (NF-κB) activation and subsequent transcription, is that which influences mitochondrial dysfunction. Investigators have found that MuRF-1, a muscle specific E3 ubiquitin ligase is an important regulator of ubiquitin-mediated protein degradation in skeletal muscle (Bodine et al., 2001 Science. 294, 5547, 1704-8). Transcriptional factors, NF-κB and FoxO3a translocate into nucleus and subsequently upregulate transcriptional activities of MuRF-1 under certain pathological conditions (Cai et al., 2004, 119, 2, 285-98.; Gumucio and Mendias, 2013 Endocrine, 43, 1, 12-21. Perry et al., 2016, Ex Immunol Rev, 22, 94-109) such as sub-clinical inflammation associated with obesity and diabetes. This suggests that inhibition of NF-κB and/or FoxO3a pathways is a promising target for preventing muscle atrophy. An exercising mouse diabetic model (Liu & Chang 2018, Front Physiol. 9, 636) has demonstrated significant muscle changes in, an eight weeks moderate-intensity exercise (5.2 m/min, 1 h/day, and 5 days/week for a total of 8 weeks) program, where mice ran on a motorized treadmill (30 min with 0° slope) and exercise duration was gradually increased from 30 min to the target of 1h (0° slope). These included improved tibialis anterior muscle mass, suppression of NF-κB signalling, as well reduced pro-inflammatory markers IL-6 and TNF-alpha. mm = control mice, db/dh = diabetic mice, Ex = exercise https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5987703/ So, ideally, we are exercisers for life. However, don't despair if you haven't been into fitness, it's never too late. You still have the ability, to slow down sarcopenia, as well as hypertrophy the remaining muscle. Remember, it's not just about the amount of protein, but also the thermodynamics of metabolism and repair which dictate our inflammatory-immune responses. This dynamic allows for the deployment of the immune system during a time of crisis. Muscle Glutamine It has been established that glutamine is an important fuel for lymphocytes and macrophages. Several lines of evidence suggest that glutamine is used, at a very high rate by these cells, even when they are quiescent. It has been proposed that the glutamine pathway in lymphocytes may be under external regulation, partly because of the supply of glutamine itself. Glutamine stimulates in vitro lymphocyte proliferation, lymphokine activated killer cell activity, and cytokine production.(Ardawi MS & Newsholme EA 1984, Biochem J, 217, 289–96; Rohde T, Ullum H, Pedersen BK, et al. 1995 J Appl Physiol, 79, 146–50; Rohde T, MacLean DA, Pedersen BK. 1996 Scand J Immunol, 44, 648–5036) Skeletal muscle is the major tissue involved in glutamine production and it is known to release glutamine into the bloodstream at a high rate. It has been suggested that the skeletal muscle plays a vital role in maintenance of the key process of glutamine utilisation in the immune cells. Consequently, the activity of the skeletal muscle may directly influence the immune system. The glutamine hypothesis suggests, that during intense physical exercise, or in association with surgery, trauma, burn, and sepsis, the demands on muscle and other organs for glutamine is such that the lymphoid system may be forced into a glutamine debt, which temporarily affects its function. Muscle-immune conversion "The human immune system is a highly intricate network of cells and molecules designed to keep the host free from infection and disease. Exercise is known to have a profound impact on the normal functioning of the immune system. Having higher age and sex-adjusted scores for cardiorespiratory fitness and performing regular exercise of moderate- to vigorous-intensity exercise that fall within ACSM guidelines has been shown to improve immune responses to vaccination, lower chronic low-grade inflammation, and improve various immune markers in several disease states including cancer, HIV, cardiovascular disease, diabetes, cognitive impairment and obesity. The ongoing COVID-19 pandemic has raised a lot of questions regarding how exercise can protect us from infection by boosting immunity. This is becoming more pertinent as many of us have restricted access to the gyms and parks where we would normally undertake exercise and physical activity regimens. Compounding this problem are the known negative effects of social isolation and confinement on immunity. Glucocorticoids such as cortisol are elevated during periods of isolation and confinement and can inhibit many critical functions of our immune system. When we are stressed, the ability of our T-cells to multiply in response to infectious agents is markedly reduced, as is the ability of certain effector lymphocytes (e.g., NK-cells and CD8+ T-cells) to recognize and kill cells in our body that have become cancerous or have been infected with viruses. It is also vitally important that our immune cells maintain their ability to redeploy so that they may ‘patrol’ vulnerable areas in or body (e.g., the upper respiratory tract and the lungs) to prevent viruses and other pathogens from gaining a foothold. This process is also important to minimize the impact of the virus and to expedite viral resolution should we become infected." (Richard J. Simpson, Ph.D., FACSM Mar 30, 2020) Note, a relationship exists during exercise with adrenaline, noradrenaline, neutrophils and natural killer cells with cortisol levels post exercise. Cortisol having an inhibiting/controlling influence on the immune pro-inflammatory response. Interesting to note that cytokine levels continue to rise during and after exercise. Hence, the duration of the period of the perturbations, of the immune regulating mechanism, could be assumed to have variable damping mechanisms, with higher or lower frequency, depending on the frequency, intensity and duration of exercise, as well as the period of recovery between sessions of exercise. Pedersen & Toft (2000) https://bjsm.bmj.com/content/34/4/246#block-system-main "Each bout of exercise, particularly whole-body dynamic cardiorespiratory exercise, instantaneously mobilizes literally billions of immune cells, especially those cell types that are capable of carrying out effector functions such as the recognition and killing of virus-infected cells. The mobilized cells firstly enter the blood compartment from marginated vascular pools, the spleen and the bone marrow before trafficking to secondary lymphoid organs and tissues, particular to the lungs and the gut where increased immune defence may be required. The immune cells that are mobilized with exercise are primed and ‘looking for a fight.’ Their frequent recirculation between the blood and tissues functions to increase host immune surveillance, which, in theory, makes us more resistant to infection and better equipped to deal with any infectious agent that has gained a foothold. Exercise also releases various proteins that can help maintain immunity, particularly muscle-derived cytokines such as IL-6, IL-7 and IL-15. The cytokine IL-6 has been shown to ‘direct’ immune cell trafficking toward areas of infection, while IL-7 can promote the production of new T-cells from the thymus and IL-15 helps to maintain the peripheral T-cell and NK-cell compartments, all of which work in concert to increase our resistance to infection. Exercise is especially beneficial for older adults who are more susceptible to infection in general and have also been identified as a particularly vulnerable population during this COVID-19 outbreak" (Richard J. Simpson, Ph.D., FACSM Mar 30, 2020) Over-training - variation between sympathetic and para-sympathetic tone Chaos Theory - non linear dynamics The key to exercise is not to over-train. But, to induce a response, you need to stress the system i.e create a perturbation. This fact is important in the whole spectrum of people, from the severely de-conditioned to the highly trained. Classic signs of over-training are waking tired in the morning, 'non-restorative sleep', and irritability, 'three bastards in a day or ask your partner or significant other'. The three bastards pertained to a time prior to lock-down, where it was said if you met a person who you really didn't like, then that was unfortunate, if you met a second one, in the same day, that was doubly unfortunate and if met a third, then it wasn't them, but you. Exercise requires an 'allostatic' (restorative) response by the body to mental or physical stress (see below). It's almost akin to chaos theory. Simple perturbations of the system oscillate back to the midline (linear dynamics), with the occasional outlier (non-linear dynamics). The more extreme the perturbations, the more extreme the damping mechanisms need to be, for the non-random predictive oscillations, such as mechanically intense and/or repetitive (ie metabolic, irrespective of intensity) unaccustomed exercise. But even in accustomed exercise, in a healthy body, there will be a random 'outlier'. The random outlier, in chaos theory, is not so random, but subject to three orthogonal variables, one of which is a 'locus of control'; or a 'damping manifold'. One system has influences on nearby systems. Simply stated, it is proposed that progressive exercise, building up of endurance and resistance improves our 'damping manifold' on a ratio by ratio basis. The more finely tuned, the more amplified the ratio. Such damping, or control systems, are potentially also employed in non-accustomed exercise, metabolically compromised situations, cognitively confronting and/or during immune challenges such as COVID-19. Deterministic chaos and cytokine modulation of cytokines In a seminal paper, ' A Systems Model for Immune Cell Interactions Unravels the Mechanism of Inflammation in Human Skin' the authors (Valeyev NV, Hundhausen C, Umezawa Y, Kotov NV, Williams G, Clop A, et al. 2010), used of deterministic chaos to explain cytokine oscillations for the modulation of one other (PLoS Comput Biol 6, 12, e1001024. https://doi.org/10.1371/journal.pcbi.1001024). Their model provides a quantitative description of multiple immune reactions based on cytokine profiles, including a model of 'immune system switching', similar to 'modal switching' between various immune states described earlier for the tuning of the NF-κB system by TNF. Specifically, the inter-dependency of the immune system is highlighted using two cytokine oscillations which can maintain a 'stable' homeostatic state as well as 'switched' to an activated stable homeostatic state, of higher cytokine concentration levels, in a dose dependent manner. The model used is the autoimmune inflammatory skin condition, Psoriasis. Skin inflammation associated with Psoriasis : whilst healthy skin contains inflammatory cytokines and macrophages, the inflamed skin contains a multiple higher concentration of those substances. This is a super interesting schematic, especially when examining IL-10 (anti inflammatory) and IL-22 (involved with cell survival and synthesis of anti-microbials for wound healing). These could be, speculated as, potential controlling 'outliers'. It also suggests that examining one cytokine response against it's baseline is relatively simplistic and potentially erroneous if it isn't examined with baseline changes of other coexisting cytokines. Dose Dependent Cytokine Production: Homeostasis occurs when the concentrations of cytokine production of two inter-dependent cell populations meet. Importantly this is circular, cytokine A stimulates cytokine B and vice versa. Immune - Subsystem Response : Green lines are trajectories and convergence of cytokine A and B. Purple spot and dotted line are the stable 'homeostatic' point. Arrow heads indicate the direction of non-equilibrium cytokine concentration towards the stable point and equilibrium. Situation B, where a small perturbation of one cytokine leads to a 'divergence' of the trajectories and in this case a three fold perturbation of the other (numbered 3). In C and D we can see a response two fold larger than the applied spike, meaning that a small impulse can lead to a large reaction both in healthy (and inflammatory) states. Presumably, the perturbating stimulus can arise during exercise, as cytokine release from muscle damage, such as eccentric exercises, and/or metabolic factors from oxidative processes (REDOX). Additionally, as the second law of thermodynamics still applies, the influence of heat shock proteins should also be considered. Cytokine Trigger Dynamics: Two points of homeostasis (H1 and H3 'stable') after one cytokine concentration moves out of phase (H2 'unstable') with the other. Trajectories 1 and 2 are from a lower to a higher and a higher to lower stable state (resp) with the latter occurring due to the application of cytokine B (depicted in E and F). The initial onset of signalling of cytokine A is depicted in trajectory 1, C and D. Presumably, multiple points of homeostasis could exist when confronted with varying degrees (concentrations) of inflammation and repair. Oscillatory Cytokine Concentration Dynamics : one of the 'unstable' solutions forms a limit cycle of cytokine oscillations, either around a stable point of convergence or a point of homeostasis; or any other point of 'unstable' cytokine concentrations. What is amazing, is how these nullcline diagrams look like synoptic charts. (remember Edward Lorenz and the Butterfly effect eluded to much earlier) Small amplitude perturbation results in oscillations whereas a larger amplitude results in a single spike. Noteworthy is that small perturbations result in a many fold greater response. Small perturbation results in a return to homeostasis. Resolution : one stable point at a lower cytokine concentration. Mathematics of 'deterministic chaos' and cytokine immune inter-dependence (Valeyev et al 2010) The rate of cytokine uptake Mol/sm2 by a cell population is proportional to the numberof receptors bound to the cytokine, multiplied by the total number of receptors on the cumulative cell surface: Full immune model equation is thus given by the formula The complete dynamic mathematical equations of interactivity between inter-dependent cytokine populations (A Systems Model for Immune Cell Interactions Unravels the Mechanism of Inflammation in Human Skin' (Valeyev NV, Hundhausen C, Umezawa Y, Kotov NV, Williams G, Clop A, et al. 2010), and their use of a 'deterministic chaos' mathematical model to explain cytokine concentration inter-dependency (PLoS Comput Biol 6, 12, e1001024. https://doi.org/10.1371/journal.pcbi.1001024). Orienteering and the 'uncontrolled manifold hypothesis' of motor control and learning (cortical resource optimisation) Orienteering is a sport requiring the efficient movement through the forest, at high speed, along an optimal route, using a calm cognitive state during a high physiological state. Another paradox? Importantly, expertise in orienteering requires decades of experiential learning.in a potentially chaotic environment. This chaos being physical, as in uneven terrain, varying vegetation and varying geological formations. Additionally, it's potentially cognitively overloading, in the sense of navigating in potentially unique and new terrain, requiring totally different central nervous system (CNS) strategies to what they are used to. To learn, is to delve into the unknown........and the cognitively superior strategy may win over the physically stronger individual (game theory). These cognitive - mechanical concepts are entertaining when considering chaos theory and infinitesimal controlling mechanisms. Furthermore, simultaneously induced mental and physical stress, as well as exposure to environmental pathogens, adds another variable of considerable inadvertent influences on immune responses, which vary depending on the 'selective qualitative experiences' of the individual from their years of competition, conditioning, mental health and training. Game theory and variability of the 'outlier' for adaptability It is interesting to speculate that both the novice and elite orienteer are more susceptible to infection because they both have more rigid motor patterns, are less inclined to take risk and therefore are less likely to be confronted with error generating patterns of correctability? The assumption underlying game theory is that there is a resource over which there is a conflict. A factor which the orienteering paradigm partially defines, and identifies, is the freedom of thought and movement. That fact that many investigations are looking at exercise and the immune system, using captive animals, might be problematic in itself. These animals are in a predictable environment, which for this purpose is ethical, reductionist and conforms with rigorous scientific research protocols, which is practical, as it reduces the number of 'dependent' and 'independent' variables. However, from an evolutionary point of view, and from the perspective of the example used here, where in orienteering, more may be learnt and fine-tuned, in an unpredictable variable environment, whereby the use of caged animals may be limiting the validity of the paradigm (deterministic chaos) which is under investigation. Moreover, in terms of cognition, confinement is a stressor. Moreover, the calmness and clarity of thought needed in the freedom of orienteering (running and navigating) through the landscape can be considered the antithesis of the caged animal. Our ancestors were striving for energy security through appeasement, subjugation or dominance over other life forms, both internally and externally. In this sense, the 'freedom to navigate and move' paradigm, suggests that our evolutionary forefathers, used their muscles, to propel themselves out of Africa, for 'greener gut biome pastures'. Therefore, maintaining good health in new and potentially 'dangerous environments', involved an unpredictable deterministic variable. As it pertains to cognition, it is an intriguing idea that a motor-sensory curiosity, drove a mechanism, which simultaneously caused muscle hypertrophy, and endowed the muscles with enhanced glutamine and cytokine concentrations, which were needed, if an immune response to pathogens was encountered. Additionally, it is conceivable, that the gut biome was driven by the laws of thermodynamics, in the search for energy. Subsequently, the gut-environment interface provided the interaction needed, to both provide energy for movement, allowed the immune system the encounters needed to flourish, and achieved the abundance of gut species required, in a variety of situations, from feast to famine. Therefore, the gut - muscle - brain cognitive pathway, was driven at a conscious and subconscious level to meet the demands of thermogenesis and immune competency, resulting in collective gain amongst all cells which required energy. Akin to Zen Buddhist philosophy, suggestions are, that the constant sensation of mild hunger, drives the clarity of thought needed, to strive for all encompassing meaning and ultimate enlightenment. Yoga, using animal poses, to stretch muscles and enhance breathing, whilst calming the cognitive state, may be based on the same primeval paradigm, of what is good for muscles is also good for the gut and brain. The 'dove and hawk' paradigm in game theory is interesting. If a hawk and dove compete over the same resource, direct open conflict of the dove with the hawk would be suicidal. Hence, one would think it's better to be a hawk. However, what if two hawks meet, there will be only one winner and potentially both could be injured for the same net gain. Whereas, if two doves meet, they may postulate and gesticulate and eventually one may retreat or they may even share the resource, with the less risk of injury. Hence, the stakes for the Hawk are much higher. Humans have always been in conflict for resources. Does this mean that the immune system is tuned by adaptation to 'individual' resource dominance? Or, as people developed and evolved as tribes, into communities did our immune systems come to share pathogens, which may have entailed 'herd immunity' but at the same time, gave humans a lack of species variability, making them more vulnerable to 'novel' pathogens? Even more intriguing, is the notion that within a group of similar, the weakest may be driven out, seeking new resources, which in this case means new environments and new pathogens, invoking an 'immune enriching' response? Continuing with the 'hawk dove' analogy, if we have too many hawks in a population, the consequences are constant conflict. If too many doves, constant compromise. In fact, a single dove in a hawk environment might be totally ignored, as might a single hawk in a dove environment. Thus, the apparent weaker species could be at an advantage when it's the outlier? To carry this further, we could postulate that the hawk is more prone to injury. Does this mean that in humans, the more dominant 'aggressive' individuals have an immune system which is more in demand for potential or actual injury? Whereas, the postulating dove, activates it's immune system minimally when it's performing some form of escape or deception? Interestingly, most animal conflict encounters, go out of their way to avoid injuries to themselves. Regardless, it's likely, that in both 'stressful' situations, the immune and musculoskeletal systems are activated, in a proportionately preparatory manner. Thus, the stronger the variability in the individual, the more proportional, and therefore robust their immune response. Needless-to-say, a balance between hawks and doves needs to be established for mutual gain to take effect. In terms of the human genome, it's very underwhelming, yet it has evolved to a complex multi-cellular life form, still totally dependent upon trillions of unicellular life forms within the individual gut biome. This flies in the face of Darwinian evolution and the survival of the fittest, in that simple life forms keep complex life forms alive. Even, within the gut biome, there appears to be a symbiotic relationship with parasites and a healthy immune system (i.e. parasitic exposure appears to reduce auto-immune disease such as allergies). A 'simple' multitude (gut biome) balanced with a 'complex' minority (human DNA). Humans eat to feed their gut, their gut breaks down energy from food, which in turns propels the human, with the energy gained, to find more food. A net win win situation using the gut-brain-muscle axis. In terms of muscles, a simplistic view, (using this analogy) would be that the glycolytic (fast twitch) muscles are the 'hawks', whereas the oxidative (slow twitch) muscles are the 'doves'. The glycolytic muscle fibres tend to be ballistic two joint (mechanical) energy straps which propel the body, whereas the oxidative endurance (metabolic energy) muscles are one joint deep muscles tending to stabilise joints and prevent injury. Therefore, the 'hawks' make the large perturbations whereas the 'doves' dampen them. Luckily, there is a muscle glycolytic fibre type which can become more oxidative (endurance power). Hence, 'hawks' which can be tempered towards a 'dove' like mentality....a balance between metabolic and mechanical energy systems, where the mechanical perturbations stimulate the metabolic-immune response. In terms of neurophysiology, this analogy could potentially be taken further, where the sympathetic nervous system is the 'hawk' and the para sympathetic nervous system are the 'doves'. Fortunately, within the sympathetic nervous system there are self modulating ('dove' like) perturbating mechanisms. But it could be envisaged that putting a 'hawk' amongst the 'doves' wakes them up from a state of complacency. Similarly, 'staleness' is an 'existential threat' to any training regime and to any 'immune system'. Cortical 'resource' representation, mapping, in knee muscles, after injury In the context of physiotherapy, a simple model of game theory might be applied to the problem of anterior knee pain. Commonly, this problem is associated with pain at the front of the knee when it is in flexion (a bent position), such as stair climbing, cycling, squats, etc. The conventional wisdom is that the patella (knee cap) is mal-aligned due to a lack of medial (VMO) muscle activity pulling the patella inwards and too much activity of the lateral thigh muscle (VL) pulling it outwards. Game theory could be applied here as the muscles compete for finite cognitive territory to represent their individual (rather than mutual) function, where ultimately neither muscle gains, both loose out to pain generating cortical representations, reducing fidelity and increasing noise in the system. However, if the muscles were to readjust for a functional outcome, they would do so through gaining a synergy of proportionally shared resources (power sharing), hereby a dominance over pain and dysfunction is gained. Physiotherapists, use functional electrical muscle stimulation (FEMS) to give added 'resources' to the VMO, which then can be used during functional exercise training. As the system adjusts, the pain improves and the gain experienced by all the muscles convinces the VL to fire with the VMO, hamstrings and gluteals in a functional synergy for stairs, cycling (see previous), squats, etc. Hereby, game theory would suggest all have won and injury has been avoided. Investigations in Australia, by the Brazilian, Abrahao Baptista (2014), looking at 40-50 year old women with chronic knee pain, demonstrated the significant reduction in the volume of muscle representation in the cerebral cortices, as well as changes in the location of these muscle representations (see below). Moreover, in the context of neurons who 'fire together, wire together' it would be of utmost importance to find exercises that act as functional synergies and relate in a real or a 'virtual' manner to the environmental context in which they need to fire. This also becomes particularly important in psychological behavioural issues of 'fear avoidance' and disuse atrophy. Ideally rehabilitation stimulates 'wiring and firing together' of goal-oriented regions of the brain rather than those which are directed at fearing and avoiding movement. Therapist must instil confidence through their choices of treatment whereby they outline and hence monitor the expectations of outcome. In this picture, it is clear that, the volume of the quadriceps muscle representation in the cortex of people with anterior knee pain (PFP = patello femoral pain) is dramatically reduced. Not seen here, but demonstrated in other research, is the phenomenon of pain processing altering cortical activity in various brain areas (see below). Individuals with patellofemoral pain (PFP) had reduced map volumes and an anterior shift in the M1 representations, greater overlap of the M1 representation and a reduction in cortical peaks across all three quadriceps (RF, VL, VMO) muscles compared with controls.(Te et al 2017 Pain Medicine, pnx036, https://doi.org/10.1093/pm/pnx036). Physiotherapists use FEMS (30HZ functional electromuscular stimulation) to enhance muscle cortical representation in the brain, which improves function and in turn improves pain. FEMS stimulation readjusted cortical mapping to that seen in asymptomatic individuals. Alternatively, therapists use trans-cortical stimulation of the pre-frontal cortex to improve 'executive function' and pain. Brain activation related to spatial discrimination of noxious stimuli is distinct from that related to perceived pain. These images are located at x = 0 mm, x = 30 mm, z = 5 mm, and y = –30 mm in standard stereotaxic space. IPL/SPL, Inferior parietal lobule/superior parietal lobule; GP/PT, globus pallidus/putamen; M1, primary motor cortex; DISCRIM., discrimination. (Oshiro et al 2007 J Neuroscience, 27, 13, 3388-3394) Abrahao Baptista (2020) and his colleagues are conducting research into trans-cortical stimulation and vagal (para-sympathetic) nerve stimulation in the treatment of patients with COVID-19. They are basing their assumptions and working hypothesis on some positive results a rheumatologist has had with this methodology for the treatment of auto-immune inflammatory disease. COVID-19 has many of the hallmarks of an auto-immune disease, including the cytokine storm. This treatise has argued that sympathetic, rather than para-sympathetic, stimulation is necessary to add a deterministic chaotic input which perturbs the immune system into action. It would be intriguing to speculate a large perturbation between sympathetic and para-sympathetic can also activate the immune response. In this case, the illness has already set the sympathetic nervous into a heightened chaotic state, which needs additional buffering (redundancy) from the vagal nerve stimulation. Exercise induced disease "The road to hell is paved in good intentions" (Henry G. Bohn's A Hand-book of Proverbs in 1855) The chaos of infections and the assault on the immune system has been seen amongst endurance athletes, such as cyclists, endurance road runners and orienteers. Saturation of inflammatory immune markers by uncontrolled mechanical irritation or infectious diseases from ticks found in the forests of Scandinavia, have been espoused as a theory behind extremely fit people having catastrophic immune consequences. After intense long duration exercise, the functions of (CD 16 natural killer) NK and (CD 19) B cells are suppressed. Thus, the NK cell activity (the ability of NK cells to lyse a certain number of tumour target cells) is inhibited. Furthermore, antibody production in the circulation is inhibited, and local production of secretory IgA in the mucosa is inhibited (Pedersen BK & Nieman DC. 1998 Immunol Today, 19, 204–6) Too much of a good thing can become a bad thing. Where does the balance lie? In the chaotic state? Anti - carcinogenic effects of exercise Alternatively, it has been shown, albeit in mice, that aerobic training activates Interleukin 10, which is considered to have colon anti-carcinogenic effects (Frajacomo et al 2016, Med Sc Sp Ex, 47, 9, 1806-1813). This supports reports on the association of aerobic exercise and marked reduction of colon cancer risk in humans (Boyle et al 2011, Cancer Causes Control, 22, 12, 1647-1658; Cerin et al 2005, Cancer Epidemiology Biomarkers Rev, 14, 4, 1000-1002). A mechanism for the effect of exercise is the production of Interleukin 6 (IL-6) as a result of muscle damage during exercise, which has been demonstrated to stimulate anti-inflammatory cytokines such as IL-10 (Benatti et al 2015, Nat Rev Rheumatol, 11, 86-97). Importantly, as discussed previously, chronic increases in IL-6 are related to frailty in the aged population. However, in the acute scenario, significantly, the release of pro-inflammatory substances, stimulate the release of anti-inflammatory substances elsewhere, as well as the stimulation of the controlling mechanisms, in the location, where the pro-inflammatory substances are released. So, what are the controllers? When is too little recovery, too much exercise? Where and what are the balancing mechanisms of the cytokines? What behavioural methods can we use to improve our immune response? Allostasis Neural componentry and chaos Several investigations, examining surface EMG (electromyographic activity of muscles) using chaos and entropy theory, exist. Investigators, examining facial paralysis (Xiong et al 2014, Robot Intelligence Technology and Applications 2 pp 805-819), used chaotic analysis to extract new features of EMG, including correlation dimension, Lyapunov exponent, approximate entropy and so on. They discovered that the maximum Lyapunov exponents are all greater than 0, indicating that sEMG is a chaotic signal. Interestingly, correlation dimensions of sEMG on healthy sides are all smaller than that of diseased sides; and inversely, the approximate entropies of healthy sides are all greater than that of diseased sides. Consequently, they concluded that chaotic analysis can provide a new insight into the complexity of the EMG and may be a vital indicator of diagnosis and recovery in the assessment of facial paralysis Application of chaos theory to a model biological system was used to examine evidence of self-organization in the intrinsic cardiac (heart) nervous system (Skinner et al 1996, Integr Physiol Behav Sci. 31,2,122-46). Using a rabbit model and ischaemic events, on electrical activity in and around the heart, they found that it's the neutral organization that determines the specific beat-to-beat pattern of cardiac behaviour. This was demonstrated in the independent regulation of the RR intervals (chronotropy) and the corresponding QT subintervals (inotropy), as the former defines the rate of contraction and the latter has a linear negative correlation with the peak pressure inside the contracting ventricular muscles. During accumulating ischemia/anoxia, dimensional fluctuations of the two sub-interval series as correlates of adaptation-dependent self-organization and reorganization in the underlying intrinsic cardiac nervous system, was seen. COVID-19 and Allostasis As we know, organs exposed to the outside world, such as the digestive and respiratory tracts and skin have a high functional immune component, which acts as an interface and barrier to external pathogens. At the outset of this pandemic, COVID-19 was considered a lung condition. However, as time went on, hypoxia and diffusion issues began to be noted, including oxygen blood saturation levels of 50%, skin changes in the periphery (esp toes) resembling lesions seen in chilblains and chicken pox, notably in young people (20-40 years of age). Additionally, vascular clotting began to be seen in this younger population leading in some cases to stroke. Furthermore, longer gastric emptying was seen which may or may not be an immune response. It has also been noted that it's highly contagious, human to human, animal to human and human to animal, as well as being highly unpredictable, in who survives and who does not. Since it is a 'novel corona virus' we do know that we need our 'innate immune response' to fight it. That's potentially why it generally doesn't affect children (however there have been exceptions) and it's mortality rate is much higher amongst the elderly and those who are already metabolically or immune compromised. Furthermore, psychological stress from confinement has also been seen. Further mental health issues, from potentially the extreme viral exposure amongst essential services, and/or extreme exhaustion amongst health care workers has also been acknowledged. Psychology and mental stress, such as that from Post Traumatic Stress Disorder (PTSD) is thought to reduce the number of naive T cells, meaning a reduced ability to launch an immune response to a novel pathogen and is also thought to contribute to increased susceptibility to auto-immune disorders (Dr. Annette Sommershof). Therefore, the essential question, is it purely metabolic and cognitive exhaustion, and/or exhaustion of the immune system from exposure to COVID-19? Would people (orienteers) used to mental stress, whilst exercising, better be able to launch a balanced immune defence? Adaptation has a damping mechanism whereas lack of adaptation does not. Additionally, it is important to launch a stimulus or perturbation strong enough to activate an appropriate balanced response. Recovery and sleep routine It is critical to maintain a healthy sleep pattern if we wish to maintain a healthy immune system. Routines of the day can become good anchor points for the body. These include eating regularly and sleep. Psychology of the immune state Psychologically, we also need to be prepared for what lies ahead. Currently, we're fighting an unknown assailant. A virus which our adaptive immune system has never seen before. This means that we must rely on our innate immune system, the one we're born with, to adapt it's RNA to a DNA antigen which can fight the disease. However, remember psychological stress of 'perceived dangers' such as job and income insecurity, fear of the disease, isolation and loneliness can affect where and when we deploy our cytokines. Importantly, when or if we are exposed to COVID-19, ideally your immune system is able to react and isn't already exhausted. Part of your exercise regime may need to include meditation and Yoga. Diet Another, important way of avoiding an 'exhausted immune system' is diet. Generally, a well balanced diet is important. Moreover, during exercise our immune system is enhance, whereas post exercise it can be depressed. One of the best ways to ameliorate this, is through amelioration of metabolic demands with pre-exercise, during long exercise and/or immediate, post exercise calorific intake, thereby avoiding metabolic imbalance and potential catabolic (break down) reactions, whilst promoting anabolic (building) ones. Besides nitrogen balance, contracting skeletal muscles, in sports such as running, are a major source of increases in the circulating concentration of the cytokine, Interleukin-6 (IL-6), seen during exercise. It's appearance decreases with the ingestion of glucose and with endurance training. Low pre-exercise glucose levels, results in greater transcriptional activity of IL-6 gene in muscle and higher IL-6 concentrations during subsequent exercise, which in turn stimulates hepatic glucose production and fatty acid mobilisation and oxidation. Thus, IL-6 may be a carbohydrate sensor, mobilizing substrates and/or augmenting substrate delivery to working muscles. Interestingly, IL-6 concentrations increased with increasing intensity of exercise, whereas tumour necrosing factor alpha (TNFα) did not (Scott et al 2011, Med & Sc Sp & Ex, 43,12, 2297-2306), suggesting a specific and therefore potentially finely tuned immune response. The gut-muscle-immune axis: a ratio of innate and adaptive immune substances? It could be simply argued that all systems are oscillatory, finely tuned through damping mechanisms and that the reference points of the tuning are not only defined by extent of the oscillation (linear dynamics) but also by the randomness of non-cycling oscillations. Mechanically, this may be analogous to a mass-spring system defined by Hooke's Law, but immunologically it's potentially defined by the balance between up-regulatory and down-regulatory immune pathways of the adaptive and innate systems? https://phys.org/news/2016-03-gut-microbiome-remarkably-stable.html Using a yeast and bacteria (E.coli Hsp60 homologue known as GroEL) model, a tenuous relationship has been proposed between HSP60 and HSP70 chaperone proteins, as they are both vital for mitochondrial proteostasis, being involved in the import and/or the folding of almost 50% of the mitochondrial proteins. Moreover, both proteins were found to carry out various functions via interaction with a large number of extra-mitochondrial complexes. In the case of HSP 70, its mitochondrial functions are performed by the classical mechanism known for all HSP 70, utilising a protein and a nucleotide exchange factor. With regard to mitochondrial HSP 60 and HSP 10, it is notable that this pair developed a unique reaction cycle in the gut (Jebara F et al 2017 DOI: 10.1002/9780470015902.a0027152), a bit like the relationship of HSP27 with HSP72. The amount of human DNA is totally under-whelming compared to that of the intestinal mircobiome. The intestine is composed of a complex ecosystem of more than trillions of bacteria, viruses, fungi, Protozoa and Archea that live in a symbiosis with the host in the gut lumen. The healthy microbiome include a limited number of highly represented taxa, such as Bacteroides and Prevotella and a large number (>2000 to date) of minor players with low representation but high metabolic activity. These latter 'players' with high metabolic activity are likely to be the ones which interact with the musculoskeletal system. In older age, species richness and diversity of the microbiome decline, inter-individual variability increases, and resilience to perturbations are reduced. Apart from aging, the presence of acute and chronic diseases affects the microbiome. In the aging and/or unhealthy microbiome a 'dysbiosis' can occur, where a disruption of the gut balance 'symbiosis' results in intestinal permeability, allowing bacteria, or bacterial toxins and metabolites to enter the host circulation thereby promoting sub-clinical inflammation. Clinically, sub-clinical inflammation has been referred to as 'inflammaging' and 'immunosenescence'. All components of the innate immune system exhibit profound changes during aging. Monocytes are classified into three subtypes: classical, non-classical, and intermediate. During aging the number of nonclassical CD14+CD16+ monocytes increases, indicating a shift to senescence, proinflammatory phenotype with short telomeres. Similarly, a shift in macrophages from immunoregulatory M2 macrophages to proinflammatory M1 macrophages. Furthermore, Natural Killer (NK) cells are innate lymphoid cells, where 2 subtypes are present. CD56bright cells are immature cells providing an immune regulatory function, and CD56dimCD16+NK cells which produce high levels of IFN-gamma, associated with a potential dysregulated cytokine production, as CD56bright cells decrease with aging. Moreover, exercise appears to have the opposite effect to aging, where a reduction the number of nonclassical CD14+/CD16+ monocytes, was found, in a 12 week combined strength and endurance training program. The adaptive immune system changes with aging. Although the total number of T-cells remains constant throughout life, the two main cellular subtypes CD8+ cells increase, whereas CD4+ decrease. This phenomenon is part of the immune risk profile (IRP) and indicates immunosuppression in certain diseases. Reduction of naive CD4+ cells is driven by thymic involution from chronic antigenic stimulation and inflammation. Inflammaging chronically increases IL-6 and TNF-alpha. Improved T cell function has been reported in elderly runners who trained for an average of 17 years, and thus improvements in the adaptive immune response. In 102 male participants between 18 and 61 years of age, with above-average VO2 had fewer senescent CD28-CD57+, CD4+, and CD8+ cells and increased number of naive CD8+ T cells. Acute bouts of exercise induces cell death in apoptosis-resistant senescent T-cells. Additionally, regular endurance training in the elderly, improves CD4+/CD8+ ratio. Although exercise seems to improve the immune system, endurance exercise seems better than strength training alone. Exercise also influences inflammation induced from visceral adipose tissue (fat). Toll-like receptors (TLRs), mainly in the innate immune system, are upregulated with physical inactivity, systemic inflammation and the development of age-related diseases. They are particularly reactive to heat shock proteins (HSP). HSP's are found in muscle and released with exercise. Conversely, a reduced expression of TLR2 and TLR4 has been found in both acute and regular exercise. Importantly, skeletal muscle itself acts as an endocrine organ, whereby muscle contractions and energy metabolism induce the production of various cytokines-termed myokines-or peptides with anti-inflammatory potential. As highlighted earlier IL-6 is one of the most effective myokine. IL-6 increases during and after exercise, proportional to intensity and duration, stimulating immune-regulatory mediators such as IL-10 and the IL-1 receptor antagonists and downregulation of TNF-alpha by monocytes and macrophages. Results form middle-aged master athletes demonstrated that IL-1ra, IL-1beta, IL-4 and IL-8 levels were elevated compared to inactive, younger-middle-aged controls. Exercise-induced IL-6 has been shown to inhibit endotoxic-induced TNF-alpha. Besides IL-6, myokines such as meteorin-like has been shown to induce brown fat metabolism, increase IL-4 levels and promote polarization of M2 macrophages. IL-7 and IL-15 are myokines that might stimulate lymphocyte proliferation and it has been suggested that IL-7 exerts protective effects on the thymus.. IL-15 seems to have further effects on immune homeostasis which induces a better survival rate of naive T-cells. At a metabolic level, IL-15 reduces the accumulation of visceral and white adipose tissue by reducing the accumulation of fat. Exercise is generally considered a positive modulator of the gut biome. Regardless of age, exercise has a positive effect on taxa involved in energy, carbohydrate and protein metabolism and short chain fatty acid (SCFA) production. Maintenance of exercise is needed to induce long-lasting modifications of intestinal microbial ecosystem. Such changes have been shown to improve the inflammatory mediators of the gut. Importantly, dosage of exercise is important, as over-exercise can induce ischaemic events in the gut mucosa, associated with acute gastrointestinal symptoms including abdominal pain, nausea, and diarrhoea. Supplementations, of probiotics and prebiotics can attenuate some of these unfavourable changes of the gut. Probiotics have been shown to modify the gut microflora population, increase natural killer (NK) cell cytotoxicity, increase secretary immunoglobulin A (IgA) levels, and enhance resistance to infections, potentially through the kynurenine/tryptophan ratio, activated T-suppressor (CD8+CD25+) and natural killer cells (CD56+CD16+) in high doses, whilst low doses increased activated T-helper lymphocytes (CD4+CD25+), B-lymphocytes (CD19+) and antigen-presenting cells (HLA-DR+). There is a gut-muscle axis hypothesis in age-related sarcopenia. A dysbiotic intestinal microbiota can effectively result in reduced bio-availability of dietary proteins, in particular tryptophan, which is a powerful mediator of inflammation, as well as a promotor of muscle protein synthesis. Additionally, the gut bacteria are also involved in the synthesis of many vitamins, including folate, vitamin B12 and riboflavin, which exert pro-anabolic effects on muscles. Tryptophan is a pre-curser of serotonin and plays a pivotal role in immune system regulation. Enhanced breakdown of the tryptophan kynurenine pathway occurs in aging and in conditions with an increased pro-inflammatory response. Tryptophan and particular serotonin have been known to be associated with mood and cognition. The kynurenine pathway not only plays a role in the innate immune system via IDO (an enzyme which degrades tryptophane) and it's influence on IFN-gamma, but also in the adaptive T-cells immune response, through selective apoptosis of Th1, and not Th2, cells. Accumulating evidence implicates gut microbiota in the regulation of kynurenine pathway metabolism, and thus the gut-brain axis. Chronic exercise interventions may lead to reductions in IDO activity as a result of anti-inflammation. Assuming that chronic inflammation induces sarcopenia and vice versa, good muscle mass reduces chronic inflammation, a vicious cycle needs to be broken by any means possible, through a combination of dose specific exercise and diet. As already stated anti-oxidants and sufficient carbohydrates and protein are important in our diets. Additionally, n-3 polyunsaturated fatty acids (PUFAs), has been shown to have anti-inflammatory properties through their effect on leukocyte action, eicosanoid production, and T-cell proliferation. PUFAs in combination with strength and endurance training have been shown to have favourable muscle building effects, where 6 months of Progressive Resistance Training (PRE) (2 x week, 3 sets per x's. 50-85% 1RM) combined with n-3-PUFA-rich diet, improved gene expression, whereby pro-inflammatory IL-1beta was down-regulated and regulator of cellular growth mechanistic Target of Rapamycin (mTOR) was up-regulated in skeletal muscle in older women. Exercise training has been shown to reduce intestinal inflammation and modulate gut microbiota profiles in insulin-resistant people (Motiani et al 2020, Med Sc Sp Ex, 52, 1, 94-104), using both moderate-intensity continuous training (MICT) and sprint interval training (SIT). High fat diets reduces the Bifidobacterium, Eubactterium rectale-Blautina coccoides, and Bacteroides genus which leads to an increase in the Gram-negative : Gram positive ratio, meaning a subsequent increase in LBP was found by Cani et al (2008 Diabetes, 57, 6, 1470-1481). Moliani et al (2020), on the other hand, found the opposite with both forms of exercise training. There was a reduction in Firmicutes/Bactroidetes ratio, mainly due to an increase in the relative abundance of Bacteroidetes and a decrease in abundance of Blautia spp. and Clostridium spp at genus level. This may induce regulatory T-cells to produce IL-10 (anit-inflammatory cytokine) inside the gut (Mazmaniian et al 2008 Nature, 453, 7195, 620-625). Furthermore, it was found that Bacteroidetes at the species level correlated negatively with plasma inflammation (LBP, TNF alpha, and CRP levels) (Moliani et al (2020). Exercise training also reduced the relative abundance of Clostridium and tended to reduce the Blautia genus. The former thought to play a role in whole body inflammatory response and the latter found in abundance in pre-diabetic people. Moliani et al (2020) also found a reduction in TNF alpha after 2 weeks of training, which also plays a critical role in inflammation. The Firmicutes/Bacteroidetes ratio is elevated in obese people, whereas it is reduced in this study as well as in some investigations examining dietary intervention.(Ley ey al 2006 Nature, 444, 7122, 1022-3)..It is thought this ratio is important in that Firmicutes may contribute to obesity because they can harvest more energy from food (Turnbaugh et al 2008, Cell Host Microbe, 3, 4 213-223). Increases in faecal Bacteroidetes were also found, which is significant as it plays an essential role in the metabolic conversions of complex sugar polymers and degradation of proteins (Rajilic-Stojanovic & Voss 2014, FEMS Micorbiol Rev, 38, 5, 996-1047). Although, these are very positive findings for exercise intervention, chaos theory would suggest that the SIT group should have shown more changes than the MICT group. Interestingly, by choosing a cycling program, any effect of muscle micro-tears and an immune response is mitigated, as would be seen with eccentric exercises, such as a running regime. Hence, this is a purely metabolic (vs mechanical load) load, where the SIT is high intensity but of a much shorter duration (30secs x 4-6 bouts) vs MICT of 40 - 60 minute duration. One would surely elicit an anaerobic, lactic acid, response whilst the latter would elicit a Glut-4 muscle energy metabolising response. It's difficult to reconcile this on a purely metabolic basis and perhaps it's the neural activation of exercise which is the prime signalling pathway? The Paper of the Year for Exercise and Sports Science (2020) was recognised for several findings, including exercise alters the microbiome of the gut independently of diet exercise exerts strain level selection for microbes within the host more robustly than genotype reduced exercise tolerance in situations of reduced microbiome (eg anti-biotic use and gene knock out mice) mechanism is likely via butyrate-producing microbes gut-immune interactions via gut-associated-lymphoid tissue bile acid circulation metabolic flux Specifically, Fecalibacterium prausnitzii, has been shown, not only to be enhanced with exercise training, it is thought to improve type II diabetes outcomes, as well as improve symptoms of depression and anxiety. (Mailing et al 2019, Ex Sp Sc Rev, 47, 75-85. Weyh C et al (2020), Nutrients, 12, 622: doi:10.3390/nu12030622 Ticinesi A et al (2019) EIR 25, 84-95 Ticinesi A et al (2019) Nutrients, 11, 1633; doi:10.3390/nu11071633 Codella et al (2017), Digestive and Liver Disease, doi:10.1016/j.dld.2017.11.016 Dietert R & Dietert J (2012), Entropy, 14, 2036-2065: doi:10.3390/e14112036 COVID-19 is not just in the lungs - it's also in the gut. Bursitis, tendinopathy and the immune system Clinically, I began to notice a relationship between bursitis, tendinopathy and gut immune compromise back in the early 1990's when I was working with Swiss elite national teams in various sporting endeavours. It seemed like a common occurrence for young healthy athletes to suddenly develop bursa and tendon symptoms after a gut infection, severe cold, etc. Since that time, many investigations have demonstrated a relationship between metabolic-immune compromise and fatty-immune substance infiltration into bursa and tendon resulting in pain. Interested readers should see shoulder tendinopathy elsewhere on this website for further details. Dosage of exercise to fine tune the immune system Hence, dosage and type of exercise becomes important as well as the way you progress your loading. The benefit of resistance training, is that you can do this indoors, using weights around the house, as well as body weight. Additionally, it is easy and important to establish a base line. That is, how many repetitions for a certain number of sets. Each set of repetitions should feel the same in each set. The last repetition is the 'point of failure' ie you cannot do another repetition. You will also need to establish the time of recovery between sets. Write these down. Once a base line or a protective foundation of exercise has been laid down, using a deterministic chaotic variable (usually 4-12 weeks), then the introduction of random - chaotic - novel exercise, fine motor exercise, high repetition exercise, high load low repetition needs to be employed, to improve cognitive, metabolic, emotional, mechanical and ultimately immunological demand on the system. Those fortunate enough to be able to leave their home for exercise, walking and cycling are great activities. Even here, you can challenge yourself with distance, time and hills. If walking, you may wish to use a weighted backpack. If cycling, use higher gears from time to time, so as to add some resistance training into what is essentially an endurance activity. However, these activities do not replace a structured home exercise or gym based regime. Oscillations in another part of the body can be used to establish harmonic frequency elsewhere. For example, arm movements activating the opposite erector spinae activity, pelvic oscillations for scapular control, arm lifts for contra-lateral gluteal activity. Alternate kneading of the hands into something soft activates the abdominal muscles, spinal rotatores and scapula muscles. Oscillations of the pelvis around the hip activates eccentric scapula control. Alternate lifting of the arm off the wall activates the opposite buttock muscle. Alternating arm flexion/extension around the 90 degree angle activates the opposite erector spinae muscles of the low thorax and upper lumbar spine. Moving through the horizontal with a consistent oscillation also has varying effects on those muscles. Importantly, if loading is required to activate a muscle building response, then repetitions need to include tremor. Either fine motor tremor or exhaustion tremor, if we want to include a 'deterministic chaotic variable', which it is hypothesised to create an immune training variable. "In this regard, it is vitally important that we try to maintain our activity levels within recommended guidelines. Not only can exercise have a positive direct effect on the cells and molecules of the immune system, but it is also known to counter the negative effects of isolation and confinement stress on various aspects of immunity. Although no scientific data currently exists regarding the effects of exercise on coronaviruses, there is evidence that exercise can protect the host from many other viral infections including influenza, rhinovirus (another cause of the common cold) and herpesviruses such as Epstein-Barr (EBV), varicella-zoster (VZV) and herpes-simplex-virus-1 (HSV-1). Work from Jeff Woods’ lab at the University of Illinois showed that moderate-intensity exercise training during an active influenza infection protected mice from death. It also promoted a favourable immune cell composition and cytokine shift in the lungs that was associated with prolonged survival. A major focus of our research is to understand how exercise can mitigate the negative effects of stress to maintain immune function, particularly during prolonged periods of isolation and confinement such as space travel. We showed recently that astronauts who had higher pre-flight cardiorespiratory fitness and skeletal muscle endurance before a six-month mission to the International Space Station were less likely to reactivate EBV and VZV during the mission. Copies of EBV viral DNA were also lower in the fitter astronauts, indicating that their ability to infect others is also reduced. Moreover, those astronauts who had lower pre-flight fitness levels and returned to Earth with the greatest levels of cardiorespiratory deconditioning were more likely to have reactivated a virus during the mission. Viral reactivation is a global indicator that our immune system has been weakened, which, in this context, we believe to be largely due to the stressors associated with isolation and confinement. This research indicates that exercise, in addition to the aforementioned direct effects it can have on cells and molecules of the immune system, may be an effective stress-induced countermeasure to help maintain immune function and lower infection risk." (Richard J. Simpson, Ph.D., FACSM | Mar 30, 2020) "Floppies vs Stiffies" consideration when prescribing exercise There are essentially two types of people - the 'floppies' vs 'stiffies'. The forming are hyper-mobile whereas the latter are hypo-mobile. The floppies like to do fast and quick type of exercise such as gymnastics, dance, track and field, etc. The stiffies tend to do slow type of exercise such as marathon running. Hence, not only do these people have different connective tissue type, but also different muscle fibre type. The 'fast' twitch muscles are the ballistic muscles, whereas the stiffies tend to have 'slow' twitch endurance muscles with a joint and posture stabilising function. Stiffies tend to be found in the Pilates class, whilst the floppies are found in the Yoga class. In terms of clinical reasoning and injury management this should probably be the other way around. Another, interesting clinical anecdotal observation, floppies tend to do better in pulling type of exercise ie where energy is brought back into the body, whereas stiffies tend to do better with pushing type of exercise where energy is produced outward away from the body. Motivators to exercise and to eat Interestingly, research which I undertook in 1992-93, examined the influence of the hypothalamus and the peripheral sympathetic nervous system on fibromyalgia, chronically over-exercised and repeatedly injured female elite athletes. What was exceedingly interesting were the interactions with luteinising and follicle stimulating hormone and immune system. Clinically, these athletes (orienteers, x-country skiers and distance runners) suffered from eating disorders, osteoporosis, dysmenorrhea, late menarche, and were frequently ill with skin infections and upper respiratory infections. Paucity of research on the hypothalamus, at the time and even contemporarily in humans, due to the technical nature of research in this region, means that the majority of investigations are still done in rodents. More recently, leptin, glucose and glut-2 astrocyte and neuron (related to glut-4 muscle) receptors, and neuropeptide Y (NPY) were found to be involved in a complex interaction around the arcuate nucleus (ARC), related to transcriptional regulation of motivated exercise (Good et al 2020, Ex Sp Sc Rev, 48, 2, 74-82). These areas happen to be also related to taste and smell (olfaction), which coincidentally the loss of, is one of the symptoms related to COVID-19. The olfactory system has been used as a conduit for drug and homeopathic administration, directly into the central nervous system (CNS), as there is no blood brain barrier or blood nerve barrier here. New genetically engineered biotechnology products, such as recombinant human nerve growth factor, human VEGF, and interferons, are now possible to be delivered into the brain from the non-invasive intranasal route. For gene therapy, intranasal route is also a promising alternative method to deliver plasmid DNA to the brain. Additionally, anti-biotics are also being trialled via nasal delivery in COVID-19 patients. Insulin nasal delivery has also been approved by the FDA using a methodology originally developed by (my uncle-in-law) Eric Bechgaard of Denmark (https://www.sciencedirect.com/science/article/pii/0378517395043152), Interested readers of this modality should see https://www.ncbi.nlm.nih.gov/pubmed/21712015 for a review.. It would appear that the same area of the brain relating to eating is also related to initiation or continuation of exercise, at least in rodents. Leptin levels are reduced 1-3 hours after exercise such as running (Zheng et al 1996, Biochem biophys Res Commun, 225, 3, 747-750). In rodents, injecting an expression vector for Leptin receptors increased home cage activity . A wild type mouse had significant reduction in weight using a similar methodology (Coppari et al 2005, Cell Metabol, 1,1, 63-72). Furthermore, it's not just a simple glucose or leptin-sensing mechanism by hypothalamic neurones, but a series of inter-connecting neurones, astrocytes, integrated receptors, adenosine triphospahate (ATP) synthesis and sodium sensing within the brain. Importantly, however, these incredibly complex, areas may also exert an influence, directly or indirectly, on the immune-inflammatory axis, through it's action on muscles, which affects overall health and susceptibility to disease. Importantly, a (un)healthy relationship exists between weight and susceptibility to disease. The review by Good et al (2020) stipulates that it's the flux of leptin, rather than the absolute levels of leptin, which is sensed by the LepR POMC neurones, whereby an increase in leptin levels may signal the need to exercise, so as to remove excess available energy. Specifically, transcriptional gene regulation downstream of the neuronal basic helix-loop-helix transcription factor nascent helix-loop-helix transcription factor nascent-loop-helix 2 (NHLH2/humans, Nhlh2/mouse) in POMC neurones, drives motivation to exercise by increasing melanocortinergic and dopaminergic tone in the hypothalamus and extrahypothalamic brain regions. Leptin, diabetes and exercise Researchers, using a diabetic mouse model, have demonstrated that decreased leptin, MCP-1, and resistin levels were observed in diabetic mice after moderate exercise training compared with the non-exercised group. Leptin, MCP-1, and resistin levels in diabetic mice+Ex mice were 8.6, 75, and 39% lower, respectively, compared with diabetic mice without exercise training (Liu & Chang 2018, Front Physiol. 9, 636). Monocyte chemoattractant protein-1 (MCP-1/CCL2) is one of the key chemokines that regulate migration and infiltration of monocytes/macrophages. Both CCL2 and its receptor CCR2 have been demonstrated to be induced and involved in various diseases, including fibrosis, arthrosclerosis and systemic inflammation such as psoriasis. Migration of monocytes from the blood stream across the vascular endothelium is required for routine immunological surveillance of tissues, as well as in response to inflammation. Moreover, a metabolic role involves adipocytes secreting various adipokines that may be involved in the negative cross-talk between adipose tissue and skeletal muscle. CCL2 impairs insulin signalling in skeletal muscle cells via ERK1/2 activation at doses similar to its physiological plasma concentrations (200 pg/mL), but interestingly, does not involve activation of the NF-κB pathway. CCL2 significantly reduced insulin-stimulated glucose uptake in myocytes. CCL2 may represent a molecular link in the negative cross-talk between adipose tissue and skeletal muscle assigning a completely novel important role to CCL2 besides inflammation (Sell H et al 2006 Endocrinology. 147, 5, 2458–67Endocrinology. 147, 5, 2458–67). Leptin and diet The first time I heard about leptin was in the mid 90's and it was described as a hormone produced by fat cells. Certain foods stimulate leptin sensitivity (vs leptin resistance and weight gain). These include Apples. Research has shown pectin—as found in apples—may be effective in fighting back leptin resistance. Oatmeal. Rich in fibre and known for decreasing insulin levels, oatmeal can help prevent that “starving” feeling. Lean proteins. The protein you get in turkey, chicken, and other lean meats can help to raise your metabolism and reduce leptin resistance. The same with fish, a top choice for battling leptin resistance. Green tea. A European study involving mice showed that green tea is effective in decreasing leptin resistance. Almonds. Besides the essential “healthy” fats, fibre, and protein you get from almonds, you also get essential fatty acids that boost metabolism and leptin sensitivity. Broccoli. Also thought to decrease your leptin resistance is broccoli, a vegetable that’s generous in calcium and vitamin C. Eggs. Known for their vitamin B12 and protein contributions, eggs can lift your metabolism and help keep you from becoming leptin-resistant. Generally speaking, keep fruits and vegetables front and centre at your meals. Top choices: grapefruit, watermelon, pears, and blueberries along with purple sweet potatoes, peppers, lettuce, carrots, and zucchini. Exposure "Currently, the greatest risk of COVID-19 infection is exposure. It is paramount that we find creative ways to exercise while maintaining social distancing and proper hygienic countermeasures. While exercise may not prevent us from becoming infected if exposed, it is likely that keeping active will boost our immune system to help minimize the deleterious effects of the virus, ameliorate our symptoms, expedite our recovery times and lower the likelihood that we can infect others with whom we come into contact. This is merely my intuition, but I do expect a large body of exercise immunology research to follow after this pandemic so that we can provide more specific exercise recommendations as they pertain to infection risk and control in both healthy and clinical populations." (Richard J. Simpson, Ph.D., FACSM Mar 30, 2020) Low Back Pain, lumbo-pelvic movements and sample entropy An interesting article was published in 2022. For many years, it has been observed that people with chronic low back pain (LBP) have less perturbations of movement. There was the famous investigation in the 1980's, where people standing still with a WW1 German spiked helmet on their head, seemed to sway less when suffering chronic LBP. Clinically, it has been observed that chronic LBP is frequently associated with loss of ranges of motion (degrees of freedom). Thiry P et al (2022, Entropy, 24, 437, https://doi.org/10.3390/e24040437) demonstrated lack of randomness (entropy), of lumbo-pelvic movements, in a 70 seconds 'touch the stool' test, in people with LBP. Moreover, this lack of variability can persist, even after the cessation of LBP. It is thought that this smaller amplitude and less variability of the instantaneous centre of rotation results in a potential overloading of certain structures and underloading of others, creating disuse atrophy or overuse trauma. So, in the presence of CLBP, the aims of therapy would be to ascertain movement restrictions, ameliorate those, introduce oscillatory mobilisations and exercise techniques with increasing amplitude, displacement and ultimately variability. Musculoskeletal Physiotherapy in the recovery from injury Previously, we discussed game theory in terms of adding resources to the VMO through FES (functional electrical stimulation) to moderate anterior knee pain and regain quadriceps cortical representation and function. We also described the need to stress the system to induce the change needed to improve immune health. Those stressors may, if they cross the threshold from functional to dysfunctional at times, need to be managed,. The latter inducing pain, which if it persists, results in clinical or sub-clinical inflammation, thereby creating an immune compromised states. Obvious everyday signs of this are frailty and obesity. Clinically, traditional Manipulative Physiotherapy (now called Musculoskeletal Physiotherapy) used a multitude of questions from the cognitive domain to ascertain a persons dysfunction. Parameters included the stage (temporal), stability (current or past history of ease of recurrence), irritability (time to worsen vs time to ease) and severity (how disabling). Intrinsic to questioning, was establishing a persons normal baseline of activity w.r.t. their age and wellness level, and calibrating that degree pf loading to questions on the triggers of their pain and dysfunction. Multidimensional reasoning on ascertaining perturbations or 'outliers' to an expectation of this persons and the average persons functional capacity, health and physical as well as mental well being. Once, these 'outliers' are correlated into a clinical picture, a reductionist approach to treatment, exercise prescription and goal setting can be achieved within the construct of the persons expectations, values and beliefs. The 'outliers' of the subjective examination are correlated with the 'outliers' of the physical examination. For clinicians, the 'noise' is the average, the 'fidelity' are the answers we receive from the inductive and deductive reasoning. Knowledge is strength. Physiotherapists, Exercise and Sports Scientists, Team managers and Trainers should have the confidence in their construct validity by incorporating their knowledge of the immune system, 'outliers', game theory and deterministic chaos into their treatment, rehabilitation, training regimes and sporting strategies, using a multi-modal reasoning approach. Conclusion Does exercise create a chaotic environment which stimulates and tunes the immune system? I have argued that it does, based on the muscle itself being an endocrine organ, in which multiple immune reactions occur and from which there is an interaction with multiple organs, including the brain, gut, thymus and liver. Additionally, intrinsic to exercise is the use of the lungs, which in essence is an immune interface with pathogens from the outside world. Where does chaos fit in? Chaos could be considered the non-harmonic perturbations of an oscillatory or regulatory system. A system of ratios, higher 'fidelity' as the magnification of the ratios, where perturbations of cytokines creates oscillations and new states of homeostasis through modal jumps. These oscillatory systems also include those of the second law of thermodynamics, motor and metabolic control. Paradoxes exist which allow the seemingly random fluctuation of a homeostatic system. Exercise can be deemed to be an easy tool for us to use in order to push the boundaries of these fluctuations, in order to set the reference points for a dynamic damping mechanism. The greater the fluctuation, the greater the damping needed. Importantly, in any damping system, over-shooting and over-oscillating need greater damping, which could include sound professional advice from physiotherapists and trainers. This may include advice on types of training (eccentric vs concentric, metabolic ), rest, avoidance of over-training, good and varied diet as well as mental strategies for a calm cognitive - psychological state are of paramount importance in the application and dampening of stressors. Moreover, hands on therapy may be required if injury were to occur. Most importantly, exercise can be seen to stimulate muscle, one of the largest organs of the immune system. In such a sense, prophylactic exercising of muscles, makes this strategy an inoculation against immune challenges both now and in the future. In this age of COVID-19, a great opportunity has arisen where people working from home may more easily exercise. Moreover, whilst in shut down it is even more important to exercise, and if the possibility arises walk, run or ride to work, thereby incorporating exercise and deterministic chaos into your daily routine, whilst avoiding confined spaces such as public transport. However, bear in mind that the trip to work shouldn't be exhaustive, as that can lead to immune compromise, for several hours after the cessation of exercise. Justification This article was adapted from a key note guest presentation I made at a conference in Rome in 2005, as well as Post Graduate research on neuro-immune-inflammation in Low Back Pain from 1995, an under-graduate research topic on Bernsteins perspective of motor control and linear oscillatory systems to control degrees of freedom from 1986, inverse dynamics and the Hill model of the mass-spring spring cycle and thermodynamics in calf-achilles problems from 2008, and research into Orienteering on a motor-immune-cognitive control hypothesis from 1998, as well as reading on non-linear dynamics and chaos since 1992. I wrote it, in response to the pandemic, but also as a conceptual framework on which I wish people build deterministic chaos theory into their reasons for motivation to train the mental and physical well being. Hopefully, physiotherapeutic interventions incorporate game theory of 'doves & hawks' into their thinking whilst, bearing in mind that muscle is an endocrine organ of the immune system, with a gut, lung and brain axis. Stay well, stay safe, support yourself, your family and your community Martin Krause April - May 2020 References References can be found within this text and in the original papers published in 1986, 1995, 1998, 2003, 2005 and 2008 and found here elsewhere on this site : - Sarcopenia and the immune system : https://www.back-in-business-physiotherapy.com/we-treat/exercise-muscle-mass.html - Pain and inflammation : https://www.back-in-business-physiotherapy.com/pain-and-inflammation.html - Inverse Dynamics and Hill model of mass spring system : https://www.back-in-business-physiotherapy.com/we-treat/achilles-tendonosis.html - Degrees of freedom and Bernsteins concept of motor control using a linear oscillatory system : https://www.back-in-business-physiotherapy.com/shoulder.html - Orienteering, motor control and the immune system (uncontrolled manifold hypothesis) : https://www.back-in-business-physiotherapy.com/sports-performance/orienteering.html - Endurance Training : https://www.back-in-business-physiotherapy.com/endurance-training.html Uploaded : 3 April 2020 Updated : 4 August 2022 Read More -

Rotator Cuff Injuries
Rotator Cuff Blogg Hey everyone! This month’s blog focuses on the shoulder, more specifically the rotator cuff muscles and some common conditions we regularly treat here at Back in Business Physiotherapy. The shoulder is one of the most common regions of the body that we treat. One of the main reasons the shoulder gets injured is that it’s a super mobile joint. It is the most movable joint in the body in fact! In order to have so much mobility, the joint has to sacrifice stability, and the lack of stability in the shoulder leaves it susceptible to injury. Efficient movement in the shoulder largely relies on the proper functioning of the rotator cuff muscles. Read on to find out what they are, what they do, and what can sometimes go wrong with them. What is the rotator cuff? The rotator cuff is a group of four muscles – the Supraspinatus, Infraspinatus, Teres Minor and Sub-scapularis. If you have trouble remembering the names, just think ‘SITS’. Easy-peasy! Each muscle at-taches from the shoulder blade (scapula) to the arm bone (humerus) and has a specific function to play in shoulder movement. What does it do? In a nutshell, the supraspinatus helps to take the arm away from the body (abduction), the infraspinatus and teres minor help to rotate the arm outwards (external rotation), and the subscapularis helps to rotate the arm inwards (internal rotation… Other muscles also help with these movements too). Collectively, the four muscles work together to keep the ‘ball’ of the arm bone centred over the ‘socket’ of the shoulder blade. By doing this, it allows us to have a relatively free and large range of motion in the shoulder in all directions of movement. But remember, lots of mobility is only achievable by sacrificing stability, and this is where the shoulder and rotator cuff sometimes come unstuck. Common conditions Here is a brief overview of some common rotator cuff disorders: • Rotator cuff tendon injury: Who remembers what tendons do? We’ll give you a clue… They at-tach muscles to bones. A tendon may become injured acutely (known as tendinitis) or in a chron-ic way through degeneration (known as tendinopathy). This commonly occurs due to impact to the shoulder or through repetitive movements as seen with throwing sports in the initial stages. If the movements continue over a long period of time and healing doesn’t occur fully, the tendon tissue can degenerate, leading to tendinopathy. • Rotator cuff tear: If the above process continues over an even longer time period, the tendon will degenerate more and eventually it may reach a point where the tendon tears. This can cause significant loss of movement and pain with shoulder movements. • Subacromial impingement: Between the ball of the arm bone and the tip of the shoulder (a.k.a The acromion) sits a small space called the subacromial space. Several structures run through this very small space, including the tendon of the supraspinatus and part of the biceps muscle. There is also a fluid filled sac called the subacromial bursa which helps to keep movement smooth in the shoulder joint. Repetitive movements can lead to any of these structures becoming irritated and inflamed, making an already small space even smaller. The shoulder then cannot function to its full movement capability and movement becomes painful. Rotator cuff tendinitis is one cause of subacromial impingement. All of the above conditions share some common signs and symptoms. The main symptom experienced is pain with shoulder movement, particularly when raising the arm above the head, in front or out to the side of the body. Acute tendinitis, chronic tendinopathy and a tear can all lead to weakness during shoulder movements, although weakness associated with a tear is usually more severe. You may also experience pain when lying on the affected shoulder at night-time. Sometimes it can be difficult to determine from the outset what condition is developing, but we will make an informed decision based on the information you give us and what signs and symptoms you have when we assess you. Treatment All of the above conditions can be managed well with manual treatment and exercise. With the exception of severe tears, which may need a shoulder specialist/surgical opinion if the injury doesn’t respond well to conservative treatment, rotator cuff injury is commonly managed from start to finish by us here at Back in Business Physiotherapy, so always come to us as a first port of call. Acute injuries will always need time for the body to deal with the inflammation that has occurred. Then a combination of massage, shoulder and spinal joint mobilisation and mobility and strengthening exercises are what is required to get over these painful conditions. The exercise program will start simple and grad-ually progress over time; it aims to return the muscle and tendon to full strength, as well as re-train efficient shoulder and spinal movements that may have been lost during the injury process. We may decide to use other treatment techniques including taping, needling under guided ultrasound, therapeutic ultrasound to aid in the healing process. Most rotator cuff injuries respond very well to manual treatment. Even small tears can be well managed this way. If you have shoulder pain and need some help, please get in touch today, so we can get you back on the dancefloor, shimmying to your heart’s content! Uploaded : 1 April 2020 Read More -

Family stress during the time of COVID-19
Managing stress as a multitasking mother in the time of COVID-19 Are you a working mum? Or perhaps a full-time mum trying to manage kids, a house and everything that comes with it? Or maybe the events of the world right now are forcing you to wear both these hats – all at once! Being a parent can be very stressful. Between waking up and going to bed each night, there is a list as long as your arm of daily chores and jobs to do. Many of us have been there and totally sympathise with just how hard it is to juggle all of these elements of life. Here at Back in Business Physiotherapy, it is not uncommon for us to see mums in pain, stressed out and struggling to balance family, work and life. Of course, there are dads out there juggling all these elements as well, so if you’re a dad reading this, take note! There isn’t an easy solution to this problem, but there are many things you can try to do to begin making this process more manageable. Have a read through these five tips to see if they might work for you: 1. Set a consistent routine: This is a very handy thing to have in place. Busy schedules can be hectic and difficult to stay on top of. There are certain daily events that we can keep to a strict schedule, which can help to limit stress by managing each task. Try and keep wake-up and bed-times, bath times, mealtimes and story times to the same time every day. This gives you less to think about and frees up some brain space for concentrating on the day ahead, which may include an important work presentation that needs focus. Most children respond well to routine, so getting one established can mean more settled children and a more chilled mother. 2. Exercise regularly: We know that exercise is beneficial for staying fit, healthy and strong. There is also countless evidence for the effect of exercise on the mind and helping to reduce stress levels. Exercising regularly can help to reduce fatigue by improving sleep, concentration, mood levels and overall brain function. When we exercise, our bodies produce increased levels of the happy hormone (a.k.a endorphins) which help us to both tackle and stave off the effects of life’s stressors (bored screaming child). If you can’t get out for a walk or run, try some at-home exercises, a YouTube clip, or better yet, turn up the volume, and have a dance party with the kids. It lets them burn some steam, while you get some activity in. And it builds connection – win, win! 3. Consume a healthy diet: Stress hormone release is controlled by our adrenal glands. High stress situations over time can lead to increased levels of stress hormones coursing through our bodies. What we eat can help control the effects of stress. Controlling blood sugar levels is pivotal in maintaining good control of adrenal gland function. We recommend a balanced diet containing high amounts of natural, whole foods and keeping intake of sugary, nutrient-poor foods to a minimum. Foods rich in vitamins C and B are particularly important for supporting adrenal function. Try to include red bell peppers, nuts, seeds and leafy green vegetables to ensure you are getting a good supply of essential nutrients. 4. Stay hydrated: This is a simple and easy method to implement. It takes nothing to pour yourself a glass of water from the tap. Water is life-giving to humans. Without it we die quickly. All of our bodily processes and tissues rely on it to function efficiently. This includes proper function of the brain and all of the organs in our body. When we become dehydrated, the levels of cortisol (a stress hormone) increase. Stay ahead of the game and keep a bottle of water with you through-out the day. Sip regularly and your body will stay well-hydrated and ready to deal with any of those stressful scenarios that might pop up during the day. 5. Take time for yourself: We think this is the most important one of all. With being a parent comes enormous responsibility, but if you do not look after yourself above all, there is no possibility of looking after one or a whole troop of other family members. Set aside time when you can to read a book, do some exercise, meditate or do whatever makes you happy. Take a trip to the zoo or a museum on your own every now and then. If you organise these things in advance to ensure the kids are looked after by a friend or family member, then these things are easily achievable and help to keep you sane and grounded. 6: Home gym: if you have the space and a place to roll gym equipment out onto a balcony or verandah, you can keep up your fitness levels whilst in 'lock-down'. Multiple equipment will allow everyone to exercise at once. Elliptical Trainer, Plyometrics Box, Stationary Bikes, Treadmill, Rower, Punching Bag, Heavy Rope, Chin up bar, Swiss Ball, etc, etc. In these uncertain times, a pandemic which keeps on giving, potential worlwide economic collapse, home schooling, working from home, restrictions of liberty will all test our humanity. Emotional and physical stress will make parenting more difficult than ever before. We don’t think for one minute it is as easy as ABC to get all of this going alongside all this madness. Planning now, especially if there is a complete shut-down. It also looks like we are in for the long haul, potentially up to several months. But try to implement things slowly and steadily to make sure it fits well into your new daily routine. There is no handbook in such an unprecedented scenario for stress-free parenting, but we hope we’ve given you some food for thought! Isolate and keep up a routine. Uploaded : 1 April 2020 Read More -

COVID-19
Dear Clients, Back in Business Physiotherapy has been operating for most of the June - September 2021 spike in COVID. This has been at a limited capacity to minimise risk of infection. In October 2021, we will recommence having reception staff in the mornings only. During November, we're hoping to have our full reception capacity and no longer limit the number of appointments we have on offer. However, this will be in line with NSW health recommendations. If Singapore on 29 September 2021, is anything to go by, their 80% double vaccination rate hasn't prevented them to commit to another lock down, so that hospital capacity isn't over-stretched. A similar approach occurred in Scotland, where a 3 week lock down was commenced in September 2021, to allow the NHS to 'catch up'. Hence, at BinBPhysio we're committed to ensuring the safety of our clients and staff. Online bookings When you make a booking online, you will see some COVID screening questionnaire. Emails As a client you may receive an email with a signature detailing our expectations of our clients. We are in the process of installing an air filtration unit, fans, cough/sneeze shields and continue to maintain clean surfaces using hospital grade disinfectant wipes. Air Purifier The Samsung AX500K air purifier has been recommended by the CDC in the United States. This unit is recommended for 90m2, which is sufficient for our suite. Additionally, we have A/C units specifically for our suite, as well the capacity to open windows from the bottom and the top, thereby allowing further ventilation and air exchange. Rapid antigen testing kits Consideration also needs to be given to the possibility that relatively high COVID-19 rates are required in a population before rapid antigen self-test results are reliable. The March 2021 Cochrane systematic review assessing rapid tests for the detection of SARS-CoV-2 infection(COVID-19) suggested that at 0.5% prevalence asymptomatic screening would result in 70-90% of rapid tests being false positives and 30-50% of cases being missed. NSW health and the TGA are considering rapid antigen testing to become available to all households by December 2021. By this stage it is expected the sensitivity and reliability of the self testing kits to become verified. As of September 2021 neither the Australian Physiotherapy Association nor NSW health were recommending the use of kits in Private Practice. Back in Business Physiotherapy will continue to review the use of these kits and will be prepared to use them if they become recommended. Late September 2021 - vaccination rates against the virus A road map to opening was outlined in late September 2021 after 3 months of 'lock down' in the Greater Sydney Region. This included gradually opening up in mid October 2021 when a predicted 70% of the NSW population was doubly vaccinated. A projected 85-93% double vaccination rate was considered feasible to suggest complete 'opening' by early December 2021. As such, the NSW government wasn't aiming for zero COVID cases but a population 'living with the virus'. Such an amazing vaccination rate suggests that the NSW hospital system will be able to cope with the virus. COVID-19 NSW Delta strain outbreak : June/July 2021 Late June, the delta variant of COVID-19 was introduced into the Eastern Suburbs of Sydney by a driver, presumably contracted whilst transporting flight crew. Initial LGA partial lockdowns for 1 week and partial lockdowns across Sydney for 2 weeks did little to stop the spread, particularly in South Western Sydney. By the second week of July a strict lockdown has been ordered and 12 July 2021, numbers were still rising (112 new cases). Unfortunately, nationwide only 8% of Australians are fully vaccinated. Towards the end of September 2021, Australia had recorded almost 100 000 COVID cases, with the majority, ~ 61 000, occurring in NSW. All staff at BinBPhysio had been fully vaccinated by September 2021. Hence, during July and August 2021, Back in Business Physiotherapy was partially open, whilst using strict hygiene and contamination control protocols. Nearly all clients attending the practice during the first weeks of July were fully vaccinated. We are requesting that all clients use the NSW Health QR check in code when attending the practice. This procedure has already been in place since mid 2020. Mandatory mask wearing as stipulated by NSW Health. Masks : A standard medical face mask is more effective at preventing the wearer from inhaling aerosols without causing substantial breathing resistance than various cloth, medical, or respirator masks (Christian M. et al 2021, March 3, PLOS One, https://doi.org/10.1371/journal.pone.0248099 Tara Haelle Medscape Sunday, July 18, 2021) We will be using P2 and N95 masks at our practice. Some staff may also use perspex face shields Cough/sneeze shield As of October 2021, sneeze/cough shields will be installed at the reception desk. Seating, appointment time spacing and cleaning Two seats, 1.5m apart as well as seating outside, in the hallway, will be provided. Additionally, appointment times will be made to reduce client cross over as well as allow sufficient time to thoroughly clean cubicles, gym and reception areas. Cleaning agents with at least 40% alcohol content will be used, both as aerosols and as surface wipes. NSW health has a list of warnings for COVID exposed locations Please look at the NSW health COVID updates daily. Even if you feel well, if you were in one of the COVID hotspots please get tested. Depending on their recommendations you may still need to quarantine for 7-14 days, whilst testing negative. Vaccinations : 12 July 2021 In July 2021, BinBPhysio reduced working hours to accommodate acute clients and those whose chronic condition would worsen considerably, as only 8% of all Australians were fully vaccinated. In July, only two vaccines were available - Astra Zeneca, which was recommended for over 60's but became available at NSW pharmacies for over 40's. Some blood clotting risks with Astra Zeneca have been known to occur. Frontline workers and health care workers had been prioritised. Pfizer has been recommended for people under 60. Some heart and brain inflammation side effects have been reported. As the outbreak worsened, people were encouraged to vaccinate regardless of age or vaccine type. Later in September 2021, Moderna vaccines arrived in Australia. Researchers in the UK reported up to 80% protection against hospitalisation in over 80 year olds (https://www.bmj.com/content/373/bmj.n1088#) Researchers in Israel, where almost the entire population has been vaccinated with A-Z and Pfizer reported, - one shot of the vaccine was partially effective, offering 58% protection against infection, 76% against hospitalisation, and 77% against death - by seven days after the second dose (Pfizer), the vaccine was giving people 95.3% protection against infection and 96∙7% protection against death (https://www.google.com.au/amp/s/amp.theguardian.com/world/2021/may/05/two-pfizer-covid-vaccine-doses-give-over-95-protection-shows-israel-study) However, this provocative graph came our on 12 July 2021, which is somewhat misleading when compared with serious illness, hospitalisation and death. More uplifting are the preliminary results from the UK on hospitalisation : According to an analysis by PHE, the Pfizer/BioNTech jab was linked to a 94% vaccine effectiveness against hospital admission with the Delta variant after one dose and 96% after two doses, while the figures for the Oxford/AstraZeneca jab were 71% and 92% respectively (The Guardian, Australia 16 June 2021) "it's not a race" (Scott Morrison PM) Unfortunately, many reports in the media (and the fact that only 8% of Australians have been vaccinated) suggest the Morrison government is yet again (eg 2019 Bushfires), hopeless in a crisis. Australia is in a mess because the federal government bungled its vaccine procurement strategy – in particular its dealings with Pfizer, which it seems to have skimped on initially. The most damning part of Tingle’s report, and a point Rudd no doubt wanted to highlight, is the apparent confirmation that Australia got off on the wrong foot with Pfizer, with an anonymous business leader saying the government had displayed a “rude, dismissive and penny pinching” approach towards Pfizer, and sent “relatively junior bureaucrats” to the table. (A Guardian Australia report over the weekend backed this narrative, with Pfizer’s former president of global R&D John LaMattina describing Australia’s original order as “unconscionable”.) The health department has long been denying reports it botched its early meetings with the maker of the vaccine we are now desperately waiting on. But Tingle reports that well-connected Australian businesspeople in the US were “hearing even more graphic accounts of how badly offended the company had been by the response to its early approaches to Australia” (www.themonthly.com.au) Vaccine order : 25 July 2021 The Morrison government announced the acquisition of 52 million doses of Pfizer, suggesting that eventually everyone will eventually be vaccinated with Pfizer Vaccination totals : 13 July 2021 The delta variant appears to be highly transmissible and, unlike previous strains, affects children and young adults. The Sydney outbreak caught everyone by surprise, as the 'gold standard' contact tracing wasn't able to keep up with all those locations and people who have been asymptomatic and unknowingly spreading it in the community. It soon became apparent that the key to getting out of this outbreak was for everyone to get vaccinated, not only for themselves but for their country. COVID-19 vaccinations and musculoskeletal side effects - 8 August 2021 Last week, two separate clients presented with an exacerbation of injuries which I had treated previously. One was a 57 year old lady, who I had successfully treated for low back pain and nerve inflammation, a year previously. Three days after the Pfizer vaccine, she felt 'like a horse had kicked her in her back'. Luckily, her symptoms resolved after a few days. Another client, a 21 year old female, presented with severe ankle and foot pain. Similarly, three days after a Pfizer vaccination. I had treated her for a 'strange presentation' of calf and ankle swelling three years previously, for which multiple investigations found no explanation. Some form of vascular condition was suspected in the previuos presentation. This time around, her symptoms resolved within a week, however, her presenting symptoms were similar to someone with CRPS of the ankle and foot! Further reading : https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-the-immune-system-during-covid-19.html In the beginning : a historical perspective of BinBPhysio continued review and analysis of the COVID pandemic - March 2020 The following is an historical timeline of our analysis and review of the unfolding pandemic. Our work policies reflected the ever changing environment of this unprecedented situation. The following gives some perspective on how and why we responded in our work practices. North Sydney, was hit particularly hard, in terms of it becoming a 'ghost town', as most people worked from home over the past 18 months. Although this strategy was highly effective in reducing the rates of infections, peoples mental and physical well-being were affected, due to social isolation as well as poor work station home ergonomics. Read more.... Hence, updates of our policy, regarding COVID-19, has been a work in progress, with reflection of old information and the introduction of new information, which explained our reasoning for closing and re-opening of our practice. The questions at the time were : What are the rates of infection? What happens when we do nothing? How do we get herd immunity? Hospitalisation rate? Death rate of 1%, sickness rate of 20% and intensive/special care rate of 5%.Which countries are doing best? What is the political context of doing nothing? Should we wear masks? Can hot weather reduce the rate of infection? Economics versus health when closing the economy and re-opening gradually from a low base, using data, versus political expediency? Why people should not be complacent? On-going health and immune compromise? What are the symptoms in young versus old? Is this a hoax? Is this just another influenza? What are the signs and symptoms? What is Kawasaki disease? Is it just in the lungs? What are the mechanisms and treatments? COVID-19 growth : 29 April 2020 Flattening and Delaying the Curve : 30 March 2020 The reasoning for flattening the curve is to avoid over-whelming the health system. This strategy, has been advocated by the Imperial College Response Team. They have shown that those countries which isolated early, tested frequently and used personal protective equipment (PPE) liberally and appropriately had fewer deaths. Early in the pandemic, countries such as Taiwan, Singapore and Hong Kong were able to maintain a functioning economy by selectively isolating people who were testing positive for COVID-19. In countries, where recognition of the pandemic came too late, such as Italy, Spain and France, they required total shut down of peoples movements. Staggering death rates of 800 people in Bergamo alone and the death of 50 doctors in Northern Italy demonstrate the veracity of this virus, especially in the presence of inadequate personal protective equipment (PPE). Millions of face masks arrived today (30 March 2020) in Venice. Britain who commenced late, hoping for herd immunity, was on the precipice and still has rising fatalities. The PM himself, late to the party and a denier, also contracted the disease, and recovered just before the birth of his child. Those countries with a high sense of civic duty, such as Germany, who were airlifting Italian and French intensive care patients to Germany for treatment, where their mortality rate sat around 0.5%. Taking a 'nothing approach' such as advocated by President Trump in the USA and Bolsonaro, in Brazil, are showing high and prolonged mortality rates. However, these figures were likely to be skewed from lack of testing. Which brings us to Australia's measured response, of working from home and only essential services encouraged to be working outside of home. Isolation and testing, testing and testing. For the time being, this appears to have worked. Hence the regrettable decision to shut down of Back in Business Physiotherapy on 22 March 2020, could be partially reversed, with a gradual recommencement of services from the 5 May 2020. However, on 3 August, Victoria announced a 6 week stage 4 hard shut down. We will continue to monitor the situation locally, as well as head public health warning advice. We are taking all precautions, with regular cleaning, etc. All our staff are wearing masks. We'd like our clients to do so as well. Which countries have isolated best? 29 April 2020 The scary thing about this graph is that it shows that we'll be dealing with this for quite some time. 100 days is just over three moths, whilst 250 days is closer to 8 months! This brings the Northern Hemisphere back into the autumn/winter traditional influenza cycle! COVID-19 infection rates (17 July 2020) and those of influenza InfectionsCOVID-19: The first cases appeared in China in late 2019 and the first confirmed case in the United States appeared in January 2020. Approximately 13,832,242 cases have been confirmed worldwide. There have been 3,576,430 cases in the U.S. as of July 17, 2020.* Flu: The World Health Organization estimates that 1 billion people worldwide get the flu every year. In the U.S., for Oct. 1, 2019 – Apr. 4, 2020, the CDC estimates that there were 39 million to 56 million cases of flu. (The CDC does not know the exact number because the flu is not a reportable disease in most parts of the U.S.) DeathsCOVID-19: There have been approximately 590,608 deaths reported worldwide. In the U.S, 138,360 people have died of COVID-19, as of July 17, 2020.* On 3 August 2020, total deaths were 697,189. A large jump from 17 July 2020! Flu: The World Health Organization estimates that 290,000 to 650,000 people die of flu-related causes every year worldwide. In the U.S., from Oct. 1, 2019 – Apr. 4, 2020, the CDC estimates that 24,000 to 62,000 people died from the flu. (The CDC does not know the exact number because the flu is not a reportable disease in most parts of the U.S.) The COVID-19 situation is changing rapidly. Since this disease is caused by a new virus, people do not have immunity to it, and a vaccine may be many months away. Doctors and scientists are working to estimate the mortality rate of COVID-19, but at present, it is thought to be substantially higher than that of most strains of the flu. 140 institutions world wide are working on a vaccine. Two likely candidates are mRNA vaccines being developed at Finders University in South Australia and another one from The University of Queensland Footnote : the UQ vaccine although the first effective vaccine in the world had to be abandoned as they used an AIDS derived protein carrier, which unfortunately meant that a diagnosis of AIDS could not be made in people vaccinated in this way (2021) *This information comes from the Coronavirus COVID-19 Global Cases map developed by the Johns Hopkins Center for Systems Science Herd Immunity : 29 May 2020 vs 12 July 2020 The coronavirus pandemic has shown clearly what happens when a new pathogen gets loose in a population where no one has had it before: It spreads like wildfire. Long-familiar viruses, even ones that are every bit as contagious, can’t do that, because of a phenomenon called herd immunity. It works like this: The more people there are in a community who have protective antibodies, either through vaccination or past exposure, the less likely an infected patient is to encounter someone who lacks them and pass the virus along. Above a certain threshold, the virus can’t spread readily enough for an outbreak to grow. That’s why diseases like measles and chickenpox have become rare in countries like Australia and the United States even though not everyone gets vaccinated: if enough people do, then we achieve herd immunity. Notably, 90% of the population needs to have immunity for certain diseases such as Measles. Scientists and policymakers hope the world will get to that point with the coronavirus, too. But a crop of new studies suggests that herd immunity is still very far away. Additionally, thanks to the bush fires keeping tourists away, which meant keeping our COVID-19 numbers low, together with our isolation means, we'll be reliant on the rest-of-the-world for herd immunity. Gradual re-opening of our borders will be a tricky thing. Similarly, our nearest neighbour, New Zealand, went for eradication, so we won't be getting our herd immunity from there. The USA went down the politically expedient pathway of early re-opening without heading CDC guidelines. On the 12 July 2020 the USA had 62,653 new cases of COVID-19. Total confirmed infections were 3.29M with 137 000 deaths. Suggestions are that the number of unconfirmed : confirmed cases is 80 : 1, meaning that the total number of potential cases are 263.2M in a population of 328M. This is about 66% of the population which some people suggest that herd immunity may commence to take effect. Time will tell. Never-the-less, with the current infection rates, around 20% of positively tested and probably symptomatic people end up needing hospitalisation, 5% of those requiring ventilation or respiratory aid and around 1% die. Ideally, we can identify why some people remain asymptomatic, whilst others become critically ill. Furthermore, which young people are susceptible to blood vessel inflammation and megakaryocyte infiltration needs to be ascertained. However, concurrently, if the susceptible people are identified, those non-susceptible individuals should be considerate of those less fortunate, and maintain social distancing, use of masks, hand sanitation, etc. Interestingly, it appears that the death rate curve, in the USA, has started to flatten, or even trending downward. Comparing the infection and death rates in areas affected early by COVID-19, such as New Jersey and New York with Texas and Arizona, it may be that the treatment and preparedness for the pandemic has improved, and/or the virus is less virulent? However, on 19 July 2020, hospital bed capacity, in Arizona, had reached 100% occupancy and people were being moved to neighbouring states. Initially, clinicians considered it to be a respiratory disease, however now it's also considered a vascular disease. ICU survival rates in Australia are approx 85%, in the UK approx 60%, whilst in the USA it's as low as 30%. Apparently, it's been very hard to ween people off ventilators, so positive airways pressure masks, as used traditionally for sleep apnoea, and developed by ResMed, Australia, are preferred to intubation. International death rate : 14 July 2020 Interestingly, china appears in the 'rest of Asia' category. A medical case presentation in a NHS health care worker: early April 2020 The following is from a online clinical forum to which i belong. This pertains to emergency medical treatment, of a 47 year old RN (registered nurse). Although it is not describing physiotherapy, I feel it contains a lot of useful information for those who have been confused by social media.. The ensuing discussion related to the use of anti-biotics such as erythromicin. The consensus was to use it in case of secondary bacterial infection. However, one clinician pointed out that at least one publication demonstrated it's use for viral infections as well as significant anti-inflammatory side effects in the lungs. '#Azithromycin and erythromycin are unusual — for example erythromycin is given to increase gastric emptying time for GI issues. In the case of #Azithromycin, it might be that in addition to being anti inflammatory, it also has antiviral properties: Gielen V, Johnston SL, Edwards MR. Azithromycin induces anti-viral responses in bronchial epithelial cells. Eur Respir J. 2010 Sep;36(3):646-54. However, erythromycin may be treating co-morbidity factors due to increased vulnerability, to bacterial infections, in a compromised immune system? ' The reduced gastric emptying is also interesting as the gastric biome is one of largest sources of immune material in the body. The patient was later transferred to a special care unit. Let's hope that this front line care worker, as many others, survive. COVID-19 is not just a pulmonary disease - digestive symptoms : 7 May 2020 Breathlessness due to vascular complications in younger people : 11 April 2020 Breathlessness is a symptom that occurs 5-10 days into the disease. A gradual build up of hypoxia has been reported which may be accompanied by a loss of taste and smell, culminating in 50% oxygen saturation when people were turning up at hospitals. Pulse oxcimeters have been recommended. An example made, was Germany, where people diagnosed with COVID-19 are tested daily in their homes, hereby predicting morbidity, and resulting in the lowest mortality rates in the world. Other symptoms may include a temperature and sore throat, which can be accompanied by headaches, deep aches and pains. In some younger people stroke like symptoms such as drowsiness, slurred speech and paralysis. Additional symptoms are now evolving which include skin reactions and frostbite like rashes on the toes. "Of the first 200 reports analysed for the study, out of a total of 300 in the registry today, about half were toe rashes. The other skin conditions reported include hives, those itchy red bumps that are usually a sign of an allergic reaction; water blisters; and something that looks a lot like chickenpox". ( https://www.washingtonpost.com/health/2020/04/29/coronavirus-rashes-toes/ ). Federal government Health Direct website allows people to answer questions on symptoms and gives them a course of action. https://www.health.gov.au/resources/apps-and-tools/healthdirect-coronavirus-covid-19-symptom-checker Kawasaki disease in very young people during COVID-19 Although very rare, worldwide there have been around 100 reported deaths in children with Kawasaki syndrome (26 May 2020 Vancouver Health Official - Dr Henry Minister Dix). This appears to be a post viral syndrome. Additionally, there appears to be children to adult cross infection, rather than vice versa. Most likely, the very low incidence of COVID-19 in children is due to the limited number of ACE 2 angiotensin receptors in children compared with adults. These ACE 2 receptors are found in the upper respiratory tract, lungs, heart, intestines and kidneys (responsible for blood pressure). The conversion of angiotensin II to angiotensin which lowers blood pressure occurs here. Unfortunately, ACE 2 receptor sites are an entry point for COVID-19. Angiotensin II and ACE 2 receptor - Wikipedia 26 May 2020 ACE2 lowers blood pressure by catalysing the hydrolysis of angiotensin II (a vasoconstrictor peptide) into angiotensin (a vasodilator). As a transmembrane protein, ACE2 serves as the main entry point into cells for some coronaviruses, including HCoV-NL63, SARS-CoV (the virus that causes Severe Acute Respiratory Syndrome ) and SARS-CoV-2 (the virus that causes COVID-19). ACE2 mRNA expression is also found in the cerebral cortex, striatum, hypothalamus, and brainstem. The expression of ACE2 in cortical neurons and glia make them susceptible to a SARS-CoV-2 attack, which was the possible basis of anosmia and incidences of neurological deficits seen in COVID-19. As anosmia and dysgeusia (loss of smell and taste) are seen early in many COVID-19 patients, it was suggested to be considered to be a heralding clue in COVID-19, which subsequently was declared as "significant symptoms" in COVID-19 by the American Academy of Otolaryngology–Head and Neck Surgery. ACE 2 Practice Closure As you may be aware, the practice was closed from 6 March 2020 until 4 May 2020. It was a tough decision to make, however we were unable to be sure that we would not contribute to cross contamination of our clients with COVID-19. Although we are deemed an essential service, in the light of the Ruby Princess, we believed in the Australian Government and NSW Government policy of a shut down of non-essential services. When there was some loosening of these restrictions we were prepared to treat our clients so long as they were using the COVIDsafe app, and we are able to gain access to PPE (Personal Protective Equipment) and sanitising agents. At the time of closure, these latter resources were scant, and were better used at 'coal face' settings, whose role in fighting this virus was of a higher priority, than us. The practice re-opened on 4 May - with limited sessions and COVID-19 procedures in place. 'Normal' opening occurred after the Queens birthday long weekend, June 2020. We require all of our clients to be symptom free and to be using the COVIDSafe app. We also request all clients to wear masks. Projected deaths 26 March 2020 https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-Global-Impact-26-03-2020.pdf?fbclid=IwAR28ZrDCR6ZjR9H6dMfMLYhhGTk5nTPxm0BA5U9B7RahL9QTgNJGSklb0Hs Look at the North American and world numbers and compare them to these real numbers on 29 April 2020. Deaths vs number of infections is worrying and suggests a large number of unconfirmed cases. Compared to 22 June 2020. Exponential growth, with an extra million in the past month and many countries, such as Brasil, Russia, China and the USA, deliberately under-reporting the numbers, whereas other countries don't have the epidemiology tools to analyse let alone test symptomatic and asymptomatic people. Importantly, compare these numbers with those predicted by the Imperial College shown above. The fact that the USA has 120,000 deaths (23 June 2020) would suggest that the asymptomatic or untested population is much higher (over 17,730,000) or that the disease may be more deadly than predicted? Compare these results with those of America on 12/06/2020 where these numbers doubled in just over 6 weeks. This is in the midst of the Black Lives Matter protests. Considering that the infection takes 2 weeks to incubate, it is interesting to watch these numbers as America moves into summer, where in theory the virus should be less virulent. The following demonstrates that those 'hot' states are still showing high rates of infection as well as high rates of hospitalisation (Texas was at 97% capacity in early July). USA death rate almost 160 000 : 3 August 2020 - height of summer! Texas daily infection rate : 14 July 2020 Florida daily infection rates : 14 July 2020 Daily infection rates USA : 19 July 2020 USA death rate : 16 September 2020 Trump - do nothing approach - 5% of the world population but almost 20% of the world deaths Worldwide Status of COVID-19 - 30 March 2020 vs 30 April 2020 (1 million recoveries) vs 29 May 2020 vs 23 June 2020 (Opening, Post Shut Down) vs 1 August 2020 vs 16 Sept 2020 vs 12 July 2021 Heartening, are the number of 1 million recovered cases on 30 April. However, testing in many countries is still woefully inadequate and many people have now shown mild and severe symptoms which weren't previously associated with COVID-19. Big jump in numbers with testing and gradual opening up of the movement restrictions. In countries, such as Brasil and the USA, their presidents discourage social distancing and wearing of masks. Wearing a mask : 14 July 2020 Health authorities, in Australia, don't recommend wearing a mask, in all states, except Victoria. Reasons for this vary, but the major one, is that people gain a false sense of security and that they play, with their hands, with their masks. Worldwide, where there has been a significant outbreak and where a sensible health care administration exists, mask wearing has been recommended in places where social distancing cannot be practised. Australian Cases : 29 May 2020 vs 23 June 2020 vs 19 July 2020 vs 3 August 2020 Sudden increase in infection rates in Victoria, resulting in resumption of total stage 4 lock down, to stop the spread. Australian Cases : 8 April 2020 vs 22 June 2020 Bush Fires Australia is doing extremely well. Some of this can be attributed to the closing of borders and partial closure and social distancing measures. However, the borders weren't closed until the end of March. This was extremely late. By this time, the virus was rampant in Europe and other parts of the world. We also know that the virus existed since at least November 2019. The first death from COVID-19 in France was in December and evidence suggests that the virus was present in Washington State and California in late December. During November 2019 through to February 2020 Australia suffered the worst bush fires in history. A billion dead animals and 19 million hectres of burnt countryside. This meant that overseas tourists didn't come and visit Australia. Moreover, Australians themselves didn't move around to the usual holiday spots. Furthermore, thanks to the appalling smoke haze, most people avoided going outside. We were quarantining and self isolating, even though we weren't aware of this, at the time. Social Distancing : 10 April 2020 vs 19 July 2020 Note that the curve of new incidents is going down, which means social distancing is working. Clearly, we need to maintain this. Then, unfortunately, due to two security guards, doing the wrong thing, whilst guarding hotel quarantine people, a sudden surge of infections in Victoria : 19 July 2020 Recovery vs Death Rate - 15 April 2020 Australia The flattening curve in Australia 24 April 2020 Social distancing and partial shut down had been working. The curve of new cases was flattening. Then the tricky situation was the gradual re-opening. Testing testing and testing is critically important to contain areas of focal contagion. The other big question was what will happen as we go into winter?....as well as what happens when we gradually re-open? Active New Cases : 29 May 2020 Thanks to social distancing and government policy we were gradually able to re-open. But we became complacent. Letter from Spain - 7 April 2020 Hi Martin, thanks for your facebook message. We are going through a nightmare of which it will take time to wake up.I look after infected patients at my hospital, most of them frail and elderly. This disease is a death sentence for many of them.It is not particularly challenging in my context from a clinical point of view, as you give them support and little else, either they survive or not. The problem are young people at general hospitals sometimes without availability of critical care beds and ventilators. There are many reasons to understand why Italy and Spain are hit so badly. I just wish your country does not get into this ordeal. Aside from purely clinical aspects, logistics and psychological topics are the problem: lock down, isolation, lack of equipment at the hospitals and long-term facilities, giving bad news through the telephone instead of face to face, people die alone, consequences of all this for mental health ...We still have quite a few weeks of lock down ahead and the social and economic consequences of all this are going to be catastrophic, but we shall have to manage somehow. Political situation is highly unstable and deeply worrying. Hope we shall survive that aspect too.How are you getting on yourselves and your relatives?I´m not aware of the situation in your continent, to be honest, but I do not think anywhere in the world will be spared, under very effective countermeasures are timely taken in the places where it has not set foot yet.Take care and keep social distancing and ancillary measures, for now we do not have any other approach. Politicians ignored all advice and did not realise that a pandemic was approaching and it could have devastating consequences. From an infectious diseases keen student as I am, this virus compounds the perfect storm.All the best for now from Spain,Angel Optimism : 31 March 2020 Currently, there is room for optimism. Last night's (31 March 2020) new cases were down from double digits to around 9%. Australia has one of the highest rates of testing in the world. Social distancing, self isolation and isolation of people testing positive seems to be finally having an effect Work on using blood 'pin prick' testing kits is demonstrating a result within 15 minutes of testing and should become more readily available shortly. Unfortunately, there seems to be an unacceptable high rate of false negatives (up to 48%), which may give people a false sense of security. However, apart from the upside of 'ease of use', this type of testing allows people to monitor the production of anti-bodies to COVID-19. Such production, is synonymous with a persons immune system actively fighting the virus. In people, who have recovered or who only had mild symptoms, it may be possible to harvest their blood plasma and use those in transfusions for people who are critically ill. It's a similar principle to the methodology used, in the past, for immunisation against Hepatitis A. Antimalarial drugs based on chloroqine were showing some potential benefit, but should only have been prescribed under medical supervision. For some odd reason, the president of the USA thought it was OK to recommend it to the general public!!!! However, a gin and tonic to calm the nerves, at the end of day may be used, as the tonic contains a small amount of quinine.......ha ha In theory, chloroquine could be used as a prophylactic against COVID-19, as it has been used as a prophylactic against Malaria and is used in people with auto-immune inflammatory disorders. We do know, that people who do badly, are the ones who have a compromised immune response, where there is an over-activity of immune substances creating a 'cytokine storm' in older individuals, or platelet over-activity resulting in blood clots in younger people. Anti viral drugs will probably be paramount in the fight against this virus. Anybody watching the news from the United States will notice the immunologist Dr Anthony Fauci. He was at the forefront of AIDS research in the infancy of that epidemic back in the 1980's. He's advised every president on pandemics and epidemics since then. Considering that the man is in his early 80's, he's an incredibly tough and brilliant guy and a sane sight at Trumps hopeless press conference briefings. Another reason for optimism is the use of the TB antigen. The TB vaccine has been shown to reactive the innate immune system and has been used over the past few years in the treatment of bladder cancer. In fact, a few years ago, my mother-in-law, was diagnosed with an inoperable tumour, sitting on the kidney and next to the aorta. Over the following month, the tumour continued to grow, when suddenly it began to shrink, without any form of intervention. The diagnosis was never clear, however, all the puzzled specialists felt that it could have shrunk thanks to the fact she had had TB as a child!? http://malthus.micro.med.umich.edu/lab/pubs/nrmicro1919.pdf The innate immune system is the one we're born with. As we go through life, we are exposed to various pathogens, which create an innate immune reaction which produces the anti-bodies of the acquired immune system. Unfortunately, as we age, we have less protein in our body to produce such anti-bodies. The classic immune substances involved with this process are heat shock proteins (HSP). These are the basic building blocks of multi-cellular life. In mammals, the HSP's act with muscle protein to produce immune conversion. Unfortunately, after the 3rd decade of life, sedentary adults lose 1% muscle mass per year and after the 6th decade of life they lose 2% of their muscle mass. This process is called sarcopenia. To avoid sarcopenia individuals need to do at least 40 minutes of quality exercise, around twice a week. Hence, stay healthy, keep exercising and maintain muscle mass so that you have the reservoir of protein needed to fight infections and decay. Furthermore, regular exercise in this age of partial shut down is another good way to maintain mental health. mRNA vaccines : 3 August 2020 Just like normal vaccines, RNA vaccines are intended to induce the production of antibodies which will bind to potential pathogens. The RNA sequence codes for antigens, proteins that are identical or resembling those of the pathogen. Upon the delivery of the vaccine into the body, this sequence is translated by the host cells to produce the encoded antigens, which then stimulate the body’s adaptive immune system to produce antibodies against the pathogen. mRNA vaccines have never been used before. They differ to traditional vaccines, in that they encode the protein sequencing to produce antibodies (IgG) identical to those found in people who have immunity to novel corona viruses. They may also have a potential role in the treatment of cancer. Novovax : Australia For Phase 1 only. Additional information will be provided if Phase 2 is implemented. 2019nCoV-101 is a 2-part, randomized, observer-blinded, placebo-controlled, Phase 1/2 trial designed to evaluate the immunogenicity and safety of SARS-CoV-2 rS nanoparticle vaccine with or without Matrix-M adjuvant in healthy participants ≥ 18 to 59 (inclusive) years of age. The study will be conducted in 2 parts. In Part 1, at least 1 and up to two SARS-CoV-2 rS constructs will be evaluated in up to 2 cohorts, which may be enrolled in parallel. An interim analysis of Part 1 safety and immunogenicity data will be performed prior to an optional expansion to Part 2. https://clinicaltrials.gov/ct2/show/NCT04368988?term=vaccine&recrs=a&cond=covid-19&draw=2 University of Queensland University Queensland COVID19 Trial Vaccine Astra Zenica, UK http://www.isrctn.com/ISRCTN89951424 WHO https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines A possible concern could be that some mRNA-based vaccine platforms induce potent type I interferon responses, which have been associated not only with inflammation but also potentially with autoimmunity. Thus, identification of individuals at an increased risk of autoimmune reactions before mRNA vaccination may allow reasonable precautions to be taken. Exercise and the immune system Your muscles are a major endocrine organ of the immune system. Their lean muscle bulk, is of utmost importance to ensure a sufficient reservoir of protein, which is needed to mobilise an immune defence. People should exercise muscles regularly, not only to prevent sarcopenia, but also to mobilise and fine tune your immune system, as well as maintain a healthy BMI Progressive resistance exercise and endurance training Physiotherapy and the enhancement of perception of musculoskeletal and hence immune health Investigation into combined drug treatment : Chloroquine and Azithromycin : 20 March 2020 Chloroquine and hydroxychloroquine have been found to be efficient on SARS-CoV-2, and reported to be efficient in Chinese COVID-19 patients. They evaluated the role of hydroxychloroquine on respiratory viral loads. Patients and methods French Confirmed COVID-19 patients were included in a single arm protocol from early March to March 16th, to receive 600mg of hydroxychloroquine daily and their viral load in nasopharyngeal swabs was tested daily in a hospital setting. Depending on their clinical presentation, azithromycin was added to the treatment. Untreated patients from another centre and cases refusing the protocol were included as negative controls. Presence and absence of virus at Day 6-post inclusion was considered the end point. Results Six patients were asymptomatic, 22 had upper respiratory tract infection symptoms and eight had lower respiratory tract infection symptoms. Twenty cases were treated in this study and showed a significant reduction of the viral carriage at D6-post inclusion compared to controls, and much lower average carrying duration than reported of untreated patients in the literature. Azithromycin added to hydroxychloroquine was significantly more efficient for virus elimination. Conclusion Despite its small sample size our survey shows that hydroxychloroquine treatment is significantly associated with viral load reduction/disappearance in COVID-19 patients and its effect is reinforced by azithromycin. Philippe Gautret et al (20 March 2020) https://www.sciencedirect.com/science/article/pii/S0924857920300996 Importantly, this small n=6 investigation is what the president of the USA and Fox News were basing all their hopes on. It could also be dangerous to treat some patients in this manor. As we've outlined on our FB page, we suggest people follow the facts and not believe in an orange Buffoon. President George W Bush predicted and prepared for a pandemic in 2005. The orange buffoon and taking prophylactic hydroxychloroquine - 26 May 2020 Chloroquine - 12 June 2020 After WHO discontinuing research into Chloroquine, they have reversed that decision as it is thought that that the above investigation was flawed. It might be best to take the medical interventions and directions of research out of the hands of non-specialists and the media! The orange buffoon - recommending internal UV and disinfectants - 26 April 2020 This is 'fake news' ?......but continues on with the appalling handling of COVID-19 by the President of the United States. President Obama continued along this path for preparing the USA for pandemics by creating a global pandemic detection and deterrent department in the CDC. The orange buffoon dismantled all these things!!!! Additionally, it would appear he was given warnings of the impending pandemic as early as January 2020. But since he watches Fox, for his news, he remained ignorant of them. The key to good leadership is knowing when you aren't the smartest person in the room. The warning, (in late January 2020) written in a memo by Peter Navarro, President Trump’s trade adviser, is the highest-level alert known to have circulated inside the West Wing as the administration was taking its first substantive steps to confront a crisis that had already consumed China’s leaders and would go on to upend life in Europe and the United States “The lack of immune protection or an existing cure or vaccine would leave Americans defenceless in the case of a full-blown coronavirus outbreak on U.S. soil,” Mr. Navarro’s memo said. “This lack of protection elevates the risk of the coronavirus evolving into a full-blown pandemic, imperilling the lives of millions of Americans.” ( https://www.nytimes.com/2020/04/06/us/politics/navarro-warning-trump-coronavirus.html ) The orange buffoon and World Health Organisation (WHO) WHO was warned by Taiwan, in late November 2019 about an N!H1 like virus in Wuhan. WHO ignored this, as Taiwan isn't a part of WHO. Additionally, Taiwan is considered by China as a part of it's sovereignty. The Washington Post, Taipei desk, warned of a H1N1 like virus (SARS) coming out of Wuhan on 6 December 2019. WHO declared a pandemic after Chinese New Year (mid January 2020) to pander to China's sensitivities. Never-the-less, a pandemic was declared by the end of January 2020. Apart from letting a precarious situation fester for two months and get out of control, it's given the orange buffoon someone to blame!!! Basically, all of February was lost with inaction by him, 'it's a hoax", "it will go away, just disappear", This narcissistic attitude, as well as posturing by his sycophants, has not only exposed health care workers to unacceptable danger, it probably has resulted in tens of thousands of potentially avoidable deaths. Lack of PPE and ventilators, institutions specifically for such a crisis having been dismantled, being some of his many failings. Just listen to the governor of New York, Andrew Cuomo. Then, the incredible news in mid April, when WHO gave the green light for the wet market in Wuhan to re-open. Clearly, WHO has to walk a political tight rope, considering various cultural sensitivities and needing to appease many disparate parties with varying geopolitical considerations. Ultimately what is of paramount importance is the health and well-being of the worlds population. Hopefully, going forward, a constructive relationship can be developed by all parties within and outside of WHO, in the fight against the virus. Erythromycin Erythromycin is an antibiotic which has been used for many decades. Unlike many antibiotics, people do not develop resistance to it's effect. Classically, the drug was used for lung conditions. Interestingly, my father, Norbert Krause, is probably the last living person in Australia who knows the industrial process of making erythromycin. He was involved, as an industrial chemist, in it's production, at Abbott Laboratories, in Kurnell, NSW, Australia, until production was shut down some time in the 1980's, for cheaper options overseas. Another victim of globalisation. Heat Shock Protein 90 (HSP-90), Geldanamycin and COVID-19 : 19 May 2020 An intersting artcile on drug repositioning (defined as the use of approved drugs for new indications), offering an unmatched opportunity to offer novel therapeutics to treat SARS family of coronaviruses (SARS-FCoVs); Reaserchers analyzed, a dataset of patients who presented with SARS during the 2003 outbreak whereby they established a gene signature that defines differential gene expression in patients who were sick with SARS vs. healthy controls and convalescent patients. They used a robust platform to conduct drug repositioning based on clustered gene expression and pathway enrichment to identify best matching drugs. They identified 55 agents of potential benefit. In most of these drugs they were able to establish a link to previous related research, use as antiviral, or at least a hypothetical role in treating SARS-FCoVs. Most notably, the heat shock protein 90 (hsp90) emerged as a major component that enables viruses to hijack infected cells through the process of autophagy. Almost half of the drugs identified could be linked to hsp90. As such, they propose using hsp90 inhibitors, mainly geldanamycin and its derivatives, to treat COVID-19. (https://www.researchsquare.com/article/rs-18714/v1) Based on their findings, they suggest adding more drugs to the experimental arsenal deployed against SARS-FCoVs. They suggested using nontoxic drugs that are readily available for wide scale prophylaxis or the treatment of mild cases of COVID–19. These drugs would include omeprazole, nonsteroidal anti-inflammatory drugs, colchicine, sulfoanamide antibiotics, antimalarial drugs and clozapine/chlorpromazine. For patients with serious COVID–19 illnesses, the above drugs can be combined with immune modulators like sirolimus, and direct Hsp90 inhibitors under well-designed clinical trials. Given the high pathogenicity of the current ongoing epidemic, they suggested that it seems prudent to attempt to use multiple drugs in combination if low risk for toxicity and drug-drug interaction is established. Choosing a combination of drugs identified in this study or other drug-repositioning studies and careful reporting of the efficacy of these experiences can result in rapid accumulation of knowledge.(Iyad Sultan, Scott Howard, Abdelghani Tbakhi (2020, DOI : 10.21203/rs.3.rs-18714/v1) https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-the-immune-system-during-covid-19.html#HSP90 Added Complication - 27 April 2020 Pulmonary embolus and venous pulmonary clots Growing clinical evidnece is finding severe clotting in some individuals with COVID-19. Moreover, pulmonary clots and even strokes have been reported in young individuals (aged 20-40) by an Australian physician in New York (Washington Post 26 April 2020), In fact, the clotting was so profound that re-clotting was occuring during clot busting surgery. Pulmonary venous clotting has also been described by French physicians. A research letter from Hôpitaux Universitaires de Strasbourg published today in Radiology reported that of 106 pulmonary CT angiograms performed for COVID-19 patients over a one-month period in a tertiary care centre in France, 32 patients (30%) had acute pulmonary embolus (PE). This rate of PE is much higher than usually encountered in critically ill patients without COVID-19 infection (1.3%,) or in emergency department patients (3 to 10%). In the study, a D-dimer threshold of 2660 μg/L detected all patients with PE on chest CT. A second research letter published today described a study from Centre Hospitalier Universitaire de Besancon in France pointed to high proportion (23%) of COVID-19 patients with contrast CT had PE. PE was diagnosed at mean of 12 days from symptom onset. Patients with PE were more likely require care in the critical care unit and to require mechanical ventilation. (https://www.sciencedaily.com/releases/2020/04/200423143100.htm) Therefore, there is strong evidence of a combined airway-vascular response leading to organ failure. Such a combination of a 'cytokine storm' and thrombocytic events incorporating auto-immune responses leading to respiratory failure and the need for intubation and ventilation, even in young people. Obesity and COVID-19 in younger people : 5 May 2020 Health Minister announcement 31 March 2020 The Australian minister of health announced the take over of private hospitals with the already announced cancellation of elective surgery. This will bring the total capacity of beds in Australia to 35000, of which 2200 are ICU beds. Currently, 47 ICU beds are occupied by a COVID-19 patient. Furthermore, respirators for anaesthesia are being remodelled to become ventilators, bringing the total number to around 5000 ventilators. ResMed is currently building more ventilators to bring the total number to around 7500 by the end of April. Additionally, CPAP masks, normally used for sleep apnoea, will be manufactured and deployed, as their positive pressure should help prevent lungs from collapsing. Countries begin to re-open : 16 April 2020 Denmark and Germany have announced partial re-opening of the country from quite strict shut-down implementation. Denmark announced that pre-schools and primary schools would begin to re-open. The thinking here, is that children and parents of young children, who are generally part of the younger population are more resilient to COVID-19. Speaking with my wife's cousin, whose a GP in Denmark, he said that there was still a general lack of PPE, even in his practice, let alone in the general population. He also stated that if there wasn't a relaxation of the restrictions, there could be social issues, such as alcoholism, domestic violence and even civil unrest. On the other hand, Germany has gone the furthest with testing, PPE, health implementation and even taken patients from France and Italy. Their confidence for a general but gradual re-opening is because of their high rates of testing and epidemilogical capabilities. Australian re-opening : 29 May 2020 Looks like there is a predicted gradual re-opening in Australia around mid May is going ahead as scheduled. NRL played their first game post lock down. Community sports have been given the green light to start training with no more than 10 people in a group. Matches may start as early as July. No doubt, some parts of the country will re-open at different rates to others, depending on active cases. Until a vaccine is found, it's also possible that roll back and shut downs will also occur along the way. Interestingly, this week an anti-viral Remdesivir, a vaccine out of Baltimore, is being trialled in Victoria. Early days, but wouldn't it be great if Australian becomes part of the cure. In NSW, two clinical trials and peer consensus recommended approach to treatment are the current policy. Assurance Please bear with us in this time of crisis. Rest assured, we have begun to re-open as as we feel it is safe to do so. However, remember, North Sydney has a working population from all over Sydney, making it even more prudent to be cautious with our re-opening. We are cleaning morning and night as well as between each client. We are also keeping the number of people at anyone time, in the practice to 5 in 84m2. In the mean time, don't hesitate to contact us via email or make a booking on-line. https://www.myhealth1st.com.au/find/physiotherapists/nsw/nsw-region/north-sydney/back-in-business-physiotherapy. Additionally, you can stay up-to-date using our Facebook Page : https://www.facebook.com/backinbusinessphysio/ Download the tracking app - 26 April 2020 Today I downloaded the tracking app for COVID-19. Testing, testing, testing is super important to track and contain the virus. It is impossible to test everyone, and even if someone who has tested negative one day, can still test positive a week later. Therefore, downloading the tracking app will allow authorities to notify us if we've inadvertently been in contact with someone who has tested positive. If there isn't universal download of this app, then further spreading and ensuing deaths could occur. The alternative would be to have more 'shut downs' and even more serious restrictions of our liberty, re-imposed! Unfortunately, at the end of May only 6 million people have downloaded the app. I've downloaded the COVID-19 tracking app. It's imperative that we all do so. It makes our invisible mortal enemy visible. Not knowing that we've been in contact with the virus is disconcerting enough, let alone if the authorities are powerless to act, because they don't have the knowledge, to know where, to contain it. This becomes even more important as we begin to open up the country. Do everyone a favour and download the App https://www.health.gov.au/resources/apps-and-tools/covidsafe-app Opening - 4 May 2020 Currently, at Back in Business Physiotherapy, we are considering A VERY LIMITED OPENING of 2 DAYS PER WEEK, with very strict 1 client per hour schedule. This should minimise any client overlap as well as give us sufficient time to clean all surfaces and the treatment room. Stay tuned, but it could be as early as 1 May 2020. Currently, 14 July 2020, we are open 4 days a week, whilst still maintaining a strict cleaning regime. I also do wear a mask. Psychiatric issues amongst health workers who had contracted COVID-19 - 28 April 2020 There was very sad news of a young previously healthy doctor who went back to work after recovering COVID-19 and subsequently took her own life!! "She went down in the trenches and was killed by the enemy on the front line," Philip Breen said. "She loved New York and wouldn't hear about living anywhere else. She loved her coworkers and did what she could for them.""I just want people to know how special she was," he added. Health care workers face a mental health crisis as they battle the coronavirus pandemic. Philip Breen is a retired trauma surgeon, and he and his daughter would speak frequently about work, he said. Lorna Breen told her father that her colleagues were putting in 18-hour days and sleeping in hallways, and that ambulances couldn't get in because it was so busy. She worked in the emergency department and had been on the front lines for weeks, handling the onslaught of cases, her father said. New York City has been the US' pandemic epicentre, recording nearly 300,000 cases and more than 22,000 deaths as of Tuesday morning. Breen contracted Covid-19 and took a week and a half off to recover, but when she went back to work, she couldn't last through a 12-hour shift, her father said. Still, she felt like she had to get back in there to help her colleagues. "Frontline healthcare professionals and first responders are not immune to the mental or physical effects of the current pandemic," said Charlottesville Police Chief RaShall Brackney. "On a daily basis, these professionals operate under the most stressful of circumstances, and the Coronavirus has introduced additional stressors.""Words cannot convey the sense of loss we feel today," the New York City hospitals where Breen worked said in a statement."Dr. Breen is a hero who brought the highest ideals of medicine to the challenging front lines of the emergency department," they said. "Our focus today is to provide support to her family, friends, and colleagues as they cope with this news during what is already an extraordinarily difficult time." https://edition.cnn.com/2020/04/28/us/er-doctor-coronavirus-help-death-by-suicide-trnd/index.html Dr Fauci comes under attack - 13/05/2020 Unbelievably, the Trumpster and his favourite TV organisation FOX, attacked Dr Fauci's opinion on children return to school timetable. During a senate hearing testimony, Dr Fauci suggested that it would be more prudent to wait for a vaccine before children return to school. FOX suggested that Dr Fauci was unqualified as he wasn't elected to do so. They also suggested that he is a mouthpiece of the democrats. This is unbelievable in the face of the increasing prevalence of Kawasaki Disease during COVID-19. Additionally, a former Trump administration official who was controversially removed from his post has warned that the US faces its "darkest winter in modern history" unless the federal government develops a coordinated response to the coronavirus. Dr Rick Bright, the former head of the Biomedical Advanced Research and Development Authority, was in charge of the federal agency responsible for developing a vaccine and therapeutic treatments for COVID-19 until he was reassigned to a less significant position in April. Bright has filed a whistleblower complaint accusing the Trump administration of improperly pushing unproven treatments such as hydroxychloroquine and failing to grasp the seriousness of the outbreak until it was too late. The real heroes are the health officials and front line care workers not narcissistic self serving politicians, surrounded by their sycophants.. Health Care Workers being attacked There have been very disturbing reports of health care workers being attacked, doused in bleach and chlorine, evicted from their homes, etc. THIS IS TOTALLY UNACCEPTABLE - THE DEPRAVITY OF HUMANITY AT ITS WORST!! But when people are scared for their survival, those primival instincts come to the fore. https://www.theguardian.com/world/2020/apr/23/mexico-health-workers-attacked-covid-19-fears .......and to all our 'coal face' front line health workers - a tribute to them Potentially, the virus has been around since October 2019 A novel research approach by Harvard University, using satellite images of car parking movements of a Wuhan car park, suggest that some kind of epidemic was already commencing much earlier than we thought. Correlation doesn't necessarily mean causality, so in the abscence of Chinese openess to researching the origins of the COVID-19 virus, these results should be taken with a grain of salt. Exercise and the immune system, especially when ageing If you would like to understand how exercise affects the immune system, please take a look at this page, on another part of this website. https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-the-immune-system-during-covid-19.html Uploaded : 30 March 2020 Updated : 20 September 2021 Read More -

Corona Virus Policy
Uploaded 4 March 2020 Read More -

Bushwalking, hiking and rambling for cardiovascular and mental health
Hiking, bushwalking and rambling – it’s so much more than a view! Do you love the outdoors? Fresh air, sunshine, wind, rain, wildlife and nature… Blissful! We don’t know about you, but we absolutely love to get outside and immerse ourselves in the natural environment. Just you, a backpack, some energy food, a water bottle and for the organised ones, a compass and a map. Oh, and don’t forget those hiking boots. Prion Beach and Precipitous Bluff, South Coast Track, Tasmania (Dec 2019) If you’ve never considered hiking before, but like the thought of immersing yourself in nature while getting some great exercise, then maybe you need to. With technology leading the way these days, it’s easy to get bogged down with binging on TV shows and playing your favourite video games after a long week at work. We’ve all felt it before, the urge to just put our feet up for the weekend and chill. That’s okay every now and then, but we as humans need to move more, and hiking is a great way to do that. Other than a few initial costs with getting yourself a decent pair of walking boots and a backpack for all of your supplies, it’s basically a free activity. And, it comes with a heap of benefits. Read on to find out more. The advantages Hiking is primeval. We used to walk from food source to food source, building muscle mass and exposing our immune systems to pathogens on the way. Hence, it's great for our neurocognitive immune complex, which means it's good for our overall well-being. It's also a great exercise in bonding, parenting and mateship. South Coast Track, Tasmania (Dec 2019) The benefits of hiking include: • Increased muscle strength: Hiking is essentially walking, but tends to involve walking over different terrain which may range from flat forest pathways to rocky mountainous passes. Either way, getting yourself out and about is going to get those trunk and lower limb muscles engaged and pumping. This type of exercise will help to improve strength in your glutes, quads, hamstrings, calves and trunk muscles which will provide stability to your skeleton and joints, and help keep away potential joint problems like osteoarthritis.• Improved cardiovascular health: The planet is becoming more obese as each year passes, which is seeing an increase in heart-related disease. A great reason to try hiking as it could help you to control or lose weight, reducing stress on the cardiovascular system. Regular exercise of this type has been shown to lower blood pressure and blood-sugar levels, reducing the risk of developing heart disease and conditions like type-2 diabetes. Challenging yourself to walk up and down difficult terrain is a fantastic way to improve your aerobic fitness and keep everything in check.• Improved core stability and balance: Walking over rocky and uneven terrain is a great way to challenge those core stabilising muscles and work at improving your balance. Walking on flat, even surfaces doesn’t provide the body with that side to side component of movement that walking on an uneven surface can do.• Improved mental well-being: There is evidence that spending time in green, natural environments away from urban jungles can help to reduce stress levels in people. The outdoor, rural landscape can provide you with a sense of peace and quietness, calming the mind of all of life’s worries. This is something you just don’t realise when you are constantly in the hustle and bustle of city life where noise and pollution are rife throughout.• A chance to socialise: Humans are social beings. We like to engage with others (there are always exceptions to this rule!) and be with them to really enjoy the benefits of living. If family time is short mid-week because of work, school and other engagements, hiking gives you the perfect opportunity to be with the ones you love. You can talk, move and have fun together in a beautiful environment. What else do you need?! Ironbound Range, South Coast Track, Tasmania. (Dec 2019) Suggestions for hiking If we’ve said enough to get you on board (hooray!), there are a few little pointers we want to bring to your attention before you get going. 1. Get equipped: Ensure you get fitted with a good pair of walking boots, grab a backpack and if you are just starting out, a hiking stick or pole may be of benefit to help you through trickier terrain (especially if you have any knee issues).2. Pack water and food: Have enough with you to keep your energy and hydration levels up throughout your hike.3. Find a route that fits your abilities: If you are just beginning, we suggest you don’t go straight for the most mountainous route out there. Try an easy track or nature reserve walk before attempting K2 or Everest (you need extra training for these by the way!).4. Take a friend or family member: It’s sometimes good to get out on your own for ‘you’ time, but hiking is great when done with someone else. Having more than one person means that if you get injured or help is needed, you are not stranded alone with nowhere to turn to. Keeping in mind, some hikes may be in areas with little cellular reception. Invest in some kind of emergency beacon device eg Garmin InReach5. Let someone know you are going: It is safer to tell someone at home or a neighbour that you are heading out. The outdoors is sometimes unpredictable so letting someone know where you are going and when to expect you back is another safety measure worth having in place. South Coast Track, Tasmanai (Dec 2019) So what are you waiting for? Get out there and really enjoy what the world has to offer. We live on a beautiful planet, so make sure you get to experience it and improve your health whilst doing so. Ready. Set. HIKE! (You can reward yourself with an episode of your favourite show when you get back!) ........and if this isn't enough, later you can take on canyoning and rock climbing Blue Mountains, NSW, Australia (Jan 2020) Uploaded : 23 February 2020 Read More -

Sleep Deprivation and Muscle Recovery
Effects of Sleep Deprivation and Acute Muscle Recovery For many years sleep deprivation has been known to affect brain function, whereby 48-72 hours of sleep deprivation has been used as a means of torture. As in the famous novel by George Orwell, 1984, acute psychosis can be induced with sleep deprivation. Additionally, sleep deprivation can induce metabolic dysfunction including a blood spectrum similar to metabolic syndrome in otherwise young healthy individuals. Any of us who have undergone intense unfamiliar exercise know the uncomfortable feeling of DOMS (delayed onset muscle soreness) and restless sleep. A combination of lack of sleep, over-training and inadequate recovery can result in the 'three bastards in a day". Read to the end to know who these three bastards are. Taking into account the many layered affects of sleep deprivation, it should come as no surprise that muscles may also be affected. Dattilo et al (2020, Med Sc Sp Ex,52, 2, 507-514) examined the effect of total sleep deprivation on muscle recovery after eccentric exercise induced muscle damage(EEIMD). They found that, in 10 healthy untrained males, sleep deprivation did not affect muscle recovery but modifies inflammatory and hormonal response. More precisely, sleep deprivation increases blood IL-6 levels and modifies the blood hormone balance by increasing IGF-1, cortisol, and the total cortison/testosterone ratio. Significantly, acute IL-6 elevation is known to stimulate hypertrophic signalling and myogenesis through regulation of muscle stem cells. However, chronic elevation of IL-6 can be very detrimental to skeletal muscle such as seen in cachexia. Muscle damage alone stimulates an immune-nervous system response Normally functioning balance between pro-inflammatory and anti-inflammatory substances and neuro-immune modulation is referred to as allostasis An interesting hypothesis is how sleep deprivation affects the cognitive evaluation of 'danger signals' in the presence of heightened arousal in a 'milieu' of an already stimulated immune-hormonal response to muscle damage Commonly, the sympathetic nervous system is viewed in terms of the 'fight-flight' response to perceived and real danger. Top down modulation or conversely bottom up modulation? A Psychologist may think top-down whereas a physiotherapist, exercise physiologist or sports trainer should think in both directions, especially since we are muscle specialists. Commonly, over-training or over-reaching is associated with non-restorative sleep and nitrogen imbalance. This can affect catabolic processes such as those induced by cortisol and attenuate anabolic (muscle building) processes such as that induced by testosterone. Symptoms of over-training and sleep deprivation are nitrogen imbalance and the "three bastards in a day' rule. So who are these three bastards? If you meet a person who you really don't care to meet again, then that is fine. If you meet a second person like that on the same day, you might be very unlucky or in group company. If you meet a third person like this, and they aren't part of group, it's not them but you!!! Commonly, when people have asked me 'how do I know when I am in over-training?' I say, just ask your partner or spouse or have you met three bastards in a day lately??!!! Uploaded : 22 February 2020 Slides used are from a presentation I made at a conference in Rome in 2005. Read More -

The use of exercise therapy post cancer treatment to attenuate Doxorubicin-induced cardiotoxicity
Physiotherapeutic implications of exercise prescription in post cancer treatment to reduce Doxorubicin (DOX)-induced cardiotoxicity One of the complications of cancer treatment is the loss of weight. Some of this occurs due to the loss of appetite but also as a result of reduced volition to exercise. The therapeutic benefits of exercise include the improvement in muscle mass, which is important for maintaining a reservoir of protein, for the immune system. Additionally, the benefits of strength and endurance are reduced fatigue and enhanced functional capacity. Furthermore, improved oxidative capacity, through exercise, maintains healthy mitochondria, reducing oxidative stress. Animal models suggest that tumour bearing mice who are wheel exercised, have improved functional indices of cachexia, without mitigating tumour number or size (Brandon BN et al 2020, Med Sc Sp Ex, 52, 11, 2320-2330). These results weren't dependent upon exercise duration, but rather on exercise threshold. The use of Anthracylcines for chemotherapy have been commonly found to have cardiac complications. It is thought that a reduction in autophagy may be responsible. Autophagy is the process whereby lysosomes remove damaged cell material such as folded proteins, damaged lipids, dysfunctional organelles and even mitochondria. DOX induced cardiotoxicity may be due to dysfunction of this lysomal regulation. Evidence suggests that this may be due to the accumulation of Reactive Oxygen Species (ROS), especially NOX-2 (NADPH oxidase). Exercise has been shown to improve the bodies ability to 'mopp up' ROS. However, the period between the diagnosis and onset of chemotherapy is frequently short. Given the harrowing nature of cancer treatment, it is frequently unrealistic to ask someone to commence an exercise regime during this time. However, there has been a long held belief that life long exercise may not prevent cancer but may improve the persons tolerance to the side effects of treatment. Another, intriguing suggestion is that post treatment exercise could reduce the risk of cardiotoxicity. Lee et al (2020, Med Sc Sp Ex, 52, 1, 25-36) examined this notion in animals (mice). They found that exercise prevents DOX-induced tissue damage and apoptosis.Their findings included attenuation of extensive cytoplasmic vascuolization and loss of myofibrils, reduced cleavage of CASPASE 3 and reduced elevation of proapoptotic protein BNIP3. Finally a reduction in chemotherapy induced upregulation of the % of TUNEL cells was also observed. Exercise intervention also had profound effects on left ventricle autophagy with increases of LC3-II in parallel with p62 reduction. Additionally, exercise promotes mitochondrial turnover (mitophagy), as well as preventing oxidative damage by modulating NOX subunits and lowering IL-1Beta. This investigation by Lee et al (2020) demonstrates for the first time that the negative impact of multiple DOX treatment cycles can be attenuated through a post treatment exercise regime (albeit in mice). Extrapolation to humans would suggest that a graded exercise regime over a 4 -12 week period, including 4 weeks of pre-conditioning may be a useful adjunct in improving recovery from chemotherapy. Alternatively, Kirkham et al (2020, Med Sc Sp Ex, 52, 2, 278-286) have recommended 'chemotherapy-periodised' exercise to accommodate for cyclical variation in fatigue. Furthermore, suggestions have been made that exercise, such as walking, reduces the rate of recurrence by up to 57% in some cases of cancer, such as after radical prostatectomy (Richman et al 2011, Cancer Res, 71, 11, 3889-95; referenced by Swain et al 2020, Med Sc Sp Ex, 52, 2, 296-302) . A meta-analysis of individual patient data of 31 RCT's found significant beneficial effects of exercise on fatigue in patients with cancer. Moreover, supervised exercise intervention was found to be superior to unsupervised exercise (Van Vulpen et al 2020, Med Ex Sp Sc, 52, 2, 303-314). Further, some of the calming effects of exercise may also have a therapeutic effect, which hasn't been covered here. Uploaded : 22 Feb 2020 Updated : 24 November 2020 Banned by Google Adwords as they reckon physiotherapists aren't allowed to discuss exercise in people receiving cancer treatment!!!! Go Figure!!!!??? Read More -

Ketogenic diets and Exercise
Ketogenic diets and Exercise Ketogenic diets have become popular in the decade of the teens. It involves fasting up to 16 - 18 hours between meals (Dinner at 7 and lunch the following day at 1pm) as well as maintaining a strict low carbohydrate diet. In principle, this methodology, similar to repeated acute bouts of exercise, presumably encourages the fat mobilising/oxidative pathways whilst sparing glucose. Although, investigations into liver metabolic pathways to ketogenic diet and exercise, in mice, have shown them not to be additive, they have found both enhanced liver enzymes and pancreatic enzymes used to metabolise fat (Huang et al 2020, Med Sc Sp Ex, 52,1 37-48). Anecdotal evidence suggest that this glycogen sparing diet can be beneficial even in ultra-endurance type of events. When working at high intensities, carbohydrates provide the most efficient source of fuel for ATP per volume of oxygen, in the mitochondria. The size of carbohydrate stores are limited, however they can be acutely manipulated, expecially in prolongied sustained or high intensity exercise, maintenance of carbohydrate availability enhances performance. Carbohydrate plays direct and indirect roles in the muscles adaptation to training. An example of the latter is the commencement of a second bout of training before the restoration of carbohydrate stores results in a co-ordinated up-regulation of the transcriptional and post transcriptionsl responses to exercise. Additionally, carbohydrate restriction during exercise can alter and improve mitochondrial oxidation of lipids. Periodization of training and of carbohydrate loading and unloading are techniques used to manipulate athletes performance. Short term restriction of carbohydrate (CHO), when using a ketogenic diet, were shown to effect iron deficiences via the modulation of interleukin-6 (IL-6) and hepcidin levels. Acutely, the iron levels of a ketogenic diet were lower than in the CHO rich group. This may be partly due to the removal of the large iron content in the western CHO rich diet, but also as a result of a positive change to functional iron use such as increased erythropoiesis, DNA synthesis, and oxidative enzyme production. After a 3 week adaption of elite walkers to a ketogenic diet, the CHO rich diet group showed a greater decrement to serum ferritin despite greater IL-6 and hepcidin responses in the ketogenic diet group (McKay et al Med Sc Sp Ex, 51, 3, 548-555). Such a paradoxical response suggests the need to periodically check ferritin levels. Patency of blood vessels may be critical to good joint health. Elevated cholesterol levels are thought to affect blood vessel patency, as the formation of plaques within the vessels results in the relationship of blood particle number (Reynolds Number) and blood flow becoming critical causing stasis and end vessel infarction. The articular joints tend to be at the end of the line for blood vessels and hence their small diameter may be critically compromised by elevated cholesterol levels. Hence, supplementation with anti-cholesterol agents such as 1000mg of EPA and DHA in Fish Oil, the use of Co-enzyme Q10 may go some way to mitigating the effects of cholesterol. Uploaded : 18 Feb 2020 Read More -

How to be productive in the gym
How to be productive in the gym We’re a time-poor world these days and unfortunately for a lot of people, spending time looking after their bodies is not always a priority. Whether it’s because their lives are packed with work, families or a busy social calendar, most people get very little ‘me’ time. Even for those who do ‘gym it’, we regularly see an attitude of get in, get it done and get out in time to take the kids to gymnastics. We regularly get asked what a person can do to maximise their time in the gym, and lucky for you – that is exactly what this blog is about! We appreciate that life is busy, but read on for some handy tips on keeping a productive gym schedule: • Go with a friend or family member: Many people hate going to the gym alone because they find it hard to motivate themselves. Having a gym partner means you can motivate each other during those really hard slogs on the exercise bike or pushing for that last rep. If you’re time poor, this allows you to kill two birds with one stone by getting in some socialising whilst working out (no animals were hurt during the writing of this blog). • Get a P.T: What better way to be productive in the gym than having a personal trainer to guide you along the way and keep you motivated. You’ll also have the benefit of having someone there to offer advice on technique, so you avoid injury. Obviously PTs cost money, but if you can’t afford a one-on-one, think about small group classes, where you still have personalized attention, but with less impact on the wallet.• Sign up for a class: There are heaps of class types out there to cover all bases of exercise. Try a HIIT class (which stands for High-Intensity-Interval-Training) if you’re after a big calorie burn in a short space of time.• Train smart: If you want to maximise the burn and time is short, then be smart with your exercise choices. Choose an exercise that targets several muscle groups (i.e. squats into overhead press), or perform two exercises that focus on the same or different muscle groups, one after the other (called ‘super-setting’ - i.e. squats then lunges, or squats then push-ups).• Avoid peak times of business: Hit the gym during a quiet time to avoid having to deal with long queues for equipment, allowing you to get your routine done in minimal time.• Have a plan: If you know what you are doing before you go to the gym then you’ll be less likely to find yourself wandering around between exercises mulling over what to do next. Write down your routine on paper so you can tick off the list as you go along.• Have water on hand: We recommend having your favourite, eco-friendly water bottle with you at all times. Keeping hydrated throughout will mean you’ll be able to see your routine through to the end without having to stop several times to queue for the water dispenser.• Switch devices to airplane mode: Text messages, emails and phone calls are potential distractions from your workout. Simply switch to airplane mode and you’ll be working out distraction-free, which means more time for dedicated exercise.• Listen to music: Music has been shown to enhance people’s performance during exercise. It’s personal preference but if you’re looking for motivation, having a playlist of up-tempo tracks could be just what you need to keep the energy levels up. We hope these handy tips mean your future gym sessions will now be as productive as possible. And if you’ve held off from the gym in the past because of a lack of time, we hope we have convinced you that time doesn’t have to be a factor if you’re organised. Hit us up at Back in Business Physiotherapy if you have any further questions. See you next month! Uploaded : 4 February 2020 Read More -

How to protect muscles as we age
How to protect muscles as we age Welcome readers! This month we are going to talk to you about an important subject we all need to think about as we get older. The health of our muscles is important as we move through life into our later years. The body is made up of a host of different systems: the nervous, vascular and musculoskeletal systems are all examples. The skeleton is made up of bones that fit together forming joints. Muscles attach to bones and provide movement at the joints, all under supervision of the vascular (i.e. the ‘blood’ system) and immune-nervous system (i.e. muscles, the brain, spinal cord and nerves). It’s a little bit more complicated than that, but you get the gist. Our bodies rely on movement for countless different internal processes to occur, and for us to maintain function and be able to get around and stay alive. Movement keeps our bones strong, our digestion and toilet habits regular, and provides the force required for fluids to move around the body, just to name a few examples. If you look at an average person’s lifespan, we grow and get bigger and stronger until the age of 30 (give or take). After this, if we don’t work towards keeping it all, we start to lose muscle mass, bone strength and joint health, which forces our body to decline as we reach the elder years. Naturally, we start to move less and our injuries, stiffness and pain increase… Joyous thoughts I know, sorry! But… It doesn’t have to be all doom and gloom. If we spend time on our bodies throughout life, exercising, feeding it the right stuff and living a stress-less approach each day, it is very possible to move into our later years with a good body that will keep us moving well. If we take control of our bodies early on and not abuse them, it gives us the best opportunity to have a problem-free life down the line. Goodbye expensive medical bills. How nice would it be to not have to rely on our private health insurance or Medicare services?! Food for thought. Let’s recap… Muscles are movers, and we need movement to be healthy and alive. So naturally, we need to look after our muscles. “What can we do?" I hear you ask. The answer is, LOTS! • Exercise regularly: In order for our muscles to stay strong, we need to use them. The saying goes ‘if you don’t use them, you lose them’. And this is very true. Look at someone who has broken their leg and are immobilised in a cast for a six-week period. Once the cast comes off, look at the size of their muscles on that leg compared to the non-injured side. Through lack of use, the muscles have got smaller and weaker (i.e. they have ‘atrophied’). Losing muscle due to aging is a slightly different process (known as ‘sarcopenia’), but the same rules apply… If you want to increase the size and strength of your muscles, you need to be doing some regular and progressive resistance training. Whether you are using your own bodyweight, resistance bands or free weights, to be progressive means to increase gradually. In this context, you can gradually increase weight or the number of repetitions or sets in order to gain strength and continue to do so. Remember that in order for muscles to get stronger, they also need rest and recuperation, so be sure to include rest days in your plan. • Look at your diet: So you’ve ticked off regular exercise and now you need to tick off a healthy diet to back up all the good work you do getting your pump on. A muscles favourite food is protein. When we eat protein, our body breaks it down into smaller pieces (called ‘amino acids’) which our body uses to build muscle tissue. It is a good idea to give your body a protein boost following your resistance exercise routine, but if you aim to take on protein with each meal in some form, then you should be giving the muscles the food they need. You have many options… We recommend getting a good mix of fish, poultry, yoghurt, milk, cheese and eggs to ensure you hit the protein goal each day. Beans, peas, nuts and seeds are also a great source of protein. • Drink lots of water: A piece of advice we will keep coming back to time after time. It is simply a must for everyone, every single day. Our bodies are predominantly water and pretty much every process carried out inside the body needs it in order to function. The muscles are no different. Muscle tissue is full of blood. It relies on the blood to feed it all the nutrients it needs to stay healthy and to continue strengthening. Blood is largely made up of water (shocking I know!), so stay hydrated for good blood. Good blood equals a good transport system for food to get to the muscles. This is our advice to you. We know it is tough trying to figure all this out on your own, but the good news is, you are not alone… Our team here at Back in Business Physiotherapy are here to answer any queries you may have about your body and how to age as gracefully as possible. Although the body is a very complex machine, it’s not rocket science when it comes to looking after it. Just be kind to it every day and let us worry about the scientific stuff. This is what we spent years studying for. For more detailed information on improving your muscle health for the future, including exercise and dietary advice, please call us on +61299226806 to make an appointment. P.s. Please remember to drink water every day (this won’t be the last time you read this!). Further Reading : Sarcopenia and aging (Rome Presentation) Exercise, physiotherapy, deterministic chaos and the immune system Uploaded :4 February 2020 Read More -

Resistance workouts for bone health
Resistance workouts for bone health Hello everyone! We hope you have had a fantastic break and are raring to go for 2020. We’re go-ing to kick off proceedings this year with a blog topic we think is becoming more and more im-portant. It’s no secret that people are living longer and with an ageing population comes higher rates of certain conditions and diseases, such as osteoarthritis (i.e. the degeneration of joints) and osteoporosis (i.e. weakening of the bones). Did you know that exercise is good for the bones and can help keep your skeleton strong as you age? Read on to find out more… Good news people, exercise is great for bone health! In fact, it is widely accepted that exercise is one of the most effective ways of keeping your bones strong and healthy. So, there you have it. Say no more. Blog ends… Just kidding! We’ll give you a bit more than that 😉. There are several different types of exercise, and while all types will benefit your body in some way, if you want to target bone health and par-ticularly strength, then resistance type exercises are up there as some of the best. What is resistance exercise? Resistance exercise is any exercise that has the body working against an external force and will often involve the use of fitness equipment including weights (either free or machine weights), re-sistance bands, cables and medicine balls. Different examples of resistance exercises include: • Pushing against a wall• A weighted bicep curl or lunge• Banded or cable shoulder strengthening• Riding on a static bike with varying intensities Why resistance exercise? So why resistance over other types of exercise we hear you ask? Quite simply, when we exer-cise, we place forces or loads on the body which help to build our muscles which in turn place stress on the skeleton (remember, muscles attach to bones via tendons). This stress placed on the skeleton is what is needed to activate the bone building cells of the body (they are called ‘os-teoblasts’ if you really want to know). Some forms of exercise lead to lots of activation of these cells, other forms to a lesser degree. Performing our everyday activities such as washing, walking, cooking and dressing is not enough to create lots of cell activation, so keeping ourselves working at this level will not necessarily build strength in our bones (although it may help them from becoming weak - a good reason to not be a couch potato). If we want to build bone, then we need to regularly exert ourselves over the limit of everyday life tasks. This is where exercise and especially the resistance type comes into play. Resistance exercise will place a variety of force on the skeleton through the muscular system, and therefore lead to increased bone cell activation and eventually stronger bones. Will other types of exercise help my bones too? As we mentioned above, different exercises lead to different bone cell activation rates. Re-sistance exercise is not the only type that is good for building bone strength. Other examples in-clude stair climbing, hill walking and high impact exercises such as basketball and aerobics. Whilst swimming is an awesome form of exercise for the body, it has been shown to be less ef-fective at building bone strength, even though the water provides some resistance against the body as you swim. Good to know! The type of exercise you do will also be dependent on many things. Age, for example, is a big factor. Someone who is elderly and has a history of bone fractures due to osteoporosis would not be put on a program of heavy weightlifting. However, they could very much benefit from perform-ing regular light banded or cable exercises, combined with walking or gentle dancing. Whereas a middle-aged person with good fitness levels could benefit from a more intense weight program to ensure good bone health in their later years. Bones need more than just exercise It is important to remember that bone health is dependent on more than just exercise. Having a good diet which includes adequate amounts of vitamins and minerals is also a must. If you didn’t know already, Vitamin D and Calcium are two nutrients which are very important for ensuring your bones stay healthy from birth, all the way into your wise years. Get what you need by mak-ing sure you include a regular intake of spinach, kale, salmon, mackerel, cheese and milk. Many breakfast cereals will often have these nutrients added to them too. So, don’t skip your breakfast people! To conclude… The bottom line is bones need exercise to stay healthy for life. If you are unsure of what is right for you, then we are only a stone’s throw away. Please call us on 02 9922 6806 to make an ap-pointment and we’ll be happy to design a resistance program that will be unique to you and your needs. Now go and get your best gym lycra out and get ready for strong bones! References: 1. Hong, AR. and Kim, SW. 2018. Effects of resistance exercise on bone health. Endocrinology and metabolism. 33 (4). 435-444. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279907/2. Benedetti, MG. et al. 2018. The effectiveness of physical exercise on bone density in osteo-porotic patients. BioMed research international. v. 2018, 4840531, 10 pages. Available from: https://www.hindawi.com/journals/bmri/2018/4840531/cta/3. Osteoporosis Australia. 2013. Exercise - consumer guide. [Online]. Available from: https://www.osteoporosis.org.au/sites/default/files/files/Exercise%20Fact%20Sheet%202nd%20Edition.pdf. [Accessed 12 Dec 2019]4. WebMD. 2019. Top foods for calcium and vitamin D. [Online]. Available from: https://www.webmd.com/food-recipes/guide/calcium-vitamin-d-foods. [Accessed 13 Dec 2019] Uploaded : 20 December 2019 Read More -

High Intensity Interval Training (HIIT)
HIIT workouts for all Alright people, it’s a new year which means it’s time to get a move on and start ticking off those resolutions. We know for a lot of us this will include exercising more, getting healthy, or losing weight. And we also know for most of us, once normality resumes, it will be the same old story of not having enough time in the day to do it. Well we may have a solution for you! HIIT stands for? High-intensity interval training. And if you are one of those time poor people we described above, this type of training could be just what you are looking for. It’s a form of exercise that has become incredibly popular in recent years and is a great way for people to get their burn on, within a short space of time. So, if you can barely find time to think between kids, work, cooking, washing and sleeping (hang on… there is such thing as sleeping???), then read on to learn more. What is HIIT? HIIT is a type of workout that follows a repeated pattern of vigorous exercise over a short time period, followed by a rest or recovery period of less vigorous exercise. This repeated pattern will usually take place over a period of up to 30 minutes. Thirty minutes is all you need! And it has been shown that the effects on the body after performing this type of exercise are similar to that of double the amount of medium-intensity exercise. Starting to see why it is so popular? Let’s give you a little example of what you could do. Try running as fast as possible on an inclined treadmill for 30-40 seconds, followed by a light jog with no incline for 4-5 minutes. Repeat for 30 minutes. Sounds hard, right? Well it is, but that’s OK. You’ll feel goooood afterwards! What are the benefits of HIIT? There are several positive effects of HIIT on the body. These include: High calorie burn - you’re sure to burn loads of calories even when performed over a short period of time Increased metabolism - you’ll keep burning those calories for hours after you’ve finished exercising due to the boost your metabolism will get doing HIIT Fat loss - HIIT can help you reduce fat from your body, including fat that may have developed around your organs (i.e. ’visceral fat’) Reduced heart rate and blood pressure - this has been shown more in the overweight and obese population. HIIT can help to improve your cardiovascular health! Reduced blood sugar - this has been shown when performed consistently over a long period of time. This is particularly great news for the diabetic population Improved use of oxygen - regular HIIT workouts will help to improve your muscles ability to use oxygen, similar to the effects that you get from running or cycling over a long period Muscle and strength gains - although not the best way to gain muscle and strength, depending on the type of exercise you perform, you may also notice some gains in this region too Sound good? We think it does, so why not give it a try? If time is always an issue, then this is worth a shot. Please always consider your health and level of fitness before trying new forms of exercise. We recommend talking to one of us at Back in Business Physiotherapy if you are thinking of starting up a HIIT program of your own. We can assess you and advise you on a safe workout that isn’t going to send you straight right back to us with a new injury. It’s time to burn! Who’s ready? References 1. Kong, Z. et al. 2016. Comparison of High-Intensity Interval Training and Moderate-to-Vigorous Continuous Training for Cardiometabolic Health and Exercise Enjoyment in Obese Young Women: A Randomized Controlled Trial. PLoS One. 11 (7). e0158589. Available from: https://www.ncbi.nlm.nih.gov/pubmed/273680572. Skutnik, BC. et al. 2016. The Effect of Low Volume Interval Training on Resting Blood Pressure in Pre-hypertensive Subjects: A Preliminary Study. Phys Sportsmed. 44 (2). 177-183. Available from: https://www.ncbi.nlm.nih.gov/pubmed/269188463. Healthline. 2017. 7 Benefits of High-Intensity Interval Training (HIIT). [Online]. Available from: https://www.healthline.com/nutrition/benefits-of-hiit. [Accessed 13 Dec 2019]4. Batacan, RB. et al. 2017. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 51. 494-503. Available from: https://bjsm.bmj.com/content/51/6/494.short Uploaded : 19 December 2019 Read More -

Common soft tissue injuries
Common soft tissue injuries We are nearing the end of the year here in Australia, which means the sun is heating up and people are starting to get outdoors a little more. It’s at this time of the year lots of people head into the gym in search of a better body. Unfortunately for some, this can mean an increased risk of injury, which is no fun for anyone, especially at Christmas. We’re here to give you a little run down on some common injuries we see here at Back in Business Physiotherapy. This blog will concentrate on injuries related to ‘soft’ tissues… Namely muscles, tendons and ligaments Floppies vs Stiffies The soft tissue is made up of collagen. A triple helix amino acid protein complex, accounting for about 25% of the protein in the body. Genetically determined variations in collagen types, especially the extracellular matrix complex of cross bridges of collagen can determine the strength and elasticity of soft tissue. Due to the inhereted nature of collagen, there are essentially two types of people - the 'floppies' and the 'stiffies'. The 'floppies' are people who are hypermobile, partake in sports requiring flexibility and agility such as gymnastics, ballet, swimming, short distance track and field events or events which require speed and power. The 'stiffies' tend to participate in long distance land based endurance events, such as marathons, where speed, power and flexibility aren't an absolute requirement, but where postural stability is paramount. Thus 'floppies' tend to have a high proportion of type II white sprint muscles fibres, as opposed to the type I red slow twitch endurance muscles. Biomechanically, longer more elastic muscles have better recoil but also greater displacement to create maximum velocity (v = disp/time) and hence power (P=Force x velocity). Ironically, you will find the 'floppies' in the yoga class and 'stiffies' in the Pilates class when, if you wish to avaoid injuries, it should be the reverse.....but your average 'stiffy' will be intimidated by the yoga class. In the animal kingdom the tortoise and the hare might be a good example or the Painted African Wild Dog vs the Springbok? African hunting dog can run at 44 mph and cover long distances (770 sq miles) The Springbok can jump very long distances and sprints well. Thus 'floppies' need to be highly co-ordinated and have ballastic stability to avoid injury, whereas the 'stiffies' need flexibility to avoid injuries. In the off season or during the recovery phase of their training cycle, both groups should be encouraged to develop the opposite muscle fibre types to what they naturally tend to, in order to avoid injuries Muscle strain A muscle is made up of groups of tiny little fibres that shorten and lengthen to create movement around a joint. Muscles are flexible tissues that can withstand and create a lot of force. Sometimes movement can place excessive load through a muscle and some or all of the fibres within it can tear. Tearing of muscle fibres is known as a ‘strain’. A muscle will commonly strain when it is overstretched. Think of a soccer player reaching a leg out for the ball, or a gymnast kicking their leg over their head. If the muscle is not able to cope with the demands of the stretch, then the only option is for the muscle to tear. A strain is graded based on the severity of the tearing: Grade 1 - a few muscle fibres are torn, similar to unaccustomed exercise strain 24-48 hours post exercise. Grade 2 - more muscle fibre damage with pain lasting beyond 72 hours. 28 day lunar cycle for recovery. Grade 3 - extensive damage to muscle fibres, but not completely torn, Can take up to 6-8 months to recover from. Grade 4 - all fibres are torn. Catastrophic and may need surgey. Common symptoms of a strain include pain, swelling, bruising, loss of function and weakness. The range of symptoms depend completely on the severity of the strain. A low-grade strain is often painful with minimal loss to function and strength. A high-grade strain is often very painful with swelling, bruising, complete loss of strength and reduced function in the affected body part. Ligament sprain A ligament is a strong band of tissue that joins a bone to a bone, creating a joint. Ligaments provide stability at a joint, making them quite inflexible compared to muscles. They have to withstand extremely large forces that run through the body when we move. Therefore, it makes sense that it requires a very large force to injure one. Take a rugby player who gets tackled with their foot firmly planted on the ground as the opposition player runs into the side of their legs. The excessive force of the tackle on the knee could cause the ligaments to overstretch or tear. Tearing of a ligament is referred to as a ‘sprain’. Just like a muscle, a ligament injury is graded from one to three: Grade 1 - the ligament is overstretched but remains intact Grade 2 - some ligament fibres are torn, some remain intact Grade 3 - all fibres are torn Ligaments have a very poor blood supply compared to muscles which means they take longer to heal. If you look at muscle tissue it takes on a reddish appearance (i.e. a rich blood supply), compared to the silvery white colour of ligament tissue. Symptoms of a ligament injury again depend on the severity of the injury and include pain, swelling, bruising, loss of function at the joint, and joint instability… You may well feel a little wobbly on your feet following a severe knee or ankle sprain. Tendinopathy A tendon is what joins a muscle to a bone. It is similar in make up to a ligament in that it also has a much poorer blood supply when compared to a muscle. Tendon injury is referred to as tendinopathy and is usually broken down into acute inflammation of a tendon (called ‘tendinitis’) and chronic degeneration of a tendon (called ‘tendinosis’). Tendons are often injured due to overuse of a body part due to repetitive actions, such as throwing in baseball. Overuse of the tendon can lead to very small tears developing. If complete healing is not achieved before re-injury, the problem can progress. A single large force put through a tendon can result in an acute episode of pain and inflammation. If a force is large enough, or a tendon has become degenerated over time, it is possible for the tendon to tear in part, or completely. Symptoms of tendon injury include pain (often before and after activity), possible swelling, and reduced function and weakness of the affected body part. Because of the poor blood supply, tendons, like ligaments, can take quite some time to heal fully. Many tendon injuries are associated with a bursa. The bursa frequently has been shown to involve a metabolic - immune dysfunction in association with the tendinopathy. Common bursa include the Sub-Acromial bursa in the shoulder, the Calcaneal bursa at the Achilles heel, the Hamstring insertional bursa at the sitting bone and the Greater Trochanteric bursa of the hip. Management of a mid substance Achilles Tendonosis or paratendonosis is very different to that when the Calcaneal bursa is involved. Treatment and prevention of injury Each one of the injury types above is managed differently, and healing time depends on the severity. With any acute injury you’re pretty safe following the RICER protocol from the off (remember rest, ice, compression, elevation and referral). However, we recommend you get in touch with your us straight away because we will be able to get our hands on you to start treatment, as well as give advice on the whole rehab process. It is especially important to know when to begin putting load through the injured tissues again to ensure you decrease your healing time and any potential after-effects of the injury. Remember that prevention is always better than cure. We recommend you always warm up before performing your activity. A good rule to follow is warm up with exercises that are going to prepare your body for the activity you are about to perform… For soccer, warm up with ball drills, light jogging, short sprints, jumps and dynamic stretches (i.e. stretches with movement). It’s best to save your static stretches (i.e. held stretches) for your post-match cool down! If you need help with an injury or want further advice on how to prevent injury in the future, call our clinic on 02 9922 6806 or speak to your physio during your next session. References 1. Physiopedia. 2019. Muscle strain. [Online]. Available from: https://www.physio-pedia.com/Muscle_Strain. [Accessed 5 Nov 2019]2. Physiopedia. 2019. Ligament sprain. [Online]. Available from: https://www.physio-pedia.com/Ligament_Sprain. [Accessed 5 Nov 2019]3. Brukner, P. and Khan, K. 2017. Clinical Sports Medicine. 5th ed. McGraw Hill Education : Australia Uploaded : 22 November 2019 Updated : 26 November 2019 Read More -

An unusual case - femoral artery compression
Sports Physiotherapy Clinical Reasoning : An unusual case - femoral artery compromise A 23 year old female cyclist presented with a 2 week worsening history of severe anterior and posterior hip pain when sitting, intermittent 'giving way' and 'loss of power' in the knee, especially worse going up stairs and going from sitting to standing. She reported a minor fall onto her right side a few weeks previously whilst mountain biking. Otherwise, no previous history of any specific injury to that area, however a few major falls off bikes over the years, but nothing serious enough to require hospitalisation or on-going treatment. Examination revealed a clinically stable knee. Step ups were described as weak but no 'giving way'. Knee extension strength was reduced. Sciatic nerve mobility testing was within normal limits. Hip flexion was uncomfortable but didn't reproduce the intense pain which she was describing. Ranges of motion testing of the hip, in flexion,were otherwise unremarkable. Gaenslen's testing in hip extension revealed some limitation of the Psoas Major and Rectus Femoris. Patrick FABER's testing was full range as were other hip and SIJ tests Prone Knee Bend testing for femoral nerve demonstrated some restriction in movement as well as some sensitivity and restricted movement in the upper lumbar spine At this stage of the clinical reasoning process, things weren't getting any clearer. I noted previously that the foot seemed a little cold, I then asked her to return to supine, where i questioned her on any recent plane travel. An adventure racing friend of mine had a pulmonary emboli from a DVT in the abdominal region after spending time at altitude in Tibet and then flying home to Switzerland. I also quizzed her on any Leyden's Factor V or other clotting issues either diagnosed in herself or in someone in the family. I tested the femoral pulse superior to the inguinal ligament and it seemed quite strong. She was not taking anti-coagulants but was on the contraceptive pill. I decided to treat L1-L3 with joint mobilisations and the anterior hip with various techniques, including soft tissue massage, trigger points to the iliacus, quadriceps and adductors. Hip traction at 90 degrees flexion 'felt good'.The combined treatment improved the quads strength. However, I still didn't feel convinced that either the history or the physical examination and treatment had really explained the symptoms. Five days later I received a phone call from her where she said she was falling frequently and that she could not sit due to extreme pain. I suggested to go to accident and emergency since the situation sounded desperate. Several tests were conducted, including a CT to the abdominal cavity and a doppler ultrasound which revealed a mass pressing on the femoral nerve and artery. Emergency surgery was peformed where a haematoma was discovered. This was evacuated resulting in an almost full immediate recovery. Some loss of quads strength was still evident 6 weeks later but was purely clinical. Reviewing the literature revealed this to be a rare clinical presentation in the absence of taking anti-coagulant medication. When it did present, it was most common post surgically or in young adults and adolescents. "Compression of the femoral nerve secondary to iliacus haematoma is widely reported in patients with blood coagulation disorders and those on anticoagulant treatment. Femoral nerve palsy caused by traumatic iliacus haematoma in the absence of bleeding diathesis has not been reported widely in the literature. All published reports occurred in young patients aged between 12 and 24 years and most cases were precipitated by a traumatic injury while participating in sport. Haematomas in this region present insidiously and are not heralded by an obvious lesion or ecchymosis. Patients initially complain of groin pain with the onset of neurological symptoms occurring as late as 10 days following the injury. The differential diagnosis for this syndrome is large and early recognition requires a high level of suspicion. A simple muscular strain is a common diagnosis in young athletes and can mimic iliacus haematoma in the early stages, and is regularly treated with non-steroidal anti-inflammatory drugs. These drugs have been implicated in the progression of the haematoma in a number of published cases. The most common mechanism of injury in reported cases is a fall onto the back or buttocks, although more indolent precipitating injuries are described. Direct trauma to the pelvis or hyperextension of the hip may result in muscular tears leading to iliacus haematoma. Two separate syndromes of lumboscacral plexus compression are recognised. The entire plexus can be compressed within the psoas muscle resulting in weakness of those muscles supplied by the obturator and femoral nerves. Alternatively, the femoral nerve is compressed as it passes through the closed fibrous compartment formed by the iliac fascia and the ileum." Murray et al (2010) ttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC3027788/ Uploaded : 2 November 2019 Read More -

Tape, tape and more tape!
Tape, tape and more tape! Have you ever been to see your physio and left with some additions stuck on your skin? Taping is a very popular technique used by physios in the treatment and prevention of musculoskeletal injuries. There are various types of tape, ranging from rigid to more flexible kinesiology (you may hear this referred to as K-tape) or active tapes. Here is the low-down on some different types you might come across during your time with your physiotherapist. Rigid strapping tape This is one of the most common and more conventional forms of tape used by physios globally. As the name suggests, it is rigid (i.e. it does not stretch). It is usually light brown or beige and is designed to hold firm, making it ideal for providing support or stability to a joint. Let's give you an example… A footy player has rolled their ankle and is returning to training after an intensive rehab period. Their physio may decide to apply rigid tape around their ankle for a few reasons; it will provide a barrier stopping the ankle from rolling again, but will also give the player confidence and an ability to play without fear of re-injury. It won’t be the aim of their physio to keep applying it every time they play, but it may be beneficial in the short term while the player is still working on match fitness. Other common areas of the body where it’s used include: • Across the front of the knee to aid with kneecap alignment during movement• Under the arch of the foot for people with flat feet that require extra support• In the management of pretty much any ligament injury in the knees, shoulders, fingers, ankles and feet Sports Tape This tape is a fairly rigid tape but has some degree of elasticity (approx 6%), which makes it a good tape for boney curvey regions of the body or where larger ranges of movement are required. Dynamic Tape This tape was developed by a physiotherapist on Norfolk Island which is an Australian external territory and island in the Pacific Ocean located between Australia, New Zealand, and New Caledonia, 1,412 kilometres from the mainland. It has exceptional elasticity (apprx 60%) and is very useful in areas of swelling. Kinesiology or K-tape This tape has been developed in more recent years and is pretty much the opposite to rigid tape. This is very stretchy (approx 30% elasticity) making it pretty useless at providing stability to a joint, but it does have some very cool functions. It comes in a range of colours for no other reason than to allow a player or patient choice over which colour they prefer. Choosing a pink one over a blue one doesn’t mean you’ll get anything extra from it… They are all the same (we thought we should clear that up!). However, Japanese practitoners believe the different colours absorb different energy and hence maybe used where temperature and energy levels are part of the practitioners reasoning process. K-tape may be used for the following reasons: • To provide moderate support to joints and muscles whilst allowing free range of motion and relieving pain. • When applied stretched over the skin, it creates a puckering effect lifting skin away from underlying tissue - this can be very beneficial in aiding blood flow and drainage of fluid from one region to another. It is also used to aid in myofascial release techniques and is often applied with the joint and muscles in the stretched position. • When applied to the skin over an injured joint, it can provide information to the brain about what the joint is doing and allow for increased muscle activation in the area. Hypoallergenic underlay Some people are sensitive to the glue used on certain tapes, in the same way people are sensitive to band-aids or plasters. In these instances, your physio will use a hypoallergenic underlay or wrap protecting the skin from glue, meaning those people who are allergic or sensitive can still get benefit from taping. Unless they are allergic to hypoallergenic tape as well, which some people are! These are by no means the only types of tape out there, but they are some of the most commonly used. There are some newer types of tape available now, including active or functional tape. This type of tape is similar to K-tape but will stretch more and is stronger and more elastic. It is particularly useful in offloading injured muscles and tendons and aiding with pain relief and recovery. Next time you are in the clinic, feel free to ask us about different types of tape. We will be in our element explaining what they are used for, and if warranted, will show you firsthand how it works! References 1. Brukner, P. and Khan, K. 2017. Clinical Sports Medicine. 5th ed. McGraw Hill Education: Australia2. Rock Tape. 2019. How it works. [Online]. Available from: https://rocktape.com.au/how-it-works/. [Accessed 09 October 2019]3. Strapit Medical Sports Supplies. 2019. Gripit activetape. [Online]. Available from: https://www.strapit.com.au/products/active-tapes/gripit-activetape-75mm-314. [Accessed 09 October 2019] Uploaded : 22 October 2019 Read More -

Ankle Sprains
Rolled your ankle? Have you ever rolled your ankle? Plenty of us have, especially people who partake in sports such as netball, basketball, volleyball, football and soccer, where ankle injuries are one of the most common injuries of all. These sports all involve pivoting, quick changes of direction, jumping and landing. The classic ankle injury involves rolling your ankle during landing on an uneven surface from a jump, or lunging for a ball during a tackle, where your foot rolls inwards and your leg outwards upon contact with the ground. About ligaments Our ankles are stabilised either side by an outside and inside ligament (tissues that attach bone to bone). The inside (medial) ligament is much stronger than the outside (lateral) one, therefore injuries to these ligaments where you roll your foot outwards, are much less common. The outside ligament is made up of three parts - front, middle and back. The front part of the ligament is the weakest and is usually the most affected in ‘rolling’ injuries. With more severe injuries, it is possible to affect the other parts too. What happens when I roll my ankle? When you roll your ankle, forces placed on the outside ligaments may be too great, and the ligament will sprain. A sprain is broadly categorised into three grades:• Grade 1 - the ligament is overstretched but not torn• Grade 2 - the ligament is partially torn with some ligament fibres still intact• Grade 3 - the ligament is completely torn (also known as a ‘complete rupture’) Signs & symptoms As with most ligament injuries, it starts with a moment where too much strain or force is put through the joint/ligaments, and you feel something give. This is usually painful and may or may not be accompanied by a ‘pop’, which usually signifies that something has torn. Depending on the severity of the injury, you may start to see swelling and bruising appear quickly, or it may take time to develop. Either way, bruising is another sign something has torn and bleeding has occurred under the skin. Whether you can put weight through the joint and walk straight after injury is an important part of the process. If you can, this tends to indicate a less severe injury. If you can’t and require help to move off the field or court, this may mean something more serious has happened, like a fracture alongside a sprain. If this is suspected by your physio, you may be sent off for x-rays to confirm. Immediate treatment It is important that the injury is managed well from the word go to ensure a speedy and hassle-free recovery. The first goal is to protect the joint from further injury. Depending on severity, this may require you to be off your feet for a short period, so crutches may be needed. Additionally, the use of an aircast may be required. After this, it is recommended to start putting weight through the joint to help reduce swelling and increase movement. Ice, compression and elevation are also recommended in these early stages. If it turns out you have a fracture too, there will be a short period of immobilisation in a moon boot to allow the fracture to heal. Further treatment and return to play After the acute period is over and your swelling and pain are controlled, your physio will get to work on your ankle. You would have lost range of motion of the joints, so they will mobilise them and give you exercises to keep mobilising at home between treatments. You would have lost some strength as well, so you will need to strengthen the surrounding muscles, as well as work on other aspects of fitness including balance. During this period, you will get back to full weight bearing activities starting with walking and moving through to jogging, running, jumping and landing, adding agility exercises to retrain the ankles' ability to pivot and change direction without giving out on you again. You’ll need to complete some rigorous training before your physio clears you to return to the field of play to compete. The time it takes you to get back playing will depend on the severity of your injury, with a simple low-grade sprain taking anywhere from 2-4 weeks to heal, and a severe sprain and fracture taking months. The latter is particularly true if there is a tear of the syndesmosis and/or a Weber Fracture. Weber Fracture Syndesmosis tears (picture c) can easily be missed and minor fractures of the malleolus can masquerade as acute tendonosis. Tears of the syndesmosis can lead to a chronically unstable ankle. These conditions are often treated in a moon boot, but occassionally surgical intervention is necessary. Take action If you have rolled your ankle and need some help to get back to the field or court, then look no further. Call us today on 02 9922 6806 to book your appointment, and we’ll have you hopping, skipping and jumping in no time at all! References 1. Brukner, P. and Khan, K. 2017. Clinical Sports Medicine. 5th ed. McGraw Hill Education : Australia2. Chen, ET. et al. 2019. Ankle sprains: Evaluation, rehabilitation, and prevention. Current Sports Medicine Reports. 18 (6). 217-223. https://journals.lww.com/acsm-csmr/Abstract/2019/06000/Ankle_Sprains__Evaluation,_Rehabilitation,_and.7.aspx Uploaded : 22 October 2019 Read More -

The use of ultrasound for mastitis
The use of Ultrasound for the treatment of Mastitis Mastitis is a painful blockage of the milk duct of the breast. Symptoms include swelling, redness, tenderness, localised increased temperature, generalised malaise and occasionally fever. It is a painful condition occuring most commonly 2-4 weeks post partum in the breast feeding mother. Generally, the pain is derived from both the physical blockage as well as the resultant inflammation. Severe and prolonged mastitis can cause infection and sometimes abscess formation. The latter would need treatment with antibiotics, whereas the former can be treated with physiotherapy. Physiotherapy treatment may include gentle massage, self instruction on massage, reassurance to continue breast feeding, even the use of lactation aids such as expression pumps and ultrasound. During pregnancy you will have become familiar with ultrasound imaging. Another form of ultrasound is used extensively in physiotherapy for treatment of soft tissues injuries. Ultrasound is a sound wave, which delivers a mechanical massage at the natural resonance frequency of our bodies, 50hz. By using this frequency, in effect the ultrasound is massaging at a cellular level. This vibration most likely improves lymphatic drainage, cell membrane permeability, and increases arterial inflow and venous outflow. It probably also calms nerve endings. Physiotherapists have been using this form of treatment for over 40 years. Sharna Hinchliff, herself a mother of 4, including twins, knows a lot about issues associated with pregnancy and the post partum period. Don't hesitate to contact us for more information. Uploaded : 17 October 2019 Read More -

Preventing Falls in the Elderly
Preventing falls in the elderly Hello everyone and welcome to our October blog. This month we’re going to talk about the older generation of people we are fortunate enough to share this world with. It only seemed fitting given that on the 1st of this month it’s International Day of Older Persons. It’s no secret that the elderly population is growing. People are living longer, and in many cases, having to work longer too. Being a physio is not just about treating sports injuries. We treat people from all walks of life and we certainly see our fair share of elderly patients. Most people know that as we age our bodies go through a process of gradual degeneration. Our joints are susceptible to wear and tear, our muscles weaken and other areas of the body like eye-sight also become affected. Our ability to move efficiently declines and this can lead to an in-creased risk of falls and subsequent injury. Falls are actually one of the leading causes for injury in the elderly population and it’s not unusual for us physios to be called upon to help in the after-math of a fall. Common injuries include hip and wrist fractures, as well as shoulder and head trauma. It’s our job to get these people moving again and on a speedy road to recovery. Prevention is better than cure We are always there for anyone who has been unfortunate enough to experience a fall and have a resultant injury. Whether it’s getting them moving again following hip surgery or a wrist fracture, we have the tools and knowledge to get them back to their best. However, everyone knows that prevention is better than cure. And there are lots of things that can be done to prevent falls in the elderly. Let us outline some things we can do to help: • Biomechanical assessment - we know human biomechanics. We can look at how you move and highlight any dysfunctions within your body that may be a risk factor for falling. We can then provide you with hands-on treatment, a home exercise program and sound advice on how you can nip those issues in the bud to reduce your risk of falling.• Strength and conditioning exercises - a common cause of falling is weakness, particularly in the lower limbs. We can test your strength and provide you with a gentle strengthening program to ensure you are working towards a stronger body that can support you better as you age.• Balance and coordination exercises - our balance and coordination can also be affected as we get older. And you can imagine, if your balance is poor, then the likelihood of falling can in-crease. Well fear not, we can provide you with exercises that aim to improve your balance and coordination. You’ll be feeling steady on your feet in no time!• Advice for the home setting - it’s not just issues with the body that increase the risk of falls. It’s also important your home is set up in a way to reduce your risk of falling. For some elderly people, ensuring that carpets, rugs and mats are removed from common walkways, and ensur-ing there is plenty of room to maneuver around furniture can greatly reduce the risk of falling in the home.• Help with walking aids - some elderly people require the use of walking sticks or frames. We’re here to help you get the best out of your walking aids. We can teach you how to use them so that they are a benefit to you rather than a hindrance. During a consultation, we may highlight other areas that need attention outside of our domain. You may need a medication review from your GP to ensure your medications are not a risk factor. If you have poor eyesight, you may require the help from an optician or optometrist. And if your feet require some further expert eyes, we will be able to point you in the direction of a good podia-trist. We’ll ensure you know exactly which areas require attention so that the risks of falling are as low as possible. We understand that getting older is often a challenge and that it can be very difficult to come to terms with a body that is not working as well as it once was. We are here to tell you that help is at hand and we promise it’s not all doom and gloom. You have the power people! If you eat well, drink heaps of water, exercise regularly and work at keeping your body the temple it deserves to be throughout your life, your body will thank you for it later! References: 1. United Nations. 2019. International day of older persons. [Online]. Available from: https://www.un.org/en/events/olderpersonsday/. [Accessed 06 Sept 2019].2. Waldren, N. et al. 2012. Falls prevention in older adults: Assessment and management. Aus-tralian Family Physician. 41 (12). 930-935. https://www.racgp.org.au/afp/2012/december/falls-prevention/3. Richardson, M. et al. 2019. A study to evaluate the potential contribution of medication use to falls in elderly patients presenting to an acute hospital. In Hospital Pharmacists Association of Ireland Annual Conference 2019. Uploaded : 26 September 2019 Read More -

Osgood Schlatters Disease
Injury blog: Osgood-Schlatter disease With most of the winter sports coming to a close, we may start to see a few less sports injuries coming through the door. But far out, we have been busy treating all kinds of injuries this season! There are thousands of really active kids in Australia and across the world - and active kids are bound to pick up a few injuries here and there. Being young comes with its advantages, but it al-so comes with its hurdles. Growing being one of them. Active adolescents are particularly susceptible to developing a knee condition called Osgood-Schlatter disease. This problem usually arises around the time when a child goes through a big growth spurt when rapid changes are occurring in the bones and muscles. Does your child play lots of sport and sometimes has pain around the front of their knee? Are they currently in the mid-dle of a growth spurt? Then read on… What is Osgood-Schlatter disease? Osgood-Schlatter disease is a condition which is characterised by inflammation and pain on and around a bony prominence on the lower part of the knee joint. As your quad muscles run down your thigh to your knee, they merge to form the patella tendon which then inserts into the shin bone or tibia. Where the patella tendon inserts into the tibia is called the tibial tuberosity (you should be able to feel the small bump at the top of your shin bone). Inside this part of the bone is a growth plate, a highly active part of the bone where put simply, growth of the bone takes place. Now, because kids these days play a hundred different sports and activities, the quad muscles repeatedly contract, especially during running and jumping (footy and netball are classics for this type of injury). This can lead to the pulling, softening and irritation of the growth plate underneath where the patella tendon inserts. This leads to inflammation and ultimately, pain which is aggra-vated by exercise. Who does it affect? Boys are generally more affected than girls, and usually at slightly different ages due to the differ-ences in age when the growth spurt occurs in each gender. Once activity at the growth plate slows and eventually closes, the pain relating to this condition generally goes away. This is usual-ly around the age of 16 in boys and 14 in girls. Depending on how severe the problem is, the end result may be having to live with a slightly enlarged tibial tuberosity. Can treatment help? The simple answer is yes! And treatment is pretty simple too. After consulting your physio for diagnosis and advice, the most important aspect of treatment for this condition is activity modifi-cation. If the child can modify the amount of activity they are doing, it can greatly reduce the amount of pull on the bone and therefore less irritation to the growth plate. Because it is a devel-opmental condition, children and parents should be informed from the beginning that symptoms may come and go, but may last right up until the child reaches the age where the growth plate closes. So, play when you feel good, and rest when you are in pain. Your physio will likely re-lease excess tension in the quads and provide you with some light stretching to perform at home. Some people also respond well to strengthening and this is usually implemented when pain al-lows. Icing when pain is high may help to reduce pain and control inflammation and swelling. There are also some handy patella tendon de-loading taping techniques which your physio may well make use of to control pain and keep your child playing longer. We hope you found this an interesting and educational read. If you are young and reading this, or if you have a child with knee pain that is aggravated by exercise, please call and book an appointment so we can have a look and get you managing this problem from the get-go! Osgood Schlatter may feel like NotSoGood Schlatter disease (now that’s a dad joke!), but with our help, your child will be feeling good in no time! References 1. Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. Australia: McGraw-Hill Education2. American Academy of Orthopedic Surgeons. 2019. Osgood-Schlatter disease (Knee pain). [Online]. Available from: https://orthoinfo.aaos.org/en/diseases--conditions/osgood-schlatter-disease-knee-pain/. [Accessed 05 Sept 2019]. Uploaded : 25 September 2019 Read More -

Physiotherapy
Physiotherapy… What is it exactly? Hello everyone and welcome to our September blog (it’s 4 months until Christmas - the countdown is on!). This month we are going to answer a question that we get asked A LOT by our patients. And because we get asked it so much, we thought we would dedicate a whole blog to it. The question we refer to is ‘What is Physiotherapy?’. To answer this question, we’ll give you some insight into what Physio is, how it can help you, and the sorts of things you can expect to experience during a typical consultation with a Physiotherapist. So… What is Physiotherapy? If you are looking for a simple definition of what Physiotherapy is, we think the Royal Children’s Hospital Melbourne sums the profession up very nicely. They say, “Physiotherapy is a clinical health science and profession that aims to rehabilitate and improve a person’s ability to move and function”. The lead governing body of Physiotherapy in Australia, the Australian Physiotherapy Association (APA) say that “Physiotherapists help you get the most out of life. They help you recover from injury, reduce pain and stiffness, increase mobility and prevent further injury. They listen to your needs to tailor a treatment specific to your condition”. We couldn’t have said it better ourselves! Basically, if you have hurt yourself or have a long-standing mobility issue, there is a good chance seeing a Physiotherapist is going to be beneficial to you. We use our expertise in the anatomy, physiology and biomechanics (i.e. how the body moves) of the human body to assess and provide treatment to people of all types with a wide range of health problems. And to ensure you are in the safest hands possible, each Physiotherapist has to obtain a university degree and be registered by law with the Australian Health Practitioner Registration Agency (AHPRA). So, you won’t be walking in and placing your health in the hands of any random off the street. Your Physio has been put through their paces to ensure they provide you with the best possible care. What to expect during your appointment For those who have never seen a Physio, we understand it can be quite daunting booking your first appointment. Fear of the unknown… What are they going to ask me? Will I have to get undressed? It’s perfectly natural to feel these things when you are trying something new. But ask someone who regularly uses the services of a Physio and they will be able to put your mind at rest. Physio’s are friendly and knowledgeable people. Yes, they ask you questions, and yes you might have to show your arms, legs and other body areas during the consultation, but everything is done with the patient’s well-being in mind. We know getting undressed can be embarrassing for some people, so we always advise you to wear comfortable loose clothes like shorts and a sports top, and if we require to see an area of the body like your abdomen or back, rest assured we’ll only look where we need to, and you should always, always, always keep your underwear on, and of course decline if you’re uncomfortable. Most Physio clinics will provide you with a robe or gown to wear during an assessment or treatment to ensure you feel safe and protected at all times and cover you with towels where appropriate. We promise there is nothing to be afraid of. After you have arrived for your appointment and have been greeted by your Physio or receptionist, you will likely be asked to fill out some paperwork that takes care of your personal details and all the administration stuff. Then you’ll be directed into a room or space where your Physio will sit down with you and talk to you about why you are there, and most importantly, what you want to achieve with their help. Once they have all the information they need (expect questions relating to lifestyle, occupation, social life, sleep, exercise and hobbies… They are all important), they will then carry out an assessment on you. During the assessment they will watch you stand and get you to move. They may even move some body parts for you and carry out a range of tests so they can come to an accurate diagnosis. Once they have a diagnosis, there’ll be a brief discussion to let you know exactly what is happening, what treatment is required, and a general plan laid out, so you know exactly what is going to be involved. Before your Physio carries out any treatment on you, they will always get your consent and tell you why they are wanting to perform that treatment. Physio’s use a wide variety of techniques to treat their patients. These might include soft tissue massage, joint mobilisation and manipulation, dry needling and acupuncture, hydrotherapy (i.e. the use of water in rehab), exercise and treatments that may use treatment aids such as splints, casts, braces, tapes, crutches and wheelchairs. This obviously depends on the issue you are being treated for, as each person and their rehab is completely unique. Appointments will usually last anywhere from 30-60 minutes and by the end of your initial consultation, you will have a clear explanation of what is going on with your body and a plan of attack to get you out of pain in the quickest and safest way possible. If your Physio thinks you require a scan of a body part, or the opinion of another health professional such as a GP or specialist, they will also discuss this with you. So, there you have it. We think we’ve covered just about everything. If you are wanting to book a Physio appointment, or are looking to find out more information, please do not hesitate to contact us on 02 9922 6806. We are ready to help you! Uploaded : 22 August 2019 Read More -

Quadriceps
Body facts: The Quadriceps muscles Fancy a stroll? Or is it leg day at the gym (groan)? It doesn’t matter whether you are old or young, a cyclist, fishmonger or a green-fingered gardener. To perform the simplest of everyday tasks such as getting out of a chair, walking or climbing the stairs requires a complex array of movements using many muscles and joints. One particularly important group of muscles which helps us to perform such tasks is the quadriceps muscle group. Here’s a little run down of what they are and why they are important to you. Some anatomy and biomechanics for you… The quadriceps or just ‘quads’ are a group of muscles found on the front of the thigh. As the name suggests, there are four muscles all together. As with most things on the human body, they have some fairly crazy names… We’re pleased to introduce you to Rectus Femoris (RF), Vastus Medialis (VM), Vastus Intermedius (VI) and Vastus Lateralis (VL). Start memorising now… We’ll test you on them later! The VM, VI and VL muscles all span from the thigh bone (femur) to the leg bone (tibia) running down the front aspect of the body. The RF muscle sits on top of the three Vastus muscles and spans from the front of the pelvis to the leg bone where the other three muscles also attach. Because all four muscles cross the knee joint, they all help you to straighten your knee (known as knee extension). But because the RF muscle also crosses the hip joint, it has a separate function in helping you to bring your thigh forward in front of you (known as hip flexion). As the muscles run down the thigh and cross the knee joint, they converge into one big tendon which houses the kneecap or ‘patella’. And because the patella lives inside the quad tendon (it literally floats over the knee joint), the quads also have the very important function of controlling the movement and tracking of the patella over the knee joint. These powerful soldiers of the lower limb are partly responsible for ensuring that your kneecap doesn’t constantly dislocate (just imagine that!). So, they are a pretty useful group of muscles to have around. Some real life examples Let’s give you some examples in everyday life where you are using your quads. Climbing the stairs is a good example. As your leg goes forward towards the step, your RF muscle (along with some other muscles) flexes the hip. As you take your step up and your knee straightens to drive you up, all four muscles are acting together. Kicking a soccer ball is another good example. You run towards the ball, plant one foot next to the ball and the other leg swings through. RF drives the hip joint forward and all four muscles contract to straighten the knee so you can blast the ball into the top corner. This is quite a simplistic way of looking at things because as we’ve already suggested, there are other muscles helping all of this to happen, but you get the idea of how the muscles are working together to help us do these actions. As with all muscles, there is potential for injury, and quad muscle or tendon injury is quite common. Muscles can be strained with varying severity, repetitive movements commonly lead to tendon related injuries, and taking a knee into the thigh from an opposing player for example can leave you with a nasty corked muscle, not to mention a dead leg! And now… …A TEST! Haha, we said there would be one! Look at the table below. On the left we’ve listed the two main movements that the quads are responsible for in the human body. It’s your job to list which muscles are responsible for those movements. Write down or tell yourself RF, VM, VI or VL for each movement. Try it first and then check back through the text to see if you’ve remembered. Who said tests aren’t fun? Movement Muscles responsible (RF, VM, VI, VL)Hip flexion ???Knee extension ??? Uploaded : 22 August 2019 Read More -

Stress fracture in an adolescent foot.
Sports Physiotherapy Clinical Reasoning : Stress facture in an adolescent female track and field athlete A 16 year old female track and field athlete presented with a 6 month history of foot pain. However, it was never enough to stop her from competing and training. She did seek the intervention of a sports podiatrist. She was running 3-4 times per week, playing hockey and touch football. Her identical twin sister was doing a similar amount of exercise. Current History June 2018 - Combined Inter Schools X-Country race where she experienced no pain during the race which she won, but immediate intense pain once the race was over. Imaging An MRI was undertaken showing a stress fracture of the second metatarsal. A CT scan noted the callous formation either side without union Additional clinical findings were a Mortons toe and normal menarche and menstrual cycle. She was also excessively mobile and potentially has Ehlers Danlos Syndrome Mortons Toe is where the 2nd toe is longer than the first toe. Biomechanically this results in forefoot pronation and excessive loading of the 2nd ray. In Roman times this was considered a sign of beauty. Vikings generally had the opposite, a very large big toe and much smaller 2nd toe. Treatment Moon Boot for 4 months Daily bone stimulator -> Exogen Physio -> intrinsic muscles of the foot, calf and gluteal strengthening, Soft sand walking and running can become an ideal environment for this in the latter stages of rehab Eventually Alter G Treadmill program to recommence return to running Used Hoka A minimal shoes Land based return to running programme and agility exercises Fully returned to running 9 months later Uploaded : 8 August 2019 Read More -

Avulsion Fracture of the ASIS
Avulsion Fracture of the ASIS ASIS avulsion fracture in a 16 year old playing soccer. An uncommon injury, in adolescents, where the sartorius and/or Tensor Fascia Lata pulls suddenly on it's pelvic attachment, near the growth plate. Depending on the extent of displacement, either surgical or conservative management can be undertaken. Conservative treatment consisted of bed rest, with the affected hip at 70–90° flexion for the first three weeks, with symptomatic treatment of pain and soft-tissue oedema. After three weeks, physiotherapy and ambulation with crutches can begin, determined by X-ray findings. Partial weight bearing using crutches is indicated until six weeks from injury, when an X-ray check should be performed, and gradual full weight bearing with restricted running, jumping and sports are allowed Sprinting and full participation in sports activity was allowed six months after the injury. Sartorius Muscle Tensor Fascia Lata Further, complications may include damage or irritation to the lateral femoral cutaneous nerve resulting in meralgia paraesthetica. These cases should be considered for surgical intervention as a neurological deficit could occur. Additionally, fragment displacement of >3cm should also undergo surgical intervention. Time course of healing is quicker in the surgical group, with return to sport after 3 months vs 6 months in the conservative group. Ultimate outcomes appear to be the same regardless of intervation type. References : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4071503/ Uploaded : 1 August 2019 Read More -

Repetitive linear head trauma
Repetitive linear head trauma can cause cummulative subclinical effects on visual and vestibular (balance) function Linear repetitive impact without concussion symptoms have been shown to have some impact on visual memory and vestibular (balance) function. Interestingly, although these researchers didn't find clinical neurolgical deficits, others, using MRI imaging, have reported anomalies. Speculation remains, that cortical cognitive reserve means that these deficits are not immediately apparent, Judicious use of ball heading is recommended and potentially should be completely avoided in the young. (Caccesse et al 2019. MedScSpEx, 51, 7, 1355-1361). https://www.back-in-business-physiotherapy.com/we-treat/concussion.html Read More -

Calf Pain
Calf pain? All you need to know about Achilles Tendinosis It’s Sunday, which can only mean one thing… You’re meeting with your soccer team to play a friendly competitive game against your local rivals. After years out from playing, this season, you’ve decided to dust off the boots and start playing again. Life has been generous over the years, a doting partner, two healthy children, and maybe a generous waistline has come with it all too. It happens sometimes, but you were determined to get active again and do what you’ve always loved doing - running rings around the opposition’s defence and scoring goals! But now, you’re halfway through the season and your old calf injury has decided to rear its ugly head. It’s been years since you’ve felt the pain, but it’s very familiar, and it can really ache! So why did it rear its ugly head now? This scenario is a very common one us physios come across. We think it’s great that people decide to get themselves active again, and we’re here to help them achieve their goals. Unfortunately, that sometimes means getting them through an injury, often a recurrence of an old sports injury. The condition we described above affecting the calf is Achilles Tendinopathy, or more specifically ‘Tendinosis’. The Achilles tendon is a large broad tendon that sits at the back of the ankle. It is an extension of the calf muscles - the gastrocnemius and the soleus (bit of a mouthful hey!). It runs down the back of the leg and inserts into the heel bone (or calcaneus). The tendon is also often referred to as the calcaneal tendon. It is a very powerful tendon and functions as a spring to propel us forward and ‘push off’ when walking or running. Tendinosis refers to the degeneration and derangement of the tendon fibres that make it up. Usually the fibres run in parallel lines straight up the back of the leg, but with tendinosis, these fibres can become a bit of a higgledy-piggledy mess due to repetitive stress and consequent small tearing, followed by poor healing through the area. This means the tendon cannot function efficiently for you and eventually you can end up with a painful calf. This is very commonly seen in middle-aged, overweight people and most commonly affects the mid-portion of the tendon as it passes up the calf, much like our soccer star mentioned above. What to expect with Achilles Tendinosis The major symptom is pain, most often felt with movement after a long period of rest. As you continue to move, you may notice the pain goes away, only for it to return once you have finished your activity. There may or may not be swelling around the tendon insertion too. You may notice pain with activities such as walking up the stairs and hopping… Basically anything that loads the tendon and requires you to push off in order to move you in the direction you want to go. What can be done to help? Lucky for you, you’ve just walked into your physio clinic to seek help, which is exactly the place you need to be. We, at Back in Business Physiotherapy, see this all the time and can really help you with it. We’ll get you in for some questioning (the friendly kind, we swear) and then have a look at you moving around. We’ll pick up on all the things that have led you to this point. This might relate to old injuries you’ve had — maybe you never managed to rehabilitate properly years ago, and it is still affecting you now — and/or problems with the way you move currently and the strength you have in your muscles. You might have poor ankle mobility, or flat feet, or weak hamstrings… All things that can eventually lead you to have an Achilles tendon issue. Our aim is to rid you of pain and to correct all the issues mentioned above, so we can keep you out of pain and on the field (or wherever you want to be) for longer. One aspect of your rehab will be getting you stronger. There is scientific evidence behind the use of strength training when rehabbing Achilles tendinosis. One example of an exercise your physio will likely get you performing is a heel raise with a slow controlled drop off the edge of a step. Without getting too deep into the science behind this, this exercise allows the tendon to be loaded whilst the muscle is being lengthened (rather than shortened), and aids with the re-arrangement of the fibres running up the tendon. Over time, the tendon will begin to restore to its former glory and will be stronger and able to spring you forward like Tigger on his tail… Okay so maybe not that much, but you’ll feel the difference and will be moving with confidence. Of course, the rehab will involve a lot more than just this exercise - you may need to do some foot, hamstring, glute or core strengthening, ankle mobility exercises, and some people may need to be fitted with orthotics to help them along the way too. But don’t worry, your physio will be able to guide you through it step by step. So, don’t wait around for your calf pain to go away on its own, give Sharna or myself a call and we’ll get you on the road to a speedy recovery! Cheers Martin Krause, 23 July 2019 References Li, H. and Hua, Y. 2016. Achilles Tendinopathy: Current Concepts about the Basic Science and Clinical Treatments. BioMed Research International. 2016. 1-9. https://www.hindawi.com/journals/bmri/2016/6492597/abs/ Sports Medicine Australia. 2019. Achilles Tendon Injuries. [Online]. Available from: https://sma.org.au/resources-advice/injury-fact-sheets/achilles-tendon-injuries/. [Accessed 03 Jul 2019] Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. Australia: McGraw-Hill Education Aicale R., Tarantino D., Maffulli N. (2019) Non-insertional Achilles Tendinopathy: State of the Art. In: Canata G., d'Hooghe P., Hunt K., Kerkhoffs G., Longo U. (eds) Sports Injuries of the Foot and Ankle. Springer, Berlin, Heidelberg Karlsson J., Brorsson A., Jónsdóttir U., Silbernagel K.G. (2019) Treatment of Achilles Tendinopathies. In: Rocha Piedade S., Imhoff A., Clatworthy M., Cohen M., Espregueira-Mendes J. (eds) The Sports Medicine Physician. Springer, Cham Read More -

Book Week
Attention all bookworms! Let’s pack for your back! On your marks… Get set… GO! Let’sseehowmanybookswecanreadasquicklyaspossiblewithoutstoppingforbreathinbetween! And breathe… Yes, it’s that time of the year again for us book lovers. Book Week 2019 is being celebrated this August (17th-23rd) and it’s time to get prepared. For some of us, this might mean we’ll be reaching for an epic page turner for the first time in ages, or it might just be a great excuse to read an extra one (or two or three) books that week. For your children attending school, there will likely be several activities they will be taking part in to recognise the event, which means they’ll have one or two more books they need to carry in their school bags. As if they didn’t have enough already right?! You might be starting to think, why is my physio posting a blog on book week? Well, let us explain. Let’s face it, who doesn’t like grabbing a book, a mug of tea, a few biscuits, your favourite blanket, and snuggling down into your favourite armchair for endless hours of reading? OK, so it might not be for EVERYONE, but we love it, and for those that do too, it may mean being stuck in the same position for hours on end whilst your head is in your book and you become too engrossed in the story to realise you are straining your neck. And what about your kids? Their school bags are already heavy from packed lunches, sports kits and textbooks, and now they must take in their favourite books to read in class too. Just think what all that weight is doing to their developing little frames as they drag their backpacks around the school yard. We’re here to give you some sound advice on how you and your family can stay safe and healthy this book week. Although the advice stretches to the other 51 weeks of the year too. Sitting bookworms We’re all for snuggling up in your favourite chair or lounge to read a book. We just want to make sure that you aren’t putting yourself at risk of injury from being in the same cramped position for hours on end — and that’s not taking into consideration the possibility of falling asleep in the same spot either. If this happens, you might need to reconsider your book choice! To ensure you aren’t straining your neck and back whilst reading, try the following: Sit comfortably, but try to sit straight (this is achievable, honest) to keep your spine aligned If you do adopt a different position (i.e. lying down or curled up in a foetal position) make sure you move regularly to give your body a break from being in one position for too long Take regular breaks from reading to give your hands, shoulders and neck a rest At the end of a chapter, get up and do some stretches, squats, lunges or whatever else you enjoy doing (this includes grabbing a well-deserved cup of tea) Remember to attend to necessary life requirements like talking to family members, cooking dinner, and sleeping (hopefully not because your book is boring though) – yes, this one is tongue in cheek (although a reality in many cases)! Backpack advice When sending your kids off to school with backpacks in tow, there are some important things to remember to keep the pressure off their backs and shoulders (remember this also applies to adults too — they are not immune to the effects of heavy baggage either). Try these: Always wear BOTH straps - a single strap might look cool and be convenient to sling over the shoulder, but it will increase strain down one side of the body leading you to a possible postural imbalance Tighten the straps so that the backpack sits above the waistline (avoid letting it hang below the waist) Tighten the straps enough to limit side-to-side swinging of the bag on your back when walking - if you have a chest strap, this will also help to reduce swinging and keep the straps in place If you have a waist strap, this can help to spread the weight of the backpack over the pelvis and hips, whilst reducing load through the shoulders. You rarely see a hiker not wearing their waist strap, so why shouldn’t you? After all, carrying around a heavy backpack for most of a school or working day, repeated five days a week, can take its toll. Follow the recommended backpack weight guidelines of no more than 5-10% of a person’s bodyweight (an average 11-year-old weighs around 36 kg, so ensure their backpack weighs no more than 3.6 kgs) If you follow the above advice, then you are taking positive steps towards keeping you and your family safe and reducing the risk of injury. If you would like further advice or have woken up with a stiff neck after a hefty night of reading, please call us to book an appointment. We will ensure you are the turning pages pain and risk free before you can finish the synopsis (you know, the bit on the back of a book that we sometimes forget). Oh… And keep your waistline healthy by only having one or two biscuits please. We know how moreish they can be! #longlivebooks References The Children’s Book Council of Australia. 2019. CBCA Book Week [Online]. Available from: https://cbca.org.au/news/cbca-book-week-2019. [Accessed 10 July 2019]. National Safety Council. 2019. Back Pack Safety: It’s Time to Lighten The Load on Our Kids. [Online]. Available from: https://www.nsc.org/home-safety/safety-topics/child-safety/backpacks. [Accessed 10 July 2019] Uploaded : 23 July 2019 Read More -

Anterior Cruciate Ligament
Sprained your ACL? Let us guide you through Hello everyone and welcome to our July blog. We’re halfway through the year already, which means the soccer season, rugby and netball are in full swing! Added to this the start of the ski season. Why is this relevant you ask? Well these are sports that send quite a lot of people our way. It’s this time of year where we start to see an influx of knee injuries and it’s an especially busy time of year for treating ACL sprains - the injury any keen sports person will want to avoid at all costs! Unfortunately, there has been a significant increase in ACL injuries over the last twenty years, with nearly 200,000 people requiring surgical repair between 2000-2015 in Australia alone. A bit of anatomy for you The ACL, or Anterior Cruciate Ligament is one of four main ligaments that support and stabilise the knee joint (the others being the posterior cruciate, medial collateral, and lateral collateral lig-aments). Deep inside the knee it connects the thigh bone (femur) to the shin bone (tibia) and its main purpose is to stop the shin bone from moving forward and over-rotating when we perform certain movements. It is particularly important at stabilising the knee during movements such as jumping and landing, pivoting with a quick change in direction, and deceleration (slowing down) movements. It’s no surprise then that the way people tend to injure this ligament is by performing exactly those types of movements. Injury occurs when the ligament gets taken beyond its capa-bilities of supporting and stabilising the knee, and the result is a sprain of the ligament. Imagine a netball player jumping to catch the ball, and then landing and pivoting on one foot to change di-rection quickly. As they turn, their knee twists and falls inwards while the foot is still planted on the ground… And that’s all it takes. Minor sprains involve only part of the ligament, but less fortu-nate occurrences may tear the ligament completely - known as a ‘rupture’. What to expect when it happens If you are unfortunate enough to experience such an injury here is a list of signs and symptoms to look out for: • An audible pop or crack in the knee• Intense pain (especially in the immediate aftermath of a full rupture)• Inability to continue activity• A possible large swelling of the knee (this may be delayed in certain instances)• A feeling of instability if attempting to perform further movement• Restricted knee movements with inability to straighten the knee in particular• Widespread tenderness (especially on the inside and outside of the knee) Single joint and whole body movement changes in ACL injured athletes returning to sport (Smeets et al 2020, Med Sc Sp Ex, 52, 8, 1658-1667). The most prominent change is the increased activation of the hamstrings muscles. In surgical cases, this may be due to the use of the hamstrings (semitendinosis) tendon as a donor for the graft. Additionally, this can be a compensatory action to minimise the anterior shear of the tibia under the femur. As such, whole body compensation would be a more erect landing pattern on hopping and jumping. These authors did not find such a pattern, apart from decreased ankle flexion on the side ways hop. Another factor, may simply be that hamstring activation is a means whereby we limp, or it may represent conscious activation from physiotherapeutic reinforcement during exercise rehabilitation. Reduced knee flexion moments have also been found, which presumably represents a compensatory action to reduce anterior shear. Additionally, increased hip and trunk flexion moments were observed which moves the centre of mass more anteriorly, thereby increasing the loading of the posterior chain whilst sharing the muscular synergistic loading across the upper 2/3 of the thigh (hamstrings and quadriceps) as well gluteal contractions, which invariably lead to pelvic floor and abdominal contractions. These authors found increased trunk and hip flexion angles in 3 of 5 tasks but only in the long hop did they find an anterior centre of mass. As such, they concluded that clinicians use task independent single joint motions in their assessment of return to normal function. Programs such as FIFA 11 for ACL rupture prevention can also be used as part of the rehabilitation process. Additionally, a Delphi consensus reaching process for return to sport should also be consulted. - Return to Sport : Delphi consensus RTS ACL - FIFA 11 Plus :https://www.fifamedicalnetwork.com/lessons/prevention-fifa-11 It’s important to know that ACL injuries will often come with extra baggage. As if tearing a ligament inside the knee isn’t bad enough, unlucky recipients will also often damage the medial col-lateral ligament, the meniscus (a cartilage type structure inside the knee), or the cartilage that covers the end surfaces of the bones. Some refer to an injury which includes the ACL, MCL and meniscus as the ‘unhappy triad’. And you’d be quite unhappy indeed! However, there is light at the end of the tunnel! With the right guidance and professional care, your recovery journey can be a successful one! So what next? The first thing you need to do is see a professional. Contact our friendly team at Back in Business Physiotherapy today who can help to diagnose you. The sooner after initial injury the better, be-cause once the swelling kicks in, it’s a bit more difficult to diagnose accurately (at least until the swelling has reduced). Your physio may refer you on for imaging; often an MRI will be performed alongside an x-ray. Once you have a solid diagnosis, the next important choice is whether to treat surgically or conservatively. Generally, if it is a partial tear, a conservative approach would be taken, but this totally depends on the person and what their goal is in life. It’s quite possible to live life with no ACL at all, but you will have to be prepared to adjust what types of physical activities you partake in. A professional football player who is still young and has a career ahead of them may opt for a surgical repair with a subsequent intensive rehabilitation process to stand the best possible chance of performing at a professional level again. It’s a complex decision with many factors to consider, such as age, level of injury and the persons occupation. Your physio will be able to guide you to the right choice for you. If you opt for surgical repair, then the rehabilitation process generally takes around one year. For a partial tear without surgery, the process would be faster. Ultimately your physio will follow a structured protocol to get you back to fitness again. Phases of rehab will include the following: • Reduce swelling and restore full range of motion• Begin to progressively strengthen the lower limb muscles (i.e. quads, hamstrings)• Move from non to partial to full weight bearing (depending on the injury)• Improve balance and control of movement• Begin gross body movements such as squatting and lunging• Return to jogging, running and pivoting• Return to sport (training and fun match play) Increased hamstring activity can lead to increased compressive forces in the knee resulting in the early onset of Osteoarthritis. Similarly, excessive shear can result in OA. Therefore, rehabilitation needs to bear this in mind and find an optimal hamstring loading pattern. Further variations on the reverse lunge can include diagonal reversal, sideways slides and the use of a step. 60-70% of shock absorption in the knee can come form the calf, so eccentric calf strength is important. As mentioned previously, trunk and hip strength are also important factors in knee control. As stated before, the recovery process really depends on each person’s individual situation. For you it might be completely different than your neighbour or family member. Keep in mind, that it is possible to re-injure your ACL following surgery, with most cases of re-injury occurring within one year. For many, the risk of injuring the other knee is a distinct possibility, so it is pivot-al (no pun intended) that you follow our advice here at Back in Business Physiotherapy to ensure you achieve your goal and stay clear of injury in the future. Anyone for shooting some hoops? Safely, of course! ACL rupture and the menstrual cycle https://www.back-in-business-physiotherapy.com/latest-news/255-female-hormones-and-knee-strength.html References: 1. Zbrojkiewicz, D. et al. 2018. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. The Medical Journal of Australia. 208 (8). 354-358. https://doi.org/10.5694/mja17.009742. Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. Australia: McGraw-Hill Education Uploaded 10 July 2021 Read More -

Gluteal Strength
WEAK GLUTES? GET YOUR BUNS OF STEEL HERE! Nip into your nearest gym and you’ll hopefully see a bustling atmosphere of people working out, trying to reach goals and get their bodies stronger. You’ll see all kinds of movements occurring, push, pull, jump, squat, lunge, lift… The list is endless. Maybe your physio has advised you to get to the gym yourself and work on some strength training. —You’ve been getting a bit of lower back pain and they’ve highlighted that your glutes are weak and may be contributors to your pain. It’s hard to fit everything in! You have to sit all day at work, and you just don’t seem to find enough hours in the day after work, kids, cooking, washing and shopping to set aside time to concentrate on you and getting yourself stronger. So the bad news is, sitting for long periods of the day could be contributing to your back pain. When you sit for long periods, your hip flexors become shortened and tight. This prevents your hips from being able to extend properly (we need this to help propel us forward when we walk, run, jump and climb the stairs) and which muscle is responsible for hip extension? That’s right, your gluteus maximus muscle! Not being able to extend the hip well, means the gluteus maximus muscle becomes a bit lazy. It’s not being used properly, it’s not able to contract all of those muscle fibres through their full range to provide you with a powerful contraction. Therefore, weakness sets in and other areas of the body have to work harder to compensate for this. The lower back is one of the areas that works harder when your glutes slack off— and it lets you know it is working too hard by sending a signal to the brain that all is not well. You feel this as pain. Now it’s not all doom and gloom, don’t worry. There is good news! Your trusty physio here at Back in Business Physiotherapy will be able to use their magic to get your hip flexors released and the hip moving successfully into extension. But you’ll have to back up the work done on the treatment table by performing exercises at home. These exercises might include some hip flexor stretching, hip mobility, and gluteal activation, as well as strengthening exercises. To make it simpler for you, we’ve described three beneficial glute exercises that you can perform at home to ensure your glutes will be firing on all cylinders. Check them out below… 1. Hip thruster - Sit with your upper back against the edge of a bench (the seat of your couch will work just fine!)- Reach your arms out to the side along the bench for balance- Have your knees bent and feet flat to the floor approximately hip width apart- Squeeze your buttocks as you raise your hips up until your body and thighs form a horizontal line- Be careful not to over-arch your lower back- Return to the start position and repeat 2. Split squat - Stand tall and place your back foot behind you on a step or bench- Your front leg should be slightly out in front of you- Slowly bend your front knee, dropping your back knee down towards the floor- Squat with your front leg to an angle of approximately 45-90 degrees- Pause and then push up through your heel whilst you squeeze your buttocks- Return to the start position and repeat 3. Deadlift (using a resistance band) - Stand with your feet hip width apart on top of a resistance band- Squat down with a straight back and hold the ends of the band with each hand- Draw your shoulders back, chest up, and push up through your legs to a standing position against the resistance of the band- Return to the start position and repeat- A progression of this one may be to use a bar bell instead of a resistance band Suggestion: Try 3 sets of 10-15 repetitions, 3-4 times per week for each of the three exercises above. 4. Buttock Ups - Simply, in standing or sitting, tighten and hence lift your buttocks. Hold for up to 90 seconds and repeat every hour. As the buttocks contract you should feel the deep abdominal and pelvic floor muscles contracting. Test your upper arm strength. With the arm stretched at 90 degrees ask someone to push your hand down towards the floor. Your upper limb strength should be better with the gluteals contracted. Good gluteals should improve lower limb stability. Resistance exercise training has been demonstrated to improve insulin resistant diabetes and reduce the severity of sarcopenia (https://www.back-in-business-physiotherapy.com/latest-news/239-mitochondrial-health-and-sarcopenia.html) Please remember to speak to your physio before attempting any new exercises and always give yourself rest days to allow for recovery and strengthening to take place. We have the expertise to guide you on which exercise is ideal for each stage of your rehabilitation. Be persistent, work hard, and you’ll be on a path to having fully functioning glutes and awesome buns of steel in no time! References 1. Brukner, P. et al. 2017. Clinical Sports Medicine. 5th ed. Australia: McGraw-Hill Education2. Jeong, U. et al. 2015. The effects of gluteus muscle strengthening exercise and lumbar stabilization exercise on lumbar muscle strength and balance in chronic low back pain patients. Journal of Physical Therapy Science. 27 (12). 3813-3816. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713798/3. All exercise descriptions taken from The Rehab Lab website Uploaded : 29 June 2019 Read More -

Digestion
Five tips for digestive bliss It’s bowel cancer awareness month, so we’re here to give you tips on how to keep your digestive system healthy, so you can be the best human you can be and reduce the risk of disease. Whether you are a professional soccer player, a tradie or an office worker, a healthy digestive system is key to you being able to function and carry out your daily tasks. Our bodies break down the food we eat into energy and this is what allows us to kick a ball, drill a hole, or sit and type on the computer. Now, your digestive system will only work properly if you feed it the right stuff… So don’t expect to last the 90 minutes and be at the top of your game if all you do is gorge on deep fried or fast food. That’s just a fast track to the subs bench and unhappy insides! Try out these little gems of advice to ensure your digestive system stays healthy, so you can give 100% every single day: 1. DRINK LOTS OF WATER: We’ll make this one nice and simple… Your body needs water for almost everything! From maintaining the health of every cell in your body, to keeping your blood fluid - you can see it’s pivotal for life to exist. Water is also needed for creating your digestive juices used to break down food and preventing digestive complaints like constipation. 2. EAT A HIGH FIBRE DIET: Fibre is basically all the parts of plant-based foods that we are unable to breakdown and digest. There are different types. ‘Soluble’ fibre (found in fruits, vegetables & legumes) helps to keep you feeling fuller for longer and helps to control blood sugar levels and lower cholesterol. ‘Insoluble’ fibre (found in the skin of fruits and vegetables, wholegrain breads/cereals, and nuts and seeds) absorbs water helping to bulk out and soften our stools and aids in regulation of bowel movements. Having a good mix is important to prevent diseases such as constipation, bowel cancer, diabetes, and heart disease. 3. EAT A PROBIOTIC: Probiotics are the bacteria found living in our gut. They are responsible for providing the ideal environment for getting the most nutrients out of the food we eat. They also protect us from the effects of nasty bacteria that may show their faces at different points. Without them, we wouldn’t exist. Sometimes our stores of bacteria can be put under threat, like when we are ill, stressed for long periods, or after a course of antibiotics. Having a poor diet can also be bad for them. Luckily, we can eat foods like probiotic or ‘live’ yoghurt and kefir daily to help keep our gut well-populated with these little soldiers. 4. GET PLENTY OF EXERCISE: The benefits of exercise are endless! When you move, it helps to promote movement of food through your gut, which keeps everything functioning well and helps to reduce the risk of digestive problems like constipation. So, move every day because your gut doesn’t tend to go on holiday for days here and there. It is always working hard for you! 5. LIMIT INTAKE OF ALCOHOL AND SMOKING: Too much of anything is a bad thing, but the effects of too much booze and cigarettes on the digestive system are well documented. Heavy, long term intake may lead to conditions such as reflux, digestive ulcers, and possibly more severe disease such as oesophageal, stomach and bowel cancer. Remember, you really are what you eat. Gut health is so important for you to do the things you want to do – work, playing with the kids, sports, everything! So don’t be surprised if your physio throws in some questions regarding digestive health when they’re treating you. It’s much more than just muscles and bones. We will delve deep if we need to, to make sure you are at the top of your game. If you are over 50, the Australian Government subsidises bowel screening testing. The kits are readily available from your doctor or pharmacy. If you are over 40 and have a family history of bowel cancer you should take the screening exam annually. References 1. State Government of Victoria. 2014. Water - a vital nutrient. [Online]. [Accessed 03 May 2019]. Available from: https://www.betterhealth.vic.gov.au/health/healthyliving/water-a-vital-nutrient2. Nutrition Australia. 2014. Fibre. [Online]. [Accessed 03 May 2019]. Available from: http://www.nutritionaustralia.org/national/resource/fibre3. Webster-Gandy, J., Madden, A., Holdsworth, M. eds. 2012. Oxford Handbook of Nutrition and Dietetics. Oxford: Oxford University Press4. Enders, G. 2015. Gut - the inside story of our body’s most under-rated organ. Melbourne: Scribe Publications5. Drinkaware. 2019. Is alcohol harming your stomach. [Online]. [Accessed 04 May 2019]. Available from: https://www.drinkaware.co.uk/alcohol-facts/health-effects-of-alcohol/effects-on-the-body/is-alcohol-harming-your-stomach/6. State Government of Victoria. 2019. Smoking - effects on your body. [Online]. [Accessed 04 May 2019]. Available from: https://www.betterhealth.vic.gov.au/health/healthyliving/smoking-effects-on-your-body 4 June 2019 Read More -

What is incontinence?
What is incontinence? Incontinence is the term used to describe the uncontrollable loss of urine from the bladder or faeces from the bowel. It ranges in severity from losing only a very small amount of urine, to a complete void of the bladder or bowel. If you’ve never experienced this, you can only imagine how distressing this must be. There are different types of urinary incontinence, including: • STRESS INCONTINENCE, where small amounts of urine leak due to small increases in pressure on the bladder during physical activity, or from coughing, sneezing or laughing.• URGE INCONTINENCE, where you get an unexpected, strong urge to urinate with little to no warning. This is usually as a result of an overactive bladder muscle.• INCONTINENCE ASSOCIATED WITH CHRONIC RETENTION, where your bladder cannot empty fully, and you get regular leakage of small amounts of urine. There are many causes for this, including an enlarged prostate in men, or prolapsed pelvic organs in women, as well as medications and certain conditions, such as diabetes and kidney disease.• FUNCTIONAL INCONTINENCE, where you are unable to get to the toilet, possibly due to immobility, or wearing clothes that are not easy to get off in time. Faecal incontinence is when you have a lack of control of bowel movements and you may accidentally pass a bowel movement, or even pass wind without meaning to. This may be due to weak muscles surrounding the back passage (Unfortunately ladies, this is common following pregnancy and childbirth), or if you have severe diarrhoea. TAKING THE STRESS OUT OF INCONTINENCE! For all those suffering in silence, it is time to speak out. There is no need to be embarrassed, it is surprisingly common – and like we have already mentioned, help is out there! You may not need to look very far. Your local physio may be able to help. The most common type of incontinence that we see and treat is stress incontinence. Although seen across both sexes, women are three times more likely to experience it than men. It is very common in women following pregnancy and childbirth (when the pelvic floor muscles get over-stretched, and sometimes even damaged), during menopause (due to hormonal changes) and in the elderly. It commonly affects men who have had prostate surgery. The pelvic floor muscles sit at the bottom of the pelvic bowl, spanning from the pubic bone to the tailbone (front to back) and from one sitting bone to the other (side to side). Imagine a tarpaulin stretched out with a person holding each corner and you kind of get the gist. When these muscles are strong, they help to support our internal pelvic organs (i.e. the bladder, bowel and the uterus in women) and wrap around the openings of the front and back passages, allowing us to control when we decide to do a number one or two. Following pregnancy for example, they may become weak and dysfunctional, and we can lose that ability to control voiding. It only takes something as small as a cough, or an activity like jumping or running (things many of us take for granted) that may cause a person to lose a small amount of urine. WHAT CAN BE DONE TO HELP? The most important thing to point out is that not all types of incontinence will improve or resolve with just strengthening of weak pelvic floor muscles. So, it is very important to get an accurate diagnosis, because there will likely be other factors that need addressing too. For instance, losing weight, stopping smoking, and making other lifestyle changes are just as important in the management of these conditions, if relevant to the person of course. Some people may also require release of tight and over-active muscles. Once you have your diagnosis, then strengthening may well be a part of your therapy. In order to strengthen, you need to know where the muscles are, and how to activate them. Below is a little step by step guide to getting a grip on those pelvic floor muscles (we don’t mean literally!): 1. Get in a comfortable position - try sitting or lying on your back and take a few breaths to relax.2. Imagine you are trying to stop yourself from urinating mid-stream by squeezing for about a second. If this is not easy to feel, next time you are on the toilet emptying your bladder, have a go at stopping mid-stream and then relaxing again to finish emptying (don’t hold it for too long please - just enough to feel which muscles you need to use).3. Do the same as step two for the back passage - this time imagine you are trying to stop yourself from passing wind by squeezing.4. Do these quick squeezes 3 x 20 reps a day. Once you’re comfortable, you can do it sitting or standing. Make it routine… Do it when you’re brushing your teeth, eating lunch, or in the ad breaks of your favourite TV show. These two contractions together form the basis of what you need to be able to do to begin your pelvic floor muscle training. If you struggle to feel this, then ask for help from your therapist. They will be able to help you perfect the activation of the correct muscles. We hope you have found this blog interesting and helpful. Please join in celebrating World Continence Week (17-23 June), References 1. Continence Foundation of Australia. 2019. World Continence Week. [Online]. [Accessed 07 May 2019]. Available from: https://www.continence.org.au/events_calendar.php/482/world-continence-week 2. Continence Foundation of Australia. 2019. Laugh Without Leaking. [Online]. [Accessed 07 May 2019]. Available from: http://www.laughwithoutleaking.com.au3. Continence Foundation of Australia. 2019. Key Statistics. [Online]. [Accessed 08 May 2019]. Available from: https://www.continence.org.au/pages/key-statistics.html4. Milsom, I. and Gyhagen, M. 2018. The Prevalence of Urinary Incontinence. Climacteric. 22(3). 217-222. DOI: 10.1080/13697137.2018.15432635. Continence Foundation of Australia. 2019. Pelvic Floor Muscles in Women. [Online]. [Accessed 08 May 2019]. Available from: https://www.continence.org.au/pages/pelvic-floor-women.html 4 June 2019 Read More -

You are what you eat......and exercise
Exercise and the gut by Martin Krause We've often heard the phrase 'you are what you eat', however, did you know that exercise can have a profound affect on the gut flora, which in turn affects the way we digest our foods? Regular exercise has been proposed to alter the gut microbiota and gut epithelium. Specifically, exercise has been shown to increase the butyrate-producing taxa and fecal butyrate concentrations and reduce pro-inflammatory cytokines and oxidative stress (Mailing et al 2019, Ex Sp Sc Rev, 47, 2, 75-85).. Further reading on gut biota and exercise The implications for the gut of regular exercise include affects on Colorectal cancer Inflammatory bowel disease (IBD) Obesity and metabolic disease Mental and cognitive health Cancer Some observational studies have suggested the physically active individuals have a 24% reduced risk of colorectal cancer (Torii et al 2010, Ann Clin Biochem, 47, 5, 447-452; Wolin et al 2009, Br J Cancer, 100, 4, 611-616). Suggested mechanisms include simple biomechanics of increased abdominal muscle activity, improving intestinal mixing and reduced intestinal transition time through activities as simple as running and walking. Increased bile duct activity, improved circulation due to short term ischaemic regulation, the release of myokines, metabolites, and neurendocrines which interact with the gut directly or indirectly through the gut-immune interface are all considered potential agents in the regulation of cell function. Additionally, increased butyrate production through exercise, which is metabolised in the mitochondria, stimulates the expression of genes involved in cell proliferation and cell turn over, which effectively strengthening the intestinal barrier (Andrianopoulos et al 1987, Anticancer Res, 7, 4, 849-852). Animal studies transplanting gut microbiota from exercised and non-exercised animals showed a more regnerative cytokine profile and higher levels of transforming growth factor (TGF-beta) and interleukin 22 (IL-22) gene expression in the distal colon (Tambaugh et al 2006, Nature, 444, 1027-1031). Read more on Cancer and the Immune System Irritable bowel disease Inflammatory bowel disease has been associated with increased abundance of Enterobacteriacae and reduced abundance of Roseburia, factors known to produce butyrate and induce redulatory T-cell formation, which is known to be important for immune function. Additionally, carbohydrate metabolism has been shown to be altered in the gut of people with IBD, whereas people who are physically active have increased SCFA (Short Chain Fatty Acids). Interestingly, positive gut changes in animal studies during voluntary wheel running were NOT replicated in forced treadmill running (Allen et al 2015, 118, 8, 1059-1066). Animal studies transplanting gut microbiota from exercised and non-exercised animals showed a more regnerative cytokine profile and higher levels of transforming growth factor (TGF-beta) and interleukin 22 (IL-22) gene expression in the distal colon (Tambaugh et al 2006, Nature, 444, 1027-1031). Obesity Obesity and metabolic disease has been shown to be related to gut microbiota in a seminal paper by Tumburgh et al (2018, Gut Microbes, 9, 2, 115-130) where they placed gut microbiota from obese mice into healthy mice and noted rapid weight gain. Read more on Exercise and Obesity "I have a gut feeling" "Exercise your mood" The existance of a gut-brain axis has been well established, whereby gut microbiota affect the vagal nerve receptors. Certain gut microbes are capable of producing neurotransmitters such as serotonin and GABA. GABA is the chief neuro-inhibitor in the central nervous system and typically has an anit-anxiety and relaxant affects, whereas serotonin is associated with mood and depression. Both substances can be derived from Lactobacillus species (Carabotti et al 2015, 28, 2, 203-209). People with depressive or anxiety disorders have a unique and predictive gut profile with increased plasma levels of markers associated with intestinal permeability (Stevens et al 2018, Gut, 67, 8, 1555-1557). Butyrate seems to increase neuroplasticity and has anti-depressant activity, boosting brain serotonin levels (Matt et al 2018, Front Immun, 9, 1832) Uploaded : 9 May 2019 Updated : 30 July 2021 Read More -

New Mothers
ATTENTION ALL NEW MUMS! May!!! We agree…. How is it May already? Well, May allows us to celebrate those very special people in our lives - our Mums. Being a parent can be very challenging at the best of times. And especially if you’re a new mum. It doesn’t matter whether it’s your first, second, or fifth child, being a new mum comes with a whole host of daily challenges. Your new little human requires all your attention - feeding constantly, changing eight nappies a day, bathing… Throw in another child, other family members, work, groceries (and the list continues) into the equation and it’s easy to see how life can be taxing on you and your body. The good news is, we’ve devised a little self-help guide for new mums! Below we give you tips on how to be kind to your body and not put yourself at risk of injury, so you can give your little munchkin the attention they need. FEEDING You’re going to be doing a lot of this. Your new recruit requires constant nourishment to ensure they grow strong and stay healthy. And it doesn’t matter whether you breast or bottle feed, it’s likely you are going to be seated for long periods, looking down at your baby. This all leads to extra strain through your neck, back and shoulders. So, try some of these little gems of advice to help keep this process pain free: 1. Get a comfortable, supportive chair - pick a chair that is going to feel good to sit in, but one you can easily get up and down from. If it’s too low, allowing you to slouch right back into, you’ll struggle to move yourself and your baby around without compromising your back.2. Keep your neck moving - feeding is a great time to bond with your baby. Eye contact is important but try not to spend the whole time looking down at a funny angle. Once your baby is comfortable feeding, it’s OK to break that eye contact every now and then to move your neck. Doing some light stretches will ensure you don’t end up with sore, overworked muscles.3. Consider a feeding pillow - these are great for taking the weight of your baby, so your shoulders and arms don’t have to. And they still allow you to have that important close contact.4. If you have a partner who can help feed, allow them to help regularly to give you a break. This tip is more for the bottle feeders of course, but it can make a huge difference. CHANGING It’s going to be nappies galore! This can mean a lot of bending over, so it’s important you look after your posture so your lower back doesn’t take all the strain. Try to avoid changing your baby on the floor in these early days. Ideally, get yourself a changing table. It means you can place your baby down on the table and change them at a height where you don’t have to bend forward and hold an awkward position. And of course, the same advice can be followed when changing your baby’s clothes. Look after that back, you’re going to need it! OTHER USEFUL TIPS The following tips are by no means any less important, so try to take these on where possible: 1. Sleep when your baby sleeps: Getting those extra hours in when your baby is taking a nap is important to conserve your energy and reduce the risk of fatigue.2. Eat and drink well: It’s easy for the focus to turn to your baby, and rightly so, they are little and dependent on you. Remember though, you can’t look after your baby if you aren’t well. Eat for the health of you and your baby - lots of water and good nutritious food such as fruit and vegetables!3. Stretch: Especially your shoulders, neck and chest. Once baby comes along, our arms are always in front of us. Whether it’s holding, feeding, changing or playing, we’re usually a little slumped in our shoulders. Build stretching into your routine (like every time after baby feeds for example). We want to reverse the ‘slump’ position, so take your arms out wide, open up your chest and hold for 30 seconds (and repeat). Aim to do this three times a day (or whenever you get the chance!). Gentle shoulder shrugs and neck stretches can also help.4. Take time to relax: When the opportunity arises, get your partner, grandparent or friend to look after your newborn while you take a bath, read a book, or close your eyes for a little while. You deserve it, and it helps keep you sane and grounded during a very busy period in your life. 5 May 2019 Read More -

Female hormones and knee strength
Female Hormones and Knee Strength Endurance exercise and mid luteal phase of the menstrual cycle Investigators have found that aerobic athletic performance is compromised during the mid-luteal phase compared with the mid-follicular phase of the menstrual cycle (Freemas JA et al 2021 Med Sc Sp Ex, 53, 2, 442-452) Muscle activation around the patella and the menstrual cycle The initial firing rate is lower in the VMO (vastus medialis oblique) compared with VM (vastus medialis) in women not men. The firing rate is affected by the menstrual cycle, showing increases in initial firing during the early follicular phase through to the late luteal phase. The initial firing was lower in VMO compared to VM during ovulatory and midluteal phases (Tenan et al 2013, Ex Sc Sp Ex, 45, 11, 2151-2157). This could play a bearing on anterior knee pain due to an increased lateral gliding of the patella over the femur, leading to patellofemoral syndrome. Anterior cruciate ligament (ACL) and the menstrual cycle Women are 2-8 times more likely to rupture their ACL than men, suggesting a hormonal mechanism behind this observation (Konopka et al DOI:10.1177/0363546516646374). The ACL is designed to prevent forward shearing of the shin bone (tibia) on the thigh bone (femur). Anterior knee laxity (AKL) and hyperextension of the knees were shown to be significant predictors of anterior tibial translation (ATT) in both males and females. Interestingly the restraining structures to knee hyperextension are the posterior cruciate ligament (PCL) and popliteus muscle, suggesting that the knee in non weight bearing is in a relative posterior position and hence allows for greater total anterior excursion of the tibia. Notably, if a females ACL changes as much as 3mm across her menstrual cycle the ATT changes by 2mm which represented a change of approx 30% in mean magnitude of the ATT (Schultz et al 2011 Med Sc Sp Ex, 43, 2, 287-295). Furthermore, in another investigation, the same authors demonstrated increased absolute and relative magnitudes of multiplanar knee laxity changes. These were seen as increased valgus coupled with relatively greater external rotation of the tibia, making the knee more susceptible to injury on ground contact and early in the landing phase (Schultz et al 2012 Med Sc Sp Ex, 44, 5, 900-909) Women on the contracetive pill and ACL injuries Researchers looking at US insurance claims between 20007 and 2017 found that women on the pill were less likely to have an ACL injury whilst playing sport. Reconstructive knee surgery was performed on 569 out of 82874 women who were not on the pill versus 465 out of 82874. Thus the synthetic oestrogen and progesterone hormone were considered protective against knee injuries (De Froda et al 2019,The Physician and Sports Medicine, April) ACL injuries in football https://www.back-in-business-physiotherapy.com/sports-performance/knee-injuries-in-soccer.html Uploaded : 5 May 2019 Updated : 24 July 2021 Read More -

Thrombosis and caffeine intake during exercise
Caffeine augments the prothrombotic but not the fibrolynic response to exercise Development of clots pose a risk of cardiovascular and cerebrovascular accidents. Prothrombotic (clotting events) and fibrolynic (clot dissolving) can be influenced by altitude (thicker more viscous blood), inactivity (plane flights), genetics (haemochromatosis, prothrombin factor and/or Leyden's factor V), and paradoxically caffeine ingestion around exercise. Investigators studied the affect of a single dose of caffeine during a single acute high intensity. They found the fibrolynic effects of exercise were not affected by caffeine. However, caffeine did increase coagulation factor VIII, which suggests an elevated risk of clotting (Nagelkirk et al 2019, Med Sc Sp Ex, 51, 3, 421-425). 4 April 2019 Read More -

Sodium Hyaluronate and Platlet Rich Plasma (PRP) for partial thickness rotator cuff tears
Sodium Hyaluronate and Platlet Rich Plasma (PRP) for partial thickness rotator cuff tears Investigations have demonstrated improvements in pain and function, in small to medium sized supraspinatus tendon tears, up to 12 months after PRP and Sodium Hyaluronate injections, in 45 people who received PRP injections and 48 people who had a combination of sodium hyaluronate and PRP injections (Cai et al 2019, Med sc Sp Ex, 51, 2, 227-233). Read more on Rotator Cuff Injuries 21 March 2019 Read More -

Three favorite exercises
Three favorite exercises 1. Walking and runningA classic! An oldie, but a goodie, walking or running is a great all over body exercise. It works lower and upper leg, your buttocks, core, and even your arms! If you’re not much of a mover, start small with 15-minute walks, and build it up over time. Once you’re happily walking 30 minutes, start doing intervals, like running for 30-seconds and walking for two minutes (or more). Over time, increase your running time, decrease your walking time and soon enough you’ll be jogging for 30-minutes flat! Runners – interval training is great to mix up your training too. Try running at 90% effort for a minute, and then jogging for a minute. Play around with your run/jog times depending on your fitness and goals. 2. Squats These are a very popular exercise, and for good reason. These strengthen your lower body and back. Start with no added weights to ensure you have good technique. Stand with feet shoulder width apart. Keeping your back straight, push your bottom outwards to mimic sitting in a chair - try to keep your weight through your big and little toes, and your heels. When your thighs are parallel with the ground, return to the start position giving your buttocks a squeeze on the way back up. Keep your knees over your toes (which should point forward) – don’t let your knees waver in or out! A good progression is to add weight when you are ready; start with 1-2kg in each hand (or use bottles of water or books in shopping bags!) and work your way up! Eventually you can add weighted arm movements during or after your squat to get that whole-body work out. You can also do squats while brushing your teeth or waiting for the kettle to boil! 3. Box Jumps or step ups This is another lower body exercise but is also a great calorie burner and really engages the whole body to perform. You need a box (we strongly advise against cardboard ones!) or a strong raised surface that will take your weight with no issues (like a step/platform). Jump up onto the box, landing with both feet and raise to a standing position. Then jump back down and repeat. Start slow and low and build up to faster and higher jumps. Of course, if you aren’t quite at jumping yet, or you have any lower body injuries or heart problems, try stepping up and down to start. Try not to let your weight shift side-to-side too much as you step up. Start by doing 3 x 30secs, building up to 3 x 1-minute sets. Or try 3 x 10 jumps, building up to more as you progress. Make sure your knees and toes point forward, and if in doubt, start small! Uploaded : 16 March 2019 Read More -

What pain relief is right for you?
What pain relief is right for you? Pain has been a huge topic for discussion for a long time now. Nearly everyone feels it (I say ‘nearly’ because there is actually a very small minority of people with a special condition that does not allow them to feel pain), and it varies in character and severity depending on what part of the body is implicated. And for the most part, none of us like being in pain. When we feel pain, normally the first thing we do is to look for a way out of it (of course a small minority just ignore it - tut tut!). It’s a bit of a minefield knowing where to go for good pain relief. Some of us like a quick fix, others are more interested in fixing the problem long term by putting the hours in. When it comes to the body, we usually feel pain because our body is sending us a signal letting us know something is not quite right. That might be down to a simple muscle imbalance or joint restriction, which is leading us to walk or run differently. Or it might be down to something more serious like a tear of a muscle or tendon, or a problem with an organ deep inside the body - the list of causes is long and complex. Now once we have pain, we want to know how to get rid of it. A lot of us turn to the experts (i.e. manual therapists such as your local physio/osteo/chiro [delete as appropriate], and other professionals like doctors), and some of us like to self-diagnose using www.DrInternet.com (do this at your peril!). So, what is out there to help us relieve our pain? Some of the most common and well-known forms of pain relief include manual therapy, use of temperature, and numerous medications - you’ll find a brief overview of each below: Manual therapy Us humans have been using our hands to treat the body for a very, very, very long time! If you walk into a clinic in pain, be it you have a swollen ankle or the inability to lift your arm above your head, your therapist will get to work on you using a whole host of techniques (after they have carefully and correctly diagnosed you of course!). Soft tissue massage and release techniques are widely used in the management of musculoskeletal pain, and evidence suggests you aren’t wasting your time by getting the help of your local therapist. Your therapist may also utilise other techniques, including joint mobilisation and manipulation, to correct your problem and to help get your pain lowered and under control. Usually you will also be given some form of flexibility or strengthening exercise to perform between treatment sessions to back up what happens in the treatment room. Heat and cold therapy If you’ve hurt yourself in the past, there is a good chance you’ve tried some form of treatment relating to temperature to help relieve the pain. It’s difficult to know whether it’s best to use heat or cold therapy, but the following principles are pretty safe to follow. Cold therapy can help to reduce pain, blood flow, swelling, muscle spasm, and inflammation. Heat therapy can help to relieve pain, increase blood flow, and tissue elasticity. Although more evidence is needed to support the use of these therapies in certain scenarios, it may help, so it’s worth getting the advice from your local physio/osteo/chiro [delete as appropriate] for the best route ahead. Medication There are countless different medications out there that can help with pain relief - these are called analgesics. Without getting too complicated, they can generally be split into Non-opioid and Opioid analgesics. Non-opioid analgesics include your well known and easily accessible medications such as aspirin, paracetamol, and anti-inflammatories (such as Ibuprofen) - these are generally good for the control of musculoskeletal pain. Opioid analgesics are there for cases of more severe pain, and include codeine, tramadol and morphine (you won’t be able to get these ones over-the-counter though!). Remember it’s always safest to consult a medical professional before using any form of medication. We hope this has been a helpful overview to read. If you are injured or in pain, we advise you to book a consultation with us so we can talk through your problem, assess you thoroughly, and then advise the best course of action for you. Our aim is to help get you out of pain and moving better again! Say ‘au revoir’ to pain! Uploaded : 25 Feb 2019 Read More -

Why your body is like a chain
WHY YOUR BODY IS LIKE A CHAIN The concept that the human body is like a chain has been around for a long time. The body is a complex network of systems that all work together to allow us to move and do the things we like to do. When referring to movement, most people straight away think of muscles, bones and joints. However, there are a whole host of structures required to function together in order to produce movement. The musculoskeletal system is primarily associated with movement. From head to toe, our bones are joined at various points called joints, which are held together by strong structures called ligaments. Muscles then attach to bones via tendons and the muscles exert forces on the bones, which basically causes a joint to move. But, without blood and electrical stimulation, the muscles themselves cannot function to exert that force on the bones - so the circulatory system (which carries the blood around the body) and neurological system (where nerve impulses travel around the body) play just as important roles. Of course, the overall picture is much more complex than this, but you can see how you need lots of different elements to work together so our bodies can do what they have evolved to do – MOVE! Us humans are what we call bipedal, which means we walk upright on two feet. Other animals that do this are birds (when they are walking and not flying of course) and apes (although not all the time). Even cockroaches and some lizards sometimes move bipedally (usually when running at full speed), and of course, our native Kangaroos hop and jump in the same fashion. Think back millions of years to Mr T. Rex, who also walked around on his two back legs – it has been around a long time! Unless we move around on our hands and knees (which we don’t tend to do much after learning to walk from a young age), our main contact points with the Earth are our feet. And once we have learned to hold that upright posture, our body acts as a chain from feet to head to allow us to function as humans - get up, go to work, drive, play sports, eat our meals, and so on… If something goes wrong somewhere in that chain of muscles, bones, joints and systems, then it can lead to the whole or parts of the chain becoming dysfunctional. And when we have dysfunction in the body, it quite often leads to pain. For example, you have flat feet or collapsed foot arches – this means your feet tend to roll in. Now because the foot bone’s connected to the leg bone, and the leg bone’s connected to the thigh bone (sing along!), the flatness of your feet directly affects what is going on above in the ankle, knee and thigh. The leg and thigh bones must compensate for the lack of foot arch, which will commonly mean the knees fall inwards and you may end up with a case of knock knees. Flat feet may not cause pain in the feet themselves, but it’s very possible that knee or hip pain (areas further along the chain of the body) could be caused by such a problem. However just remember that many people who have flat feet have no pain whatsoever, so just because you have flatter feet than your friend, it doesn’t mean you are going to get pain. It just means you may be more susceptible to certain conditions because of the extra stress on the body’s structures (e.g. muscles, ligaments, joint surfaces) due to the compensations it has had to make. The body will compensate well for you, but there is always a point where the body will start to tell you it needs some help. Pain is usually the first sign of this! Often manual therapy - soft tissue release, joint mobilisation/manipulation – and some form of strengthening exercises will get the body back on track to reconnecting the chain to its former glory. In the case of flat feet, you may need some form of orthotic in your shoe too. It’s at this point where you start to feel better and can get back to playing your sport, or even just getting in the car to drive to work without being in pain. All the elements start to function together again, the body can move without, or at least with less, compensation, and that equals a much happier you. So, if you think you have a little kink in your chain, don’t take it to the jewelers to get fixed. Book in for an assessment, treatment, and some expert advice on how to manage your problem. You’ll be back roaring like a T-Rex in no time. Roar. Uploaded 16 feb 2019 Read More -

Beetroot Juice Increases Human Muscle Force
Beetroot juice increases human muscle force Beetroot juice has been shown to improve low frequency muscle force independent of Calcium-handling-proteins or REDOX reaction (Whitefield et al 2017, Med Sc Sp Ex, 49, 10, 2016-2024). Further benefits of beetroot juice are thought to include reduction of blood pressure protection from pre-mature aging aiding cancer survival lowering serveral inflammatory markers including interleukin-6, C-reactive protein and tumor necrosis factor alpha stabilising blood suger improving sexual performance anti-arthritic effects blood purification and enhanced red blood cells removing 'bad' estrogens from our blood stream Uploaded : 18 November 2017 F Read More -

YouTube videos
Take a look at our YouTube Channel Read More -

Neuroplasticity in Tendon Dysfunction
Neuroplasticity in Tendinopathy by Martin Krause A multitude of contributing factors to altered motor control must be addressed when treating tendon dysfunction. What we have failed to consider in the past when dealing with chronic or recurrent tendon issues are motor control problems encompassing corticospinal control of excitation and inhibition as well as belief systems about pain and contextual factors related to imaging. Research by Ebonie Rio et al (2015) (BJSM Sept 25, 10.1136/bjsports-2015-095215) suggest that the pain state sets up an adaptive pathway whereby the ipsilateral kinetic chain is directly inhibited by reflexogenic pathways, as well as being inhibited by contralateral hemispheric activity. Simultaneously excitation is enhanced in the opposite limb as well as in antagonists...at least in the case of enhanced excitation of the hamstrings in quadricep tendinopathy. If this is true, then so much for training the contralateral limb for 'cross training' purposes! This may also explain why a lot of people seem to have "all their injuries on the same side" (of the body). Furthermore, they recommend enhancing corticospinal drive through the use of 30-60 second isometric holds at 70-80% MVC to load the muscle whilst using isokinetics to load the tendon. Moreover, they recommend the use of a metronome at 60bpm (stages 1 and 2) with a count of 3 up, 2 down for quads, and 2 up, 3 down for calf isokinetics to optimally engage corticospinal drive through the visual and auditory stimuli (also shown by Kohei et al 2012 for motor imagery and M1 stimulation) .....read more Cortical mapping of infraspinatus muscle in chronic shoulder pain demonstrating higher motor thresholds (aMT= activation MT) and hence reduced excitability on the affected side (39 vs 35) (Ngomo et al 2015 Clinical Neurophysiol, 126, 2, 365-371) Cortical mapping of pain and fear. Lots of overlap suggesting that taking away the fear from the pain with clear clinical explanations and a focused goal directed program using specific functional outcomes is important. Individuals with patellofemoral pain (PFP) had reduced map volumes and an anterior shift in the M1 representations, greater overlap of the M1 representation and a reduction in cortical peaks across all three quadriceps (RF, VL, VMO) muscles compared with controls.(Te et al 2017 Pain Medicine, pnx036, https://doi.org/10.1093/pm/pnx036) Uploaded : 18 October 2017 Read More -
Imaging
Do I need a scan? "a picture tells a thousand words" - not really! by Martin Krause A scan, in it's self, will not improve anyone's condition. The purpose of a scan is to gain more information about the pathology. Sometimes this information may be irrelevant to the management of a patient's condition. For example, if you knocked your elbow on a door frame and suffered a bruise, which was already beginning to resolve, an ultrasound scan may show some minor soft tissue damage, but that was already obvious by the fact of the bruise, and the information gained from the scan has not helped nor changed the management of the bruise. Therefore, the main reason for getting a scan would be because there is concern that the presence of certain pathologies may lead to a change in the medical management. For example, sometimes a rolled ankle can be more than sprained ligaments, and may require surgey or immobilisation in a boot. If the therapists suspects this might be the case, then they will recommend or refer for a scan (probably an X-Ray) to check the integrity of the bones (especially the fibular and talar dome), because if there is no bony damage then the patient can be managed conservatively with taping, exercises, ultrasound, massage, joint mobilisations etc. However, if there is boney damage, for example, then it might be necessary for the ankle to be immobilised in a boot for three - six weeks, for example. This dramatically different medical management depends on the results of a scan, and it is therefore worth doing. However, scans have no predictive value to the presence or severity of pain. Thirty-three articles reporting imaging findings, in the low back, for 3110 asymptomatic individuals were investigated for pathology. The prevalence of disk degeneration in asymptomatic individuals increased from 37% of 20-year-old individuals to 96% of 80-year-old individuals. Disk bulge prevalence increased from 30% of those 20 years of age to 84% of those 80 years of age. Disk protrusion prevalence increased from 29% of those 20 years of age to 43% of those 80 years of age. The prevalence of annular fissure increased from 19% of those 20 years of age to 29% of those 80 years of age. (Brinjikji, W et al Spine Published November 27, 2014 as 10.3174/ajnr.A4173). Hence, the results of imaging need to be assessed within the context of the entire clinical picture. Frequently too much emphasis is placed on the imaging not only by the clinician but also by the patient. Some people react to pathology seen on scanning as an affirmation of their problem and can either use it to gain clarity and become better or conversely become worse. Moreover, some people find imaging with inconclusive results as a 'panic moment' - "no one knows what is wrong". Similarly, ultrasound imaging of the tendond has good predictive diagnostic and aids in clinical reasoning when it comes to full tears. However, with partial tears it is a totally different 'ball game'. Ultrasound is highly user dependent, with specifically trained musculoskeletal radiologists able to produce high-quality images that may provide more clinically relevant information than those produced by clinicians with less experience in imaging. Sean Docking, a leading tendon researcher at Monash University, cited 7 authors who found pathological tendon chnages in 59% of asymptomatic individuals, whereas he found that 52% of asymptomatic elite AFL sportsmen had tendon pathology on imaging! Furthermore, symptomatic individuals who improved clinically to the point of resuming play, weren't shown to have improvements on imaging. Again, the clinical context and the clinical reasoning can in many instances prove to be the 'gold standard' not the imaging itself, when considering management options. Shoulder supraspintatus tendon pathology, in the abscence of trauma, is known, in many instances, to be a disorder of immune-metabolic compromise of the tendon and bursa. Imaging may show some changes in signal intensity but, unless it's a complete tear, it can reveal neither the intensity nor the severity of pain when taken outside of the clinical context. A thorough physical and subjective examination integrating all the clinical dimensions of the problem will have far greater value than any one single imaging modality. Yet, imaging still should be used in instances of progressive rapid deterioration and suspected serious pathology which may require surgery and/or immediate medical intervention. In summary, sometimes it is worthwhile getting a scan, because the information gained from that scan will determined the type of medical management that is employed. However, at other times, the scan may be unneccessary, because the information may be irrelevant or lead to an incorrect change in medical management, due to over-reporting of 'false positives'. You will be able to make this decision on the advice of your health care professional. On occasions it can actually be detrimental to have a scan, because some patients can become overly obsessed with the medical terms used to describe their scan results, which then can become the major focus for the clinician and the patient, rather than the more prefereable focus on their symptoms and functional abilities. For example, many people have lumbar buldging discs yet have no symptoms, yet sometimes when these patients have an MRI or CT scan, they can develop symptoms because they think they should have pain if the scan says so! Conversely, for some people the results of imaging can have a positive and reassuring affect. Therefore, it is very important to assess a clients attitude to scans before prescibing them so that the patient's expectations are managed appropriately, and not burdened by the additional, sometimes confusing, information supplied by a scan. Uploaded : 10 October 2017 Read More -

Physiotherapeutic Implications of Post Concussion Syndrome
Neck aetiology, autonomic and immune implications, exercise and diet in the musculoskeletal physiotherapy management of Post Concussion Syndrome (PCS) - a clinical case study with associated research commentary by Martin Krause, MAPA, Titled member Musculoskeletal Physiotherapy Association of Australia A 14 year old boy presented to A&E, in August 2016, after receiving an impact to the head during AFL (Australian Rules Football League). Although his SCAT3 scores were relatively mild, he went on to suffer severe lethargy, resulting in a lengthy absence from school, culminating in a return to school for exams in the first week of December 2016. By December, even a 30 minute walk was extremely fatiguing. To place this into perspective, he had been playing elite academy grade AFL for several seasons and was an extremely fit outdoor adventurer. Confounding Variables : end of season injury and hence no follow up from the academy suffers from Hypermobile Joint Syndrome (HJS) and possibly Ehlers Danlos Syndrome (EDS), however Beighton score 4/9. suffers from food intolerances, particularly to Glutin and diary, but also some other foods. Potential IBS and autoimmune issues. had just gone through a growth spurt (190cm) EDS is considered a soft tissue disease, Additionally, people suffering from EDS frequently have concomitant autonomic dysfunction including POTS (postural orthostatic tachycardia syndrome). Imaging : Brain MRI normal Medical Examination : Balance remained impaired to tandem walking and single leg stance. The vestibular ocular motor scale showed significant accommodation deficit of 15cm and there was a mild exacerbation of symptoms. ImPACT testing revealed adequate scores and reaction time of 0.65 which is within acceptable range. History : School holidays December - January. Return to school and was placed in the lower academic classes. Prior to his concussion he was a top 10 student at an academically selective high school. Took up basketball and rowing as summer sports. Academic results tanked. Several lower limb Basketball injuries (Feb - April 17') as a result of what appeared to be muscular imbalances from the relatively recent growth spurt, as well as taking on a new sport. Showed little interest in returning to AFL as no-one from the AFL academy had followed up on his recovery (or in this case lack of recovery). Current History : September 2017 showed a continued decline in academic levels. School teachers noted an inability to concentrate. Academic results still well below pre-concussion levels. Fatigue continuing to be problematic. Stopped going to school for 7 weeks due to another head impact, but this time at Basketball. Literature Review : Post Concussion Syndrome (PCS) is defined as "cognitive deficits in attention or memory and at least three or more of the following symptoms: fatigue, sleep disturbances, headache, dizziness, irritability, affective disturbance, apathy, or personality change" Adolescents have been found to have impaired dynamic cerebral autoregulation after concussion that improves along with clinical signs and symptoms in some individuals, whilst remaining impaired in others (Moir et al, 2018 Med Sci Sp Ex,,50, 11, 2192-2199). Moreover, it would appear that measurement of dynamic intracerebral blood flow latency in reaction to changes in position from lying to sitting to standing was more sensitive than static intracerebral blood flow monitoring. This interaction myogenic vasomotor response occurs at a vascular-astrocytic level. Of the 19 people in their investigation, 2 demonstrated complete recovery at 28 days post incident, whereas 7 experienced little change in intracerebral blood flow from the first to last visit (32 + 14 day). Surprisingly, there appears to be a greater incidence of concussion amongst females (Moir et al 2018; Halstead et al 2010, Pediatrics, 126, 3, 597-615; Dick et al, 2009, Br J Sports Med, 43, Supp, i46-50) Post concussion dizziness severity predicts step count during recovery. Investigators found that the initial subjective dizziness ratings, but not subjective or objective postural stability measures or overall symptom severity, predict physical activity volume in the subsequent 2 weeks after initial concussion evaluation ( Smulligan KL et al 2022 Med Sc Sp Ex, 54, 6, 905-911). For every one point increase in dizziness rating (range 0->5) there was an approximate 1000 steps/day decrease. Given that exercise volume > 160min/wk is associated with improved post concussion outcomes (Howell DR et al 2021, Am J Sp Med, 49, 7, 1912-1920), dizziness may be limiting factor contributing to non-optimised recovery. Physiotherapeutic intervention including occulomotor training and cervical joint mobilisatons have been advocated for the treatment of dizziness - see below (Reneker JC et al 2017 Scan J Med Sci Sports, 27, 12, 2009-18; Schneider KJ et al 2014, Br J Sports Med,48, 17, 1294-8) , One of the known risk factors for Sport Related Concussion (SRC) is a history of prior concussion (Collins et al 2002. Neurosurgery, 51, 5, 1175-9. Inversen et al 2004, Brain Inj, 18, 5, 433-43). Cumulative effects exist with three or more prior concussions but not with one or two concussions (Inverson et al 2006, 40, 1, 72-75) . Although, most adults recover from concussion after 10 days, there is evidence to suggest ongoing abnormalities in the brain can persist well beyond 10 days (Prichep et al 2013, J Head Trauma Rehabil, 28, 4, 266-273). Thus, with the above described symptoms and potential motor control problems, further complications of PCS also appear to be altered proprioception, an increased risk of musculoskeletal injury which in turn can lead to SRC. The following are the results from soccer players. Nordstrom et al (2014, BMJ Sports Med, 48, 19, http://bjsm.bmj.com/content/48/19/1447) Visuomotor reaction time (VMRT) responses and whole body reactive agility (WBRA) have shown neuromechanical deficiencies in elite athletes who reported a history of concussion (Wilkerson et al 2018 Med Sc Ex Sp, 50, 9, 1750-1756). Dual task performances creates competition for neuronal cognitive resources required for higher executive function. Among demands placed by sport on the executive function are visuospatial processing, which can be crucial for management of environmental interactions. Deficits in dual task VMRT have been associated with both a history of concussion and subsequent musculoskeletal injury occurrence.(Wilkerson et al 2017, Cirr Sports Med Rep, 16, 6, 419-427). Sensory organisation test (SOT) balance scores show significant relationships with reaction time and executive function in people suffering concussion (Van der Vegt et al 2019, Med Sc Sp Ex, 51, 2, 264-270). Notably, the ability to use sensory information to adapt motor responses with varying environmental demands is essential for sport safety and performance. Predictors of PCS are uncertain. However, the following clinical variables are considered factors at increasing risk. These include prior history of concussion, sex (females more prominent), age, history of cognitive dysfunction, and affective disorders such as anxiety and depression (Leddy et al 2012, Sports Health, 4, 2, 147-154). Genome-wide association study for concussion risk Investigators, using a GWA analysis from wo sets of data from the Kaiser Permanent Research Bank (KPRB) and the UK biobank (n=291472 cases), identified two genetic markers as a potential risk factor for concussion (Kim SK et al 2021, Med Sc Sp Ex, 53, 4, 704-711). One of the genes encodes 'plexin' which is thought to transduce signals to steer axonal growth (Jensen et al 2012 Nat Struct Mol Biol,19, 12, 1293-9). Interestingly, they found that in the RPGEH group being female and weighing less was associated with a greater risk of concussion; whereas, in the UK biobank cohort, they found the opposite, being male, heavier weight and taller resulted in greater risk of concussion. The latter is significant in so far, as other researchers have found increased time to recovery, to baseline sports related concussion, in obese individuals (Lee YM 2016 et al Phys Sportsmed, 44, 3, 217-22). In this case, he was neither female nor obese, but instead had an athletic morphology. However, at 192cm and 70kg, he had a teenage body whose muscles hadn't filled out into an adult body yet. His head size was large compared to his neck musculature, being a long neck. Graded exercises Unlike the 'good old days' which recommended a dark room and rest for several weeks post concussion, the consensus appears to be a graded return to exercise in order to restore metabolic homeostasis. Disconcertingly, highly trained young individuals can find even exercises in bed extremely demanding in the presence of sport related concussion (SRC). Kozlowski et al (2013, J Ath Train, 48, 5, 627-635) used 34 people, whereby 226 days post injury to conclude significant physiological anomalies in response to exercise which may be the result of 'diffuse cerebral swelling'. Researchers have noted lower systolic and higher diastolic blood pressure in PCS (Leddy et al 2010, Clin J Sports Med, 20, 1, 21-27). Due to autonomic dysfunction manifested in altered cardiovascular and pulmonary responses (Mossberg et 2007, Arch Phys Med Rehab, 88, 3, 15-320), whereby some clinicians have recommended the use of the exercise program for POTS (Postural Orthostatic Tachycardia Syndrome). This is a 5 month program which recommends mainly exercise in the horizontal and sitting positions for 1-4 months, including recumbent bike, rowing ergometer and swimming laps or kicking laps with a kick board. Month 4 upright bike and Month 5 upright training such as a elliptical trainer or treadmill. The Modified Dallas POTS Exercise Program can be found here. Other progressive exercise therapies have also included 20 minutes per day, 6 days per week, for 12 weeks of either treadmill or home gym exercises at 80% of the heart rate at which their concussion symptoms are exacerbated. Their programs were individually modified as the heart rate provoking symptoms increased. When compared to the 'control group', this intervention was shown to improve cerebral perfusion on fMRI, increase exercise tolerance at a higher heart rate, less fatigue and were showing activation patterns in areas of the brain on performing math processing test which were now normalised (Leddy et al 2010, Clin J Sports Med, 20, 1, 21-27). Graded exercises could also have included 'motor imagery' as espouse by the NOI group and the work of Lorrimer Moseley (University South Australia) when dealing with chronic pain. Exercise Dose (literature review by Howell et al 2019, Med Sc Sp Ex, 41, 4, 647-652) Frequency : 5d/wk of moderate intensity or > 3 d/wk of vigorous intensity Duration : 30-60 minutes/day (150min/wk) at moderate intensity or 20-60 minutes (75 min/wk) of vigorous intensity Mode : exercise using major muscle groups eg walking, jogging, cycling or swimming Volume : > 500-1000 MET/min/wk (MET = 3.5 ml O2/kg/min) Pattern : exercise is performed ideally in one continuous pattern; however multiple sessions of > 10min can be performed to accumulate the desired total duration and volume of exercise Progression : Gradual progression of exercise volume by adjusting duration, intensity and/or frequency is recommended to gain continued aerobic fitness improvements Ongoing Symptoms : The literature review by Leddy et al (2012) found that ongoing symptoms are either a prolonged version of concussion pathophysiology or a manifestation of other processes, such as cervical injury, migraine headaches, depression, chronic pain, vestibular dysfunction, visual disturbance, or some combination of conditions. Anatomical considerations : Extensive anatomical connections between the eyes, neck and vestibular system (Wallwork et al 2007, JOSPT, 37, 10, 608-612) allow sensory information from neck proprioceptors to be processed together with vestibular information which, via the lateral vestibulo-spinal tract, affect the control of postural muscles such as the deep trunk muscles (Hain 2011, Neuro-Rehabilitation, 29, 2, 127-141). Psychological considerations : The Kubler Ross model of grief are applicable when it comes to chronic sports injuries. Mental health among athletes is an important consideration that has recently gained more attention. The 2019 International Olympic Committee (IOC) consensus statement on mental health in athletes reported on the high prevalence rate of mental health symptoms in athletes and the relationship of mental health with physical injury and subsequent recovery (Reardon CL et al 2019 Br J Sports Med. 53, 11, 667–699). The IOC urged that mental health is a vital component of athlete well-being and cannot be separated from physical health. Assessment of mental health and subsequent management should be a routine part of the medical care of athletes. The IOC also concluded that cognitive, emotional, and behavioural responses are important factors in injury outcomes, and mental health disorders can complicate recovery. A systematic review of 28 studies reported 65% of those patients not returning to play cited a psychological reason for not returning (Nwachukwu, BU et al 2019 Orthop J Sports Med. 7, 5, 23259 67119845313). Fear of reinjury, lack of confidence in the knee, and depression were the most commonly cited psychological reasons. Physiotherapy Assessment : One year PCS, fatigue continued to persist. Cognitive deficits with school work were reported to becoming more apparent. Assessment using various one leg standing tests employing oscillatory movement around the hips and knees for kinetic limb stability and lumbopelvic stability, which had been employed 6 months previously for his Basketball injuries were exhibiting strong deficits, despite these being 'somewhat good' previously. Significantly, during the acute phase of SRC, rugby union and rugby league players have been seen with alterations of both balance strategies and motor control of the trunk (Hides et al 2017, Musculoskeletal Sci Pract, 29, 7-19). Investigators (Lempke et al 2020, Med Sc Sp Ex, 52, 8, 1650-1657) comparing clinical reaction time (RT) assessments with functional RT found little correlation. Clinical RT assessment included computerised evaluation of simple and complex RT, Stroop RT, composite RT and Drop Stick. Functional assessment included gait, jump landing, single-leg hop, anticipated cut and unanticipated cut. This implies clinicians may not be sensitive to the functional RT required for safe and effective sports participation, potentially leading to further musculoskeletal injury, during post concussion return to sport. Interestingly, they found dual task RT quite sensitive to physical and cognitive deficits. A sweet spot may exist for dual tasks between those which are too easy (hockey puck drop stick) and those which are too hard (unanticipated cutting). Furthermore, they observed that the single leg hop RT may be a very useful test, as the transition from a dynamic movement to a static position is a relatively unaccustomed and hence un-practiced task, thereby minimising deficit masking through learning effects. Physical Examination : cervical and thoracic spine Due to the Joint Hypermobility Syndrome (JHS) it was difficult to ascertain neck dysfunction based on range of movement testing. ROM were unremarkable except for lateral flexion which demonstrated altered intervertebral motion in both directions. Palpation using Australian and New Zealand manual therapy techniques such as passive accessory glides (upslopes and downslopes and traction) exhibited muscles spasms in the upper right cervical spine. In particular, the right C1/2 regions demonstrated most marked restrictions in movement. Eye - Neck proprioceptive assessment using blind folds and laser pointer also revealed marked variance from the normal. Repositioning error (RPE) using the laser pointer with rotation demonstrated marked inability to reposition accurately from the left, tending to be short and at times completely missing the bullseye. Gaze stability with body rotation was NAD. Gaze stability whilst walking displayed some difficulty. Laser pointer tracing of the alphabet was wildly inaccurate and cognitively demanding. Thoracic ring relocation testing also revealed several anomalies, which may have also accounted for some of the autonomic dysfunction observed. Occulomotor assessment and training Upper Cervical Spine : The upper cervical spine (atlas and axis) represents approximately 50% of the available rotation. An investigation into the environmental and physiological factors affecting football (soccer) head impact biomechanics found that rotational acceleration was one of the few factors approaching significance and concluded that more research should be undertaken to evaluate this (Mihalik et al 2017 Med Sc Sp Ex, 49, 10, 2093-2101). Headache : Commonly referred to as cervicogenic headaches, one in five headaches in the general population are thought to be due to the cervical spine. The Upper Cervical Spine is particularly vulnerable to trauma because it is the most mobile part of the vertebral column, with a complex proprioceptive system connecting the vestibular apparatus and visual systems. It also coincides with the lower region of the brainstem and fourth ventricle. The brainstem houses many neurones associated with autonomic responses to pain and balance. Imaging of the fourth ventricle for swelling of the 'tonsils' and Arnold Chiari malformations are recommended when symptoms persist. In particular, children and adolescents are more vulnerable to neck contusions due to the proportionately larger head and less developed musculature. Cervical vertigo and dizziness after whiplash can mimic symptoms of PCS.. Mechanoreceptor dysfunction and vertebrobasilar artery insufficiency should be part of the differential diagnosis. Mechanical instability of the Upper Cervical Spine should also not be missed. Cervicogenic Headaches Further Interventions : Neurocognitive rehabilitation of attention processes. Psychological intervention using cognitive behavioural therapy (CBT). Neuro-opthalmologist to assess and treat smooth pursuit eye tracking. Naturopath for food intolerances and dietician for the optimisation of diet. Diet : In cases with chronic fatiguing factors, nutrition can be become a vital aspect into the reparative process. This may include energy and mineral rich foods such as bananas, green leafy vegetables for iron and magnesium (200-300mg), oranges for vitamin C (anti-oxidant and helps with the absorption of iron), anti-oxidant rich foods such as EPA/DHA (1000mg) fish oil, curcumin (Tumeric), Cats Claw, Devils Claw, Chia seeds, fruits of the forest (berries), and CoQ10 with Vitamin B. Folate and Ferritin levels should also be checked. Calorific energy intake should balance with energy expenditure. However, as we are often dealing with young individuals, as in this case, some form of comfort food may be appropriate such as, nuts, legumes, homus and sushi. Protein intake prior to carbohydrate intake may help ameliorate any blood sugar fluctuations due to Glycemic Index factors, however simple carbohydrates (high GI) should be avoided wherever practical. Even oats need to be soaked overnight and cooked briefly, otherwise they become a high GI food and may even affect the absorption of iron. The type of rice used can also influence GI, hence the addition of protein such as fish. Protein supplementations are generally over-used. Daily protein intake should not exceed 1.2g per kg of body weight per day. Dosage for children is less than that for adults. See Nutritional Section of this Site Probiotics such as Sauerkraut should also be considered when dealing with potential immune disorders related to the gut. In this case IBS was a confounding variable in his presentation. The amount of human DNA is totally under-whelming compared to that of the intestinal mircobiome. The intestine is composed of a complex ecosystem of more than trillions of bacteria, viruses, fungi, Protozoa and Archea that live in a symbiosis with the host in the gut lumen. The healthy microbiome include a limited number of highly represented taxa, such as Bacteroides and Prevotella and a large number (>2000 to date) of minor players with low representation but high metabolic activity. These latter 'players' with high metabolic activity are likely to be the ones which interact with the musculoskeletal system. In older age, species richness and diversity of the microbiome decline, inter-individual variability increases, and resilience to perturbations are reduced. Apart from aging, the presence of acute and chronic diseases affects the microbiome. In the aging and/or unhealthy microbiome a 'dysbiosis' can occur, where a disruption of the gut balance 'symbiosis' results in intestinal permeability, allowing bacteria, or bacterial toxins and metabolites to enter the host circulation thereby promoting sub-clinical inflammation. Clinically, sub-clinical inflammation has been referred to as 'inflammaging' and 'immunosenescence'. Further research on metabolic immune reactions can be found elsewhere on this website. See https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-the-immune-system-during-covid-19.html#Diet Trunk muscles : Researchers have found that a history of SRC had an increased possibility of having altered size and contraction of their trunk muscles, including smaller multifidus, larger quadratus lumborum muscles, and asymmetrical contraction of their transverse abdominis muscles, whereby an increased thickness and resting tone of the right anteroloateral abdominal muscle has been observed (Hides et al 2017 Med Sc Sp Ex, 49, 12, 2385-2393). In this case, by the second incident (Basketball impact), the subject was 15 years of age and 193cm in height. Apart from being very tall for his age he also has joint hypermobility. Combinations of SRC, growth spurt and hypemobility may have had a greater impact on his motor performance making secondary trauma more likely? A 3-6 increased risk of future SRC has been reported in the literature in cases of concussion (Abrahams et al 2014, Br J sp Med, 48, 2, 91-97). In our subject, using the laser repositioning error described above, marked inability to reposition the neck from the left was seen. This concurs with the findings in Australian Football Players (AFL), where a mean of 4.5 degrees of joint position error was reported on the left hand side (Hides et al 2017 Med Sc Sp Ex, 49, 12, 2385-2393). This is noteworthy, as our subjects initial concussion took place during AFL, with the subsequent concussion occurring in Basketball. It should also be remembered that this subject presented to physiotherapy for an ankle injury some 6 months after the initial concussion. Lower limb kinematic exercising ability, emphasising global balance and kinematic 'inverse dynamics' muscular energy strap transfer principles, demonstrated strength and balance deficits within the following programme. Leaning forward, pivoting through the hip in exercise 2 and 3, will lead to better hamstring, gluteal and quadriceps engagement. The Sideways Lunge should only be down once the Reverse Lunge is perfected. The use of a slider on the floor and progressing from reverse lunge, to diagonally sideways lunge and eventually sideways lunge may need to proceed lunges with steps and certainly forward lunges. Aim, is to re-orient the motor learning systems to efficiency of movement both metabolically and mechanically. It should be noted that this regime places emphasis on repetitive loading; hence 3 x 40 reps. Interestingly, an investigation comparing lower limb (LL) and back exercises (lumbar extension LE and lumbar stabilisation LS) for runners with chronic low back pain reported greater improvement in self-rated running capability and knee extension strength in the LL group vs LE and LS groups greater increase in running step length in LL and LE groups and similar reductions in running induced pain and improvement in back muscles across all three exercise groups. (Cai et al 2018, Med Sc Sp EX, 49, 12, 2374-2384) Extrapolation of these results to the current clinical setting suggests the importance of lower limb dynamic stability in cases of concussion. Moreover, recognition of these deficits may have prevented the second incidence of concussion? Exercise and cognition Corpo Sano Mente Sana or a Healthy Mind in a Healthy Body, has been the mythical connection between brain and brawn. In terms of neurophysiology, the dopaminergic system has been attributed for the drive to exercise. Habitual exercisers have been shown to have been predicted to have greater prefrontal cortex (PFC) executive function. Investigators have found a link between 'blink rate' and cognitive function on STROOP testing and functional near-infrared spectroscopy (Kuwamizu R et al 2021, Med Sc Sp Ex, 53, 7, 1425-1433). Orienteering is a sport requiring high endurance physical fitness, agility and high cognitive function, as the task demands navigation, at speed, through unknown terrain. In terms of this clinical presentation, he commenced a programme of multi-day bushwalking/backpacking approximately 2 years after the initial concussion incident. Later, he participated in orienteering and rogaining events. Further reading on higher executive function, clinical reasoning and learning using orienteering as a construct can be found elsewhere on this website : https://www.back-in-business-physiotherapy.com/physiotherapy-teaching/constructivism.html Conclusion Investigations, into people with persisting PCS, demonstrated that they applied more force over time to control balance. Helmich et al (2016, Med Sc Ex Sp, 48, 12, 2362-2368) proposed that in regard to cognitive processes, the increase of cerebral activation indicates an increase of attention demanding processes during postural control in altered environments. This is relevant in so far as individuals with post concussive symptomatology have a variety of symptoms including headache, dizziness, and cognitive difficulties that usually resolve over a few days to weeks. However, a subgroup of patients can have persistent symptoms which last months and even years. Complications in differential diagnosis, can arise clinically, when neck dysfunction and altered motor control occur concurrently due to both neck and cerebral pathology. For example, Whiplash and other traumatic head and neck injuries can result in pathology to both regions, whereas, more discreet altered cognitive processing from concussion can result in altered neck motor control. Musculoskelatal Physiotherapy can play a vital part in the treatment of neck dysfunction including the re-establishment of occulomotor proprioception and managing localized strength and cardiovascular exercise regimes. A total body, multi-disciplinary approach which is well co-ordinated amongst practitioners is vital to an optimal outcome. Final Outcome In 2021, some 5 years after the initial concussion at the Sydney Swans Academy, his status was as follows 20 years of age never went back to AFL or any type of contact sport missed 1.5 years of school (2016 and 2017) did his matriculation year (2019) almost solo in the library after school, (where he also happened to meet his current girl friend) whilst using class time for revision. Dropped mathematics, as it was a subject which needed continuous learning and the gap of 1.5 years was too much to catch up on. Managed to get a top 10 result in the State for Geography and an overall ATAR of 97%. 5 years post concussion studying environmental science/law at Sydney University. Caught up on Calculus and Statistics during summer semesters at University taken up rock climbing, bouldering and surfing (2020). 3 - 4 years post concussion multi-day bushwalking in Tasmania, orienteering and rogaining still has some issues with concentration when fatigued avoids alcohol or anything else which he feels has an impact on his brain. still prone to hypermobility joint strain issues See link to repetitive linear head trauma (heading at soccer) for more information : https://www.back-in-business-physiotherapy.com/latest-news/264-repetitive-linear-head-trauma.html Updated : 23 July 2022. Original : 17 November 2017 Read More -

Pain in the Brain - neural plasticity
Pain in the Brain and Neural Plasticity by Martin Krause There are several mechanisms that can create a sensation of pain, which has been described as 'an unpleasant sensory and emotional experience in response to perceived or potential tissue damage'. Pain can be the result of peripheral sensitisation from peripheral inflammation, vascular compromise, necrosis, swelling, etc. Importantly, higher centres of the central nervous system not only perceive such sensitization of the peripheral nerve receptors, they can also modulate and control the intensity and tolerability of the perceived sensation through descending modulation at the peripheral receptor and in the spinal cord and through transcortical mechanisms depending on the 'meaning' and 'context given to the pain. Moreover, the higher centres can create a 'state' of perceived 'threat' to the body through emotions such as fear and anxiety. Rather than the brain acting as a filter of unwanted sensation, in the higher centre induced pain state, rumination and magnification of sensations occur to create a pathological state. Paradoxically, representation of body parts such as limbs and individual muscles can reduce in perceived size. In such instances the pain doesn't represent the sensation of pathology but rather pain has become the pathology. Hence, the brain generates pain in the brain, where the pain is perceived to be some sort of non-existent inflammatory or pathological sensation in the periphery. Evidence for this neural plasticity comes from imaging studies, where brain white matter structural properties have been shown to predict transition to chronic pain (Mansour et al 2013, Pain, 154, 10, 2160-2168). Specifically, differential structural connectivity to medial vs lateral prefrontal cortex and connectivity between medial prefrontal cortex and nucleus accumbens has been shown in people with persistent low back pain. In this case the back pain becomes the inciting event and given the persons' structural propensity, establishes specific functional connectivity strength. Some of these changes, in the neural architecture, might be explained by the fact that roughly 5000 of our 20000 genes which make up the human genome are dedicated to chronic pain further reading Peripheral input is a powerful driver to neuroplasticity. Information gathered by touch, movement and vision, in the context of pain can lead to mal-adaptive plasticity, including the reorganisation of the somatosensory, and motor cortices, altered cortical excitability and central sensitisation. Examples of somatosensory reorganisation come from the work of Abrahao Baptista when investigating chronic anterior knee pain, who not only demonstrated reduced volume of Vastus Medialis but also is cortical translocation to another part of the cortex. Individuals with patellofemoral pain (PFP) had reduced map volumes and an anterior shift in the M1 representations, greater overlap of the M1 representation and a reduction in cortical peaks across all three quadriceps (RF, VL, VMO) muscles compared with controls.(Te et al 2017 Pain Medicine, pnx036, https://doi.org/10.1093/pm/pnx036) AKP = anterior knee pain The same researcher (Abrahao Baptista) has shown that maximal tolerable electrical stimulation (eg TENS) of muscles can induce normalisation of the cortical changes through a process called 'smudging'. Transcortical stimulation has also been applied as a cortical 'primer' prior to the application of more traditional therapy such as motor re-training, exercise, and manipulation. The altered muscle activation around the knee may lead to altered inverse dynamics, energy dissipation and propagation, leading to increased risk of knee osteoarthritis. An increase in just 1% baseline knee adduction moment has been associated with a six-fold increase risk of radiographic progression of knee osteoarthrits in a 6 year follow up study (Miyazaki et al 2002, Ann Rheum Dis, 61, 7, 617-22). Brain White Matter microstructure of people with Lateral Ankle Sprain Lateral ankle sprains occur in approximately 70% of the population. These can become chronic and quite disabling leading to declines in physical activity and its concomitant morbidity. Additionally, in the elderly, this can lead to an increased risk of fractures due to falls. Ruptured ligaments have the capacity to alter the somatosensory input to the cortices, thereby altering in turn, the afferent input from the cortices to the periphery, as evidenced by increased use of hip musculature (Doberty et al 2015, Clin Biomech, 30: 129-135), over-reliance of visual input (Song et al 2017, J Sci Med Sport, 20, 10, 910-914) and the frequent use of external stabilisers such as braces and ankle supporting footware. Speculation of pyramidal grey matter changes in the motor cortices have also been made (Terada et al 2016, PM R, 8, 11, 1090-1096). Such altered mechanics has been associated with changes in the central nervous system microstructure of the white matter in the superior cerebellar peduncle (Terada et al 2019, Med Sc Sp Ex, 51, 4, 640-646). Cause and effect cannot be established, however, clinically, emphasis must be placed on both peripheral tissue issues as well as higher centre processes if the chronic cycle is to be broken. Motor strategies learned during pain are sustained upon pain-free re-exposure to task. Adaptations to pain can interfere with movement planning and execution. Researchers have investigated the influence of pain on shoulder and elbow muscle activity during pain and subsequently after the resolution of experimentally induced muscle pain. They found that the same strategy of reduced muscle activation and reduced co-contraction occurred on subsequent pain-free re-exposure to the task (Solomoni et al 2019 Med Sc Sp Ex, 51, 11, 2334-2343). Furthermore, task accuracy was achieved through a concomitant reduction in antagonist muscle activity. Reduced EMG activity was attributed to reduced central neurological drive from higher cortical centres. Although a reduction in muscle activity may seem like a better 'economy' of movement, it places the joints at risk, as the normal, really important, stabilising mechanism during initial learning, of a novel motor task, is compromised. Physiotherapeutic Treatment Body illusions are another novel way to promote the normalisation of cortical function through adaptive neuroplasticity. Examples come from people with hand arthritis, whose perception of their hand size is underestimated (Gilpin et al 2015 Rheumatology, 54, 4, 678-682). Using a curved mirror, similar to that in theme parks, the visual input can be increased to perceive the body part as larger (Preston et al 2011 DOI: 10.1093/rheumatology/ker104 · Source:PubMed ) . Irrespective of size, watching a reflection of the hand while performing synchronised movements enhances the embodiment of the reflection of the hand (Whitkopf et al 2017, Exp Brain res, 23, 5, 1933-1944). These visual inputs are thought to affect the altered functional connectivity between areas of the brain thereby affecting the 'pain matrix'. Another, novel way of looking at movement and pain perception is the concept of the motor engram. This has been defined as motor skill acquisition through the modification and organisation of muscle synergies into effective movement sequences. The learning process is thought to be acquired as a child through experientially based play activity. The specific neural mechanisms involved are unknown, however they are thought to include motor map topography reflecting the capacity for skilled movement reorganisation of motor maps in a manner that reflects the kinematics of acquired skilled movement map plasticity is supported by a reorganisation of cortical micro-circuitry involving changes in synaptic efficacy motor map integrity and topography are influenced by various neurochemical signals that coordinate changes in cortical circuitry to encode motor experience (Monfils 2005 Neuroscientist, 11, 5, 471-483). Interestingly, it is an intriguing notion that accessing motor engrams from patterns acquired prior to the pain experience might lead a normalisation of brain activity. My personal experience of severe sciatica with leg pain, sleepless nights and a SLR of less than 30 degrees, happened to coincide with training my 9 year old sons soccer training. I was noticing that the nights after i trained the children, I slept much better and my range of movement improved. I commenced a daily program of soccer ball tricks which i had been showing the kids, including 'juggling', 'rainbows' and 'around the worlds'. Eventually, I even took up playing soccer again after a 30 year absence from the sport. Other than new activity related pain issues (DOMS), four years on, the sciatica hasn't returned. I can only conclude that this activity activated dormant childhood motor engram, worked on global balance, mobilised my nerve, encouraged cross cortical activity and turned my focus into functional improvement. Further explanations for my experience comes from evidence suggesting that a peripheral adaptive pain state is initiated, whereby transcortical inhibition occurs by the contralateral hemisphere to the one which controls the affected limb. Additionally, excitation cortical (M1) drive of the muscles of the contralateral limb to the one which is in pain also occurs. In such cases re-establishment of motor drive to the affected side is important. In terms of tendon rehabilitation, external auditory and visual cues using a metronome have been employed and are showing promising results (Ebonie Rio et al 2017 Personal communication). In terms of my experience with the soccer ball tricks, the external visual cues and the cross talk from using left and right feet, head, shoulders, and chest during ball juggling manoeuvres, whilst calling the rhythm to the kids may have been the crucial factor to overcome the dysfunctional brain induced pain - muscle inco-ordination cycle, which I was in. Additionally, I was cycling which allowed me to focus on motor drive into the affected limb. However, work by Lorrimer Moseley on CRPS has established that 'brain laterality' must be established before commencing trans-cortical rehabilitation techniques. Lorrimer's clinical interventions use 'mirror imaging' techniques which are only effective once the patient is able to discriminate the left and right sides of the affected body parts, presented visually, in various twists and angles. Alternatively, the altered pain state can result in a hostage like situation, whereby the pain takes control. Similar to the 'Stockholm Syndrome' where the hostage begins to sympathise with their captors, so do some peoples brain states, where it begin to sympathise with the pain, creating an intractable bondage and dysfunctional state. One screening question which may reflect commitment to the process of rehabilitation is to question whether they were able to resist the cookie jar when they were a child? Or were they committed to any sporting endeavours as a child? This may give some indication for the presence of motor engrams which can be used to overcome dysfunctional pain induced muscle synergies (neurotags), but also indicate an ability to be self disciplined, as well as being able to reconcile and identify goal oriented objectives, in spite of the cognitive pain processes? Remember that neurons that fire together, wire together. Uploaded : 4 June 2019 Updated : 18 July 2021 Read More -
Sickle Cell Trait and Acute Low Back Pain
Researchers believe that lumbar paraspinal myonecrosis (LPSMN) may contribute to the uncommon paraspinal compartment syndrome and that sickle cell trait (SCT) may play a role. Sustained, intense exertion of these lumbar paraspinal muscles can acutely increase muscle size and compartment pressure and so decrease arterial perfusion pressure. This same exertion can evoke diverse metabolic forces that in concert can lead to sickling in SCT that can compromise perfusion in the microvasculature of working muscles. In this manner, they believe that SCT may represent an additional risk factor for LPSMN. Accordingly, they presented six cases of LPSMN in elite African American football players with SCT. See link below http://journals.lww.com/acsm-msse/Fulltext/2017/04000/Acute_Lumbar_Paraspinal_Myonecrosis_in_Football.1.aspx Read More -
Ibuprofen, Resistance Training, Bone Density
Taking Ibuprofen immediately after resistance training has a deleterious effect on bone mineral content at the distal radius, whereas taking Ibuprofen or undertaking resistance training individually prevented bone mineral loss. http://journals.lww.com/acsm-msse/Fulltext/2017/04000/Effects_of_Ibuprofen_and_Resistance_Training_on.2.aspx Read More -

Mitochondrial Health and Sarcopenia
The mitochondria is the 'powerhouse' of the cell. It's DNA is derived from the female side of the genetic inheritance. They exist in two areas of muscle - beneath the sarcolemmal membrane and in the intermyofibrillar region. Together they form the mitochondrial reticulum. Two processes exist, fusion and fission. Fusion of the inner membrane (IM) results in expanding and elongating the mitochondrial reticulum, with more complex and extensive morphologies associated with healthy, exercise trained individuals. Functionally, this allows greater metabolic flexibility, lipid metabolism and greater distribution of mtDNA and metabolites throughout the reticulum. In contrast, fission involves removing portions of the reticulum which have become dysfunctional, limiting the affects of toxic by-products such as ROS (reactive oxygen species), or mtDNA mutations. Structurally, the IM has varying degrees of internal folding, known as cristae, whose surface area determines the effectiveness of the electron transport chain (ETC). Cristae density is often an indication of mitochondrial quality, characterised by exercised individuals. Ageing After the age of 30 results in a 10% reduction in aerobic capacity each decade. Whereas, after the age of 40, a 1% reduction of strength occurs annually, which accelerates in the 6th decade of life with inactivity. The latter is known as sarcopenia. The ageing process (AKA 30 years of age onwards), in the presence of high ROS (reactive oxygen species) and/or damaged mitochondrial DNA, can induce widespread mitochondrial dysfunction. In the healthy cell, mitophagy results in the removal of dysfunctional mitochondria and related material. In the absence of functional removal of unwanted mitochondrial material, a retrograde and anterograde signalling process is potentially instigated, which results in both motor neuronal and muscle fibre apoptosis (death) (Alway, Mohamed, Myers 2017, Ex Sp Sc Rev, 45, 2, 58-69). This process is irreversible. Investigations in healthy populations, have shown that regular exercise improves the ability to cope with regular oxidative stress by the buffering and 'mopping up' of ROS agents which are induced as a result of exercise. It is plausible and highly probable that regular exercise, throughout life, can mitigate against muscle fibre death (Sarcopenia). Importantly, this process of muscle fibre death can commence in the 4th decade of life, and be as much as 1% per year. Reduction of muscle mass can result in immune and metabolic compromise, including subclinical inflammation, type II diabetes as well as the obvious reduction in functional capacity for activities of daily living. Exercise is muscle mitochondrial medicine during ageing An elevation in the proportion of dysfunctional mitochondria within muscle with age could be a consequence of reduced biogenesis or impaired removal via mitophargy. The stability of the precursor proteins in the cytosol is reduced in aged muscle, thus providing less substrate for biogenesis. Lysomal dysfunction and the inability to remove damaged organelles and other deficits are reversed through exercise. A review by Oliviera An et al (2021 Ex Sp Sc Rev, 49, 2, 67-76) considered exercise at a potent therapeutic modality through the stimulation of mitochondrial biogenesis through a key regulator PCG-1aplha, as well as a potent stimulator of mitophagy, whereby damaged mitochondria are removed from the reticulum. Ageing, in the presence of disuse, is known to induce poor muscle oxidative status and metabolic inflexibility. For example, chronic contractile activity (CCA) reverses accelerated ROS production, evident in aged muscle, and increases transcription of PGC-1alpha toward levels found in younger individuals. Additionally, exercise has been shown to increase lysosomal content irrespective of age. Mitophagy flux elevated with age is reduced with exercise. Mitochondria are highly dynamic, interconnected organelles that continuously undergo events of renewal, removal and reorganization. The balance between biogenesis and mitophagy determines 'turn over' and hence the quality and quantity of mitochondria. In the absence of exercise, fission-fusion regulatory imbalances occur. Exercise pre-conditioning Exercise preconditioning is used to describe exercise induced changes before a period of inactivity, which serves to protect the skeletal muscle against atrophy and dysfunction through disuse. This protection is achieved through increased cytosolic and mitochondrial antioxidants and chaperones increasing mitochondrial gene expression and protein levels reduced signalling toward apoptotic and atrophy pathways Optimal approach to load progression during strength training in older adults Three dominant approaches exist to progression and exercise training perceived exertion (RPE) target repetitions (incl. repetitions to failure (RM), repetitions in reserve (RiR) % of maximum (%1RM) It has been established that repetitions to failure for sports specific training is highly effective in some populations, however in older adults it may induce DOMS or worse still function-limiting-injuries. Older peoples perception of exercise are among the major determinants whether a person will continue their exercise program. Too slow progression or too little load can be as unmotivating as an injury from repetitions to failure. Lower intensities may lead to higher adherence rates and feelings of pleasure. But what is too little and too much? Buskard et al (2019, Med Sc Sp Ex, 51, 11, 2224-2233) determined that all forms of progressive exercise improved muscular strength and functional capacity. Moreover the RPE method was significantly more tolerable and enjoyable than the RM, RiR, and %1RM methods. However, this may only hold true for the first 6 months of a training regime, after which time, the individual has become accustomed to the routine of exercise and hence may perceive greater loads as more beneficial with reduced side effects. The latter is speculative but anecdotally appears to be true in some sub-populations involved in competitive exercise. See : Sarcopenia and Aging Use of chaos theory to load progression and immune integrity during COVID-19 Since the onset of COVID-19 many of us have asked why are there so few antivirals? The answer boils down to biology, and specifically the fact viruses use our own cells to multiply. This makes it hard to kill viruses without killing our own cells in the process. So how do we ensure cell survival, whilst priming the immune system to make antigens for its defence system. What does this even mean? Can exercise be an answer to reduce the extent of our immune response if exposed to COVID-19? Will knowing why exercise is good for our immune system motivate people to exercise more? During this time of crisis, we've been told to exercise. Exercise for physical and mental well-being. Whether in partial 'lock down' or 'full lock down' or 'opening up', exercise is still important. But Why? How do chaos theory and non-linear dynamics explain movement and the immune system? We were born from the chaotic fire of genesis. Laws of thermodynamics dictate our existence. Evolution of heat shock proteins (HSP) means that we are our immune system. Today, human multi-cellular life is still totally dependent on our unicellular ancestors and their components. Trillions of species and bacteria in the gut (flora) and skin alone, associated with immune substances, attest to the importance of unicellular life in the immune system. The abundance of energy species in the gut suggests a nexus with one of the organs most in need of energy, the skeletal muscle. Importantly, muscle cells have more mitochondria than most other cells, so they can readily produce work for movement. Consequently, muscles are an energy system and an immune endocrine organ. Notably, the development from unicellular to multi-cellular life needed movement. A commonality of cellular movement and macro-muscular movements exist. Physiotherapeutic and training interventions must consider the health of the immune system and its ability to deploy and be re-deployed. Training should avoid becoming 'stale' by having enough variety (chaos) to create perturbations in the immune system which induce up and down regulation of immune components. Physiotherapy should be innovative and creative, whereby the physiotherapist additionally considers immune-cognitive aspects of pain and inflammation, when people seek physiotherapeutic intervention after/during a change in their training regime and/or commencement of unaccustomed exercise, or in the presence of immune compromise. Elsewhere, a synopsis of my past research in the field of biomechanics, pathomechanics, neurophysiology, cognition, immunology, sarcopenia and my current interest in chaos, can be found reading Aging, COVID-19, Chaos, Exercise and the Immune System p53 and anti-carcinogenic protein deficits p53 is considered a tumour suppressor protein and drives cellular apoptosis and DNA damage/repair. p53 may also have important functions for basal mitochondrial content and function, whilst the effects of it's reduction or absence, on the mitochondria, has been shown to be reversed with exercise(Oliveira AN 2021, Ex Sp Sc Rev, 49, 2, 67-76) Published 11 July 2017 Updated : 7 February 2022 Read More -

Ehlers Danlos Syndrome
Is your child suffering Ehlers Danlos Syndrome? Hypermobile joints, frequent bruising, recurrent sprains and pains? Although a difficult manifestation to treat, physiotherapy can help. Joint Hypermobility Syndrome (JHS) by Martin Krause B.Appl.Sci. (Physiotherapy); M.Appl.Sci (Manipulative Physiotherapy), Post Grad Dip Hlth Sc (Exercise and Sports), Post Grad Cert Hlth Sc (Education) When joint hypermobility coexists with arthralgias in >4 joints or other signs of connective tissue disorder (CTD), it is termed Joint Hypermobility Syndrome (JHS). This includes conditions such as Marfan's Syndrome and Ehlers-Danlos Syndrome and Osteogenesis imperfecta. These people are thought to have a higher proportion of type III to type I collagen, where type I collagen exhibits highly organised fibres resulting in high tensile strength, whereas type III collagen fibres are much more extensible, disorganised and occurring primarily in organs such as the gut, skin and blood vessels. The predominant presenting complaint is widespread pain lasting from a day to decades. Additional symptoms associated with joints, such as stiffness, 'feeling like a 90 year old', clicking, clunking, popping, subluxations, dislocations, instability, feeling that the joints are vulnerable, as well as symptoms affecting other tissue such as paraesthesia, tiredness, faintness, feeling unwell and suffering flu-like symptoms. Autonomic nervous system dysfunction in the form of 'dysautonomia' frequently occur. Broad paper like scars appear in the skin where wounds have healed. Other extra-articular manifestations include ocular ptosis, varicose veins, Raynauds phenomenon, neuropathies, tarsal and carpal tunnel syndrome, alterations in neuromuscular reflex action, development motor co-ordination delay (DCD), fibromyalgia, low bone density, anxiety and panic states and depression. Age, sex and gender play a role in presentation as it appears more common in African and Asian females with a prevalence rate of between 5% and 25% . Despite this relatively high prevalence, JHS continues to be under-recognised, poorly understood and inadequately managed (Simmonds & Kerr, Manual Therapy, 2007, 12, 298-309). In my clinical experience, these people tend to move fast, rely on inertia for stability, have long muscles creating large degrees of freedom and potential kinetic energy, resembling ballistic 'floppies', and are either highly coordinated or clumsy. Stabilisation strategies consist of fast movements using large muscle groups. They tend to activities such as swimming, yoga, gymnastics, sprinting, strikers at soccer. Treatment Treatment has consisted of soft tissue techniques similar to those used in fibromyalgia, including but not limited to, dry needling, myofascial release and trigger point massage, kinesiotape, strapping for stability in sporting endeavours, pressure garment use such as SKINS, BSc, 2XU, venous stockings. Effectiveness of massage has been shown to be useful in people suffering from chronic fatigue syndrome (Njjs et al 2006, Man Ther, 11, 187-91), a condition displaying several clinical similarities to people suffering from EDS-HT. Specific exercise regimes more attuned to co-ordination and stability (proprioception) than to excessive non-stabilising stretching. A multi-modal approach including muscle energy techniques, dry needling, mobilisations with movement (Mulligans), thoracic ring relocations (especially good with autonomic symptoms), hydrotherapy, herbal supplementation such as Devils Claw, Cats Claw, Curcumin and Green Tee can all be useful in the management of this condition. Additionally, Arnica cream can also be used for bruising. Encouragement of non-weight bearing endurance activities such as swimming, and cycling to stimulate the endurance red muscle fibres over the ballistic white muscles fibres, since the latter are preferably used in this movement population. End of range movements are either avoided or done with care where stability is emphasised over mobility. People frequently complain of subluxation and dislocating knee caps and shoulders whilst undertaking a spectrum of activities from sleeping to sporting endeavours. A good friend of mine, Brazilian Physiotherapist and Researcher, Dr Abrahao Baptista, has used muscle electrical stimulation on knees and shoulders to retrain the brain to enhance muscular cortical representation which reduce the incidence of subluxations and dislocations. Abrahao wrote : "my daughter has a mild EDS III and used to dislocate her shoulder many times during sleeping. I tried many alternatives with her, including strengthening exercises and education to prevent bad postures before sleeping (e.g. positioning her arm over her head). What we found to really help her was electrostimulation of the supraspinatus and posterior deltoid. I followed the ideas of some works from Michael Ridding and others (Clinical Neurophysiology, 112, 1461-1469, 2001; Exp Brain Research, 143, 342-349 ,2002), which show that 30Hz electrostim, provoking mild muscle contractions for 45' leads to increased excitability of the muscle representation in the brain (at the primary motor cortex). Stimulation of the supraspinatus and deltoid is an old technique to hemiplegic painful shoulder, but used with a little different parameters. Previous studies showed that this type of stimulation increases brain excitability for 3 days, and so we used two times a week, for two weeks. After that, her dislocations improved a lot. It is important to note that, during stimulation, you have to clearly see the humerus head going up to the glenoid fossa" Yoga vs Pilates Many hyper-mobile people love yoga. They are good at it. However, they could be pushing themselves from a fine line of hyper-mobility to functional instability, pain and muscle spasms. The latter feeling of stiffness, drives them to do more yoga, ultimately perpetuating a vicious cycle which could ultimately end with chronic neurogenic pain. The reality is that hyper-flexible people should choose a more gentle form of yoga and consider a form which encourages stability. Other disciplines may be more appropriate such as Pilates or more specific stabilising physiotherapeutic exercises, involving isometric contractions, oscillations and balance. Alternatively, mind-body holistic approaches such as Feldenkreis and Alexander technique may be more appropriate. The mere elongation of the upper neck, in Alexander technique, activates the pelvic floor, deep core, diaphragm and shoulder blade stabilisers. Marathon vs Sprinting Comparing a marathon runner with a sprinter is like comparing an African Wild Dog with a Springbok. The former has the ability to run for days, whereas the latter has the fastest speed of any animal on earth. You will very rarely find a 'floppy' lined up at the start of a marathon. They like to sprint and are frequently good at other ballistic activities such as high jump, pole volt, gymnastics. The 'stiffy' on the other hand loves the marathon as their stiffness stabilises them. Hence, 'floppies' need to stabilise. The stabilising muscles are the deepest layered ones, those which frequently only cross one joint and cannot easily be touched. Non-impact endurance exercise should therefore be encouraged. Sports such as swimming and cycling encapsulate this. However, even here, shoulder impingement needs to be avoided, whilst swimming (hydrotherapy), with good shoulder blade and core stability. Hydrotherapy conditioning can be practice out of water with a Swiss Ball and with Theraband exercises. Cyclists may develop knee, back and neck pain so they need to do a lot of gluteal and hamstring training in a closed kinetic chain e.g. reverse lunges for the knee, and should - shoulder blade - neck and back exercises for the upper body postures. Endurance exercise may also help calm the autonomic sympathetic nervous system, which is often seen as dysfunctional in people with EDS. Postural Orthostatic Tachycardia Syndrome (POTS) is frequently found amongst people with hypermobility. It is essentially an imbalance between heart rate and blood pressure which affects cardiac output (= SV x HR). The Modified Dallas POTS Exercise Program can be found here, which describes a progressive 4-6 month exercise program. Rock climbers are frequently hypermobile people. Clinically, I've found hypermobile people prefer to pull rather than push. They are pulling energy in towards themselves creating a stabilising force. However, they seem, initially, to gain a lot from yoga, where a lot of pushing stabilisation work can occur in positions such as high plank, down-facing dog, etc. However, too much of a good thing can become a bad thing. Stabilisation, without the aim of gaining range of movement, but rather, controlling range of movement should be the objective. Muscle synergies can play a very important role, where a group of muscles from the legs to the arms can be stabilising, whilst one limb is moving, the others are dynamically or statically stabilising. The classic three points of contact in rock climbing. Interested readers should look at the climbing section of this website for further information. There are links to exercises, concepts of shoulder and shoulder blade-thorax stability, as well as hip-pelvic-back stability. Agility vs Clumsiness and Deterministic Chaos Hyper-mobile people tend to be either highly coordinated or clumsy. There doesn't appear to be a middle ground. I therefore like people to use exercises which either are isometric, pull energy towards them (pull up vs a push up), and use oscillations. These oscillations or periodicities are able to encourage movement around a fixed point based on visio-spatial (eyes), cerebro-vestibular (ears), and musculoskeletal inflection points. These inflection points can be the therapeutic building block of all movements. It needs to be remembered that when the (chronically) injured person comes to you, if they once were a 'great' athlete (which is very common), they had learnt to move outside of the 'average' movement system. Their brains are still tuned to those fundamentals, but are now over-ridden by the 'static' of pain generator input! Those movement patterns of a prior pre-injured life are still somewhere to be found. Like peeling back the layers of an onion to disseminate what is what, and the rebuilding the system. However, it should be remembered, that those movement patterns were born of fast controlled->uncontrolled movement. These 'outliers' are essentially what 'deterministic chaos' encapsulates. Ultimately, only oscillatory balancing movements, based on a solid isometric gluteal base, can achieve achieve redemption. Activation of gluteal muscles results in the activation of the core, not vice versa!!!! Activation of the gluteal muscles also improves arm strength. Exercises - draw energy into the body to stabilise People need to use their muscle synergies to support the skeletal structures, not the other way round. Muscles support bones and organs, bones don't support muscles, they act as levers for the muscles. Consider the body to be lying in 'slings of muscles', similar to when you lie in a hammock. These slings are known as the front/anterior, back/posterior (x's 2, 3, 4, 5 and 8), inside/medial and outside/lateral (x's 1 and 6), as well as spiral slings. The following exercises are designed to invoke the muscle bellies in the loading mechanism. The strain should be felt within them, not at the joints. The joints are just the axels around which movement occurs. Basically, hyperflexible people should avoid the tendency to hyperextend/flex their joints, and nullify the habit of overloading their tendon, ligament and joint surfaces. In X's 2 try to go back and diagonally back whilst keeping the knee over the ankle and dropping the stance hip down. There should be no pressure in the knee. All the pressure should be in the butt, hamstrings and quads in the upper 2/3rds of the thigh. Similarly in X's 3 lean forward enough so that you experience the butt, upper quads and hammies doing the work, with no pressure in the knee. Back X's - posterior sling : 7, anterior - posterior sling : 6, spiral : 7, medial and lateral and anterior : 11 (add Buttock clenches and you get posterior as well) Spiral : 12, 13 and 15, Lateral and Posterior : 14, Anterior : 17 Medial : 22, Anterior : 20, Posterior : 21 Shoulder Blade stabilisers Immune system People with hypermobility may also have an auto-immune disorder. Ironically, some hyper-mobile children develop severe stiffness later in life as a result of sero-negative arthropathies such as Ankylosing Spondylitis and Psoaratic Arthritis. The latter frequently is associated with scaly inflamed skin. Additionally, irritable bowel syndrome may also occur. The gut is known to be essential to immune health, where an imbalance can lead to several dysfunctional immune-inflammatory interactions. See : Trends in Microbiology, Moya and Ferrer: “Functional Redundancy-Induced Stability of Gut Microbiota Subjected to Disturbance” http://dx.doi.org/10.1016/j.tim.2016.02.002 Additionally, energy species of the gut interact with skeletal muscle. Skeletal muscles, not only allow us to perform movement and work, they are also an important immune endocrine organ. Surgery : The effect of surgical intervention has been shown to be favourable in only a limited percentage of patients (33.9% Rombaut et al 2011, Arch Phys Med Rehab, 92, 1106-1112). Three basic problems arise. First, tissues are less robust; Second, blood vessel fragility can cause technical problems in wound closure; Third, healing is often delayed and may remain incomplete. Voluntary Posterior Shoulder Subluxation : Clinical Presentation A 27 year old male presented with a history of posterior shoulder weakness, characterised by severe fatigue and heaviness when 'working out' at the gym. His usual routine was one which involved sets of 15 repetitions, hence endurance oriented rather than power oriented. He described major problems when trying to execute bench presses and Japanese style push ups. https://youtu.be/4rj-4TWogFU In a comprehensive review of 300 articles on shoulder instability, Heller et al. (Heller, K. D., J. Forst, R. Forst, and B. Cohen. Posterior dislocation of the shoulder: recommendations for a classification. Arch. Orthop. Trauma Surg. 113:228-231, 1994) concluded that posterior dislocation constitutes only 2.1% of all shoulder dislocations. The differential diagnosis in patients with posterior instability of the shoulder includes traumatic posterior instability, atraumatic posterior instability, voluntary posterior instability, and posterior instability associated with multidirectional instability. Laxity testing was performed with a posterior draw sign. The laxity was graded with a modified Hawkins scale : grade I, humeral head displacement that locks out beyond the glenoid rim; grade II, humeral displacement that is over the glenoid rim but is easily reducible; and grade III, humeral head displacement that locks out beyond the glenoid rim. This client had grade III laxity in both shoulders. A sulcus sign test was performed on both shoulders and graded to commonly accepted grading scales: grade I, a depression <1cm: grade 2, between 1.5 and 2cm; and grade 3, a depression > 2cm. The client had a grade 3 sulcus sign bilaterally regardless if the arm was in neutral or external rotation. The client met the criteria of Carter and Wilkinson for generalized liagmentous laxity by exhibiting hyperextension of both elbows > 10º, genu recurvatum of both knees > 19º, and the ability to touch his thumb to his forearm Headaches Jacome (1999, Cephalagia, 19, 791-796) reported that migraine headaches occurred in 11/18 patients with EDS. Hakim et al (2004, Rheumatology, 43, 1194-1195) found 40% of 170 patients with EDS-HT/JHS had previously been diagnosed with migraine compared with 20% of the control population. in addition, the frequency of migraine attacks was 1.7 times increased and the headache related disability was 3.0 times greater in migraineurs with EDS-HT/JHS as compared to controls with migraine (Bendick et al 2011, Cephalgia, 31, 603-613). People suffering from soft tissue hypermobility, connective tissue disorder, Marfans Syndrome, and Ehler Danlos syndrome may be predisposed to upper cervical spine instability. Dural laxity, vascular irregularities and ligamentous laxity with or without Arnold Chiari Malformations may be accompanied by symptoms of intracranial hypotension, POTS (postural orthostatic tachycardia syndrome), dysautonomia, suboccipital "Coat Hanger" headaches (Martin & Neilson 2014 Headaches, September, 1403-1411). Scoliosis and spondylolisthesis occurs in 63% and 6-15% of patients with Marfans syndrome respectively (Sponseller et al 1995, JBJS Am, 77, 867-876). These manifestations need to be borne in mind as not all upper cervical spine instabilities are the result of trauma. Clinically, serious neurological complications can arise in the presence of upper cervical spine instability, including a stroke or even death. Additionally, vertebral artery and even carotid artery dissections have been reported during and after chiropractic manipulation. Added caution may be needed after Whiplash type injuries. The clinician needs to be aware of this possibility in the presence of these symptoms, assess upper cervical joint hypermobility with manual therapy techniques and treat appropriately, including exercises to improve the control of musculature around the cervical and thoracic spine. Atlanto-axial instability can be diagnosed by flexion/extension X-rays or MRI's, but is best evaluated by using rotational 3D CT scanning. Surgical intervention is sometimes necessary. Concussion Severity of concussion has been associated with JHS. An interesting case of EDS and it's affect on post concussion syndrome can be read elsewhere on this site. Temperomandibular Joint (TMJ) Disorders The prevalence of TMJ disorders have been reported to be as high as 80% in people with JHD (Kavucu et al 2006, Rheum Int., 26, 257-260). Joint clicking of the TMJ was 1.7 times more likely in JHD than in controls (Hirsch et al 2008, Eur J Oral Sci, 116, 525-539). Headaches associated with TMJ disorders tend to be in the temporal/masseter (side of head) region. TMJ issues increase in prevalence in the presence of both migraine and chronic daily headache (Goncalves et al 2011, Clin J Pain, 27, 611-615). I've treated a colleague who spontaneously dislocated her jaw whilst yawning at work one morning. stressful for me and her! Generally, people with JHD have increased jaw opening (>40mm from upper to lower incisors). Conclusion EDS and JHS are complex, multi-factorial debilitating conditions, which frequently, for many years, are misdiagnosed. Therapeutic intervention will depend upon the stage, stability, irritability and severity of the disease, Issues such as misuse, abuse, overuse and disuse will also need to be entertained. Regardless, a multi-modal approach to a multidimensional problem needs to be considered. Importantly, the individual must be engaged in every stage of the treatment intervention process. Updated 28 October 2022 Read More -

Physiotherapy with Sharna Hinchliff
Physiotherapy with Sharna Hinchliff Martin was pleased to welcome the very experienced physiotherapist Sharna Hinchliff to Back in Business Physiotherapy, for one on one physiotherapy sessions with clients, in 2017. Sharna is a passionate triathlete and mother and has had several years experience working locally and internationally (New York and London) in the field of physiotherapy. Originally from Western Australia, Sharna graduated from the world renowned Masters of Manipulative Physiotherapy at Curtin University. Sharna is fully vaccinated for COVID-19 (with Pfizer) since June 2021. read more Read More
No Articles for this News Feed.